Pinakabagong mga video
Examination of varicose veins
varicose vein surgery stab and avulsion technique
How to perform a lumbar puncture.
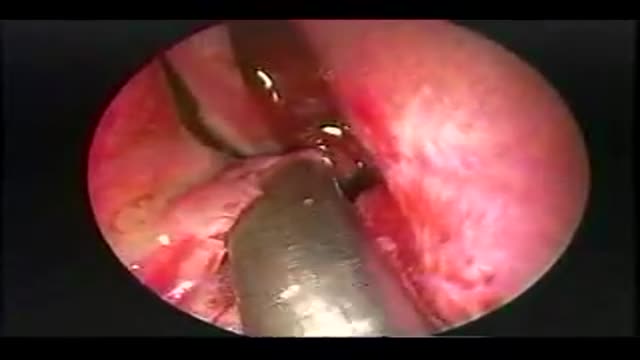
Dr. Jawad has been performing Bariatric Surgery in Central Florida since 1984, and Laparoscopic Bariatric Surgery since 1999, having completed over 2000 Bariatric Surgical Cases safely, and with great success. Here you can watch Dr. Jawad performing a Laparoscopic Adjustable Gastric Band procedure, with audio commentary describing the procedure.
Dr. Jawad has been performing Bariatric Surgery in Central Florida since 1984, and Laparoscopic Bariatric Surgery since 1999, having completed over 2000 Bariatric Surgical Cases safely, and with great success. Here you can watch Dr. Jawad performing a Laparoscopic Roux-En-Y Gastric Bypass surgery, with audio commentary describing the procedure.
Laparoscopic Roux-en-Y Gastric Bypass with Hand-Sutured Anastomosis. Dr. Dennis Smith, Advanced Obesity Surgery, Marietta, GA
Roux-en-Y Gastric Bypass Surgery
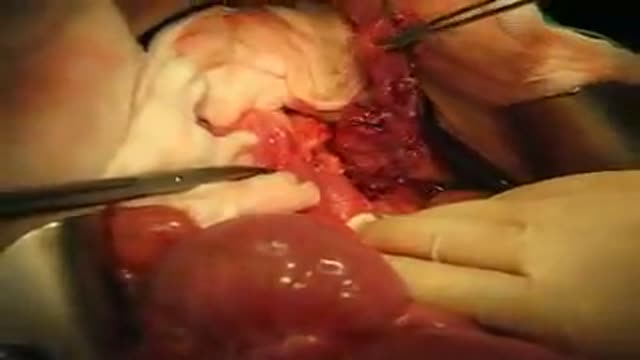
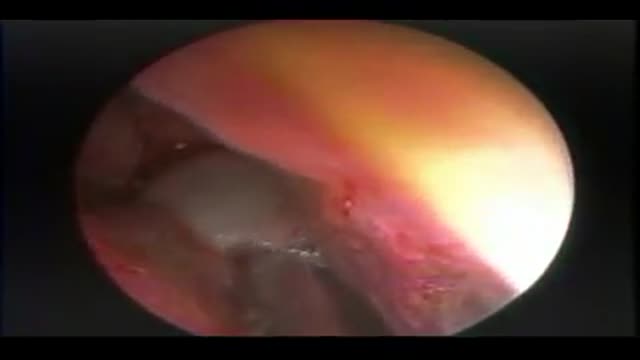
Surgery during a Pancreatectomy. One can see the pancreas half extracted. This is Experimental Surgery, taken during a Pancreas transplantation
The Stevens Laser Bra works to create a more permanent breast lift for women with sagging breasts, and can be combined with other surgery at Marina Plastic Surgery in Los Angeles, including breast augmentation or reduction, to create a long-lasting, natural transformation of the breast area.
Dr. Daniel Del Vecchio, Harvard trained plastic surgeon, performs his breast lift technique, filling the upper portion of the breast for added volume
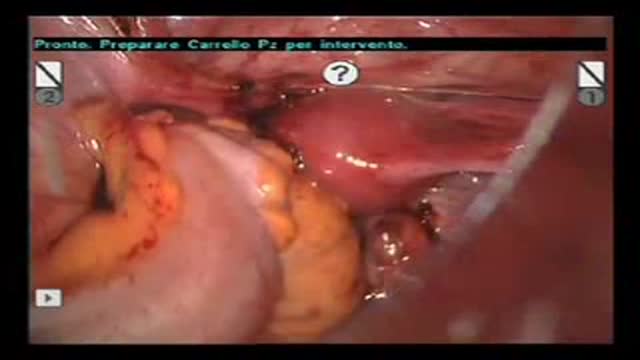
A good case comprising of laparoscopic cholecystectomy with lap. assisted vaginal hysterectomy done simultaneously
Robot-Assisted Laparoscopic Rectal resection for Endometriosis.Operation performed by D.Vitobello, director of divisione of Gynaecology, and G.Baldazzi,director of Surgical department. Abano Terme Hospital Padova (Italy)
Breast augmentation is a surgical procedure to enhance the size and shape of a woman's breasts for a number of reasons: To enhance the body contour of a woman who, for personal reasons, feels her breast size is too small To restore breast volume lost due to weight loss or following pregnancy To achieve better symmetry when breasts are moderately disproportionate in size and shape To improve the shape of breasts that are sagging or have lost firmness, often used with a breast lift procedure. By inserting an implant behind each breast, surgeons are able to increase a woman's bustline by one or more bra cup sizes.
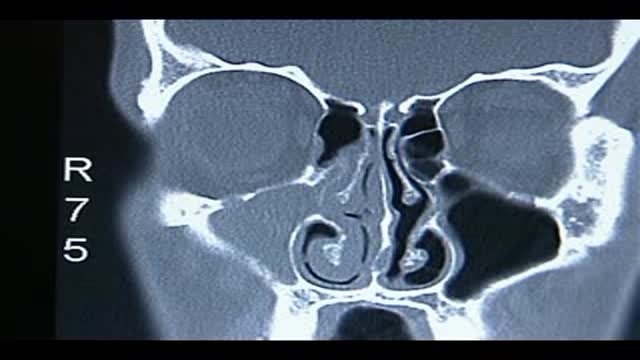
Endoscopic Treatment of Allergic Fungal Maxillary Sinusitis
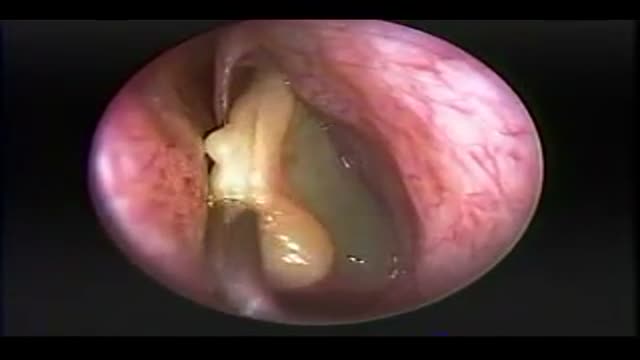
The endoscopic removal of a large intramaxillary sinus cyst which contained serous like fluid and many shiny falt white cholesterol crystals.
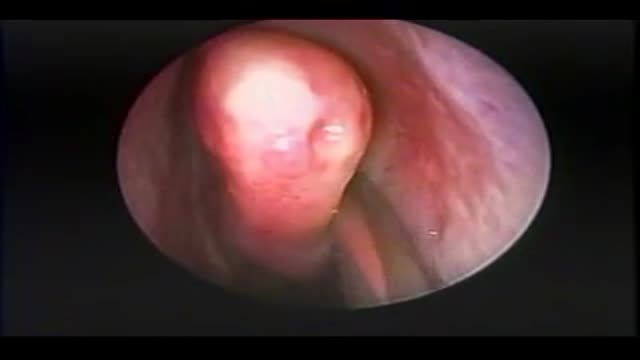
Endoscopic Removal of a Large Choanal Polyp
Endoscopic Nasal Polypectomy Using a Stryker "Hummer"
The endoscopic resection of a sharp bony nasal septal spur
Open rhinoplasty without oseotomies. Basic steps for rasping of dorsal hump and cephalic trim with septoplasty and tip strut.
Robotic Simple Prostatectomy