Latest videos
Open heart (coronary artery bypass, or CABG) surgery is performed in order to reroute, or "bypass," blood around blocked arteries, thereby improving the supply of oxygen-rich blood to the heart. Surgeons usually use an artery from the chest wall to construct the "detour" around the blocked part of the artery. Veins from the legs are also used.

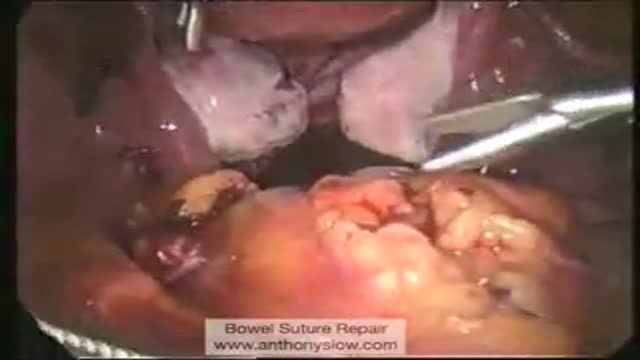
This video demonstrates the approach to a large base of tongue tumor, which was invading the ramus of the mandible. The procedure, named after Dr. Trotter, is really a median labiomandibuloglossotomy. In this case this poorly differentiated tumor was resected along with a portion of the floor of mouth. The entire area was reconstructed with a pectoralis major myocutaneous flap.

In PRK the epithelium (top layer of the cornea) is scraped off and then the laser treatment is applied. A contact lens is used as a "bandage" to decrease discomfort. The epithelium then grows back over the bare area during the next few days.
In LASEK the epithelium is exposed to 20% alcohol which helps separate epithelium from the cornea. The epithelium is pushed to one side and laser treatment applied. The epithelial layer is replaced back onto the eye and held in place with a contact lens. The contact lens is then removed a few days later. LASEK is hence a "no knife"/flap operation.
Epi-Lasik is a similar procedure that uses a keratome like that used for Lasik, but engineered to only separate the epithelium. The epithelium is left on a hinge, laser treatment applied and flap replaced.

This procedure describes one of the most versatile approaches to the anterior skull base for large tumors of the sinonasal cavity. It may be used with or without a craniofacial resection. The benefits of this approach are: wide access around the tumor; good postoperative cosmesis; & decreased operative & postoperative morbidity. We have used this approach for many bilateral tumors of the nasal & sinus cavities that approach &/or invade the skull base & brain. This video show the resection of a large esthesioneuroblastoma.