Ultimi video
open multi puncture testicular biopsy to retrieve sperm for ICSI (IntaCytoplasmic Sperm Injection)
The In-Line vasectomy is a minimally invasive, all cautery procudure. The ILV instruments were standardized by measurement and design to perform specific functions within a 4mm space.The procedure is rapid and reliable.
This video clips shows a tubal ligation (sterilization) performed on a female using a fallopian ring applicator
Female breast exam video
ectal exam is an internal examination of the rectum such as by a physician or other healthcare professional.
The digital rectal examination (DRE, Latin palpatio per anum or PPA) is a relatively simple procedure. The patient is placed in a position where the anus is accessible and relaxed (lying on the side, squatting on the examination table, bent over the examination table, etc). The physician inserts a gloved and lubricated finger into the rectum through the anus and palpates the insides.
The DRE is inadequate as a screening tool for colorectal cancer because it examines less than 10% of the colorectal mucosa; colonoscopy is preferred. However, it's an important part of a general examination, as many tumors or other diseases are made manifest in the distal part of the rectum.
This examination may be used: * for the diagnosis of rectal tumors and other forms of cancer; * in males, for the diagnosis of prostatic disorders, notably tumors and benign prostatic hyperplasia; * for the diagnosis of appendicitis or other examples of an acute abdomen (i.e. acute abdominal symptoms indicating a serious underlying disease); * for the estimation of the tonicity of the anal sphincter, which may be useful in case of fecal incontinence or neurologic diseases, including traumatic spinal cord injuries; * in females, for gynecological palpations of internal organs * for examination of the hardness and color of the feces (ie. in cases of constipation, and fecal impaction); * prior to a colonoscopy or proctoscopy. * to evaluate haemorrhoids
The DRE is frequently combined with an FOBT (fecal occult blood test), which may be useful for diagnosing the etiology of an anemia and/or confirming a gastrointestinal bleed.
Sometimes proctoscopy may also be part of a rectal examination.
How To Save The Facial Nerve During Parotid Gland Surgery
A video of a surgery of corneal graft transplantation
The Ex-PRESS Mini Glaucoma Shunt provides a simplified method of filtration surgery for patients with open angle glaucoma. The Ex-PRESS implanted Under a Scleral Flap is a minimally invasive procedure with predictable results.
Short Version of Yag Laser Treatment of Capsule Opacity or "after cataract" Video Presentation by Tampa Bay Area Ophthalmologist Ahad Mahootchi, MD from the Eye Clinic of Florida.
Scott Geller MD of Fort Myers Florida uses A LASAG Yag laser is in thermal mode, 1.5 Joules/pulse to treat the trabecular meshwork between the cornea and iris for glaucoma. The view is of the inside anterior eyeball.
real time video of modern cataract surgery employing a temporal, clear-corneal approach with topical anesthesia and ultrasound phacoemulsification; an aspheric silicone lens implant is inserted
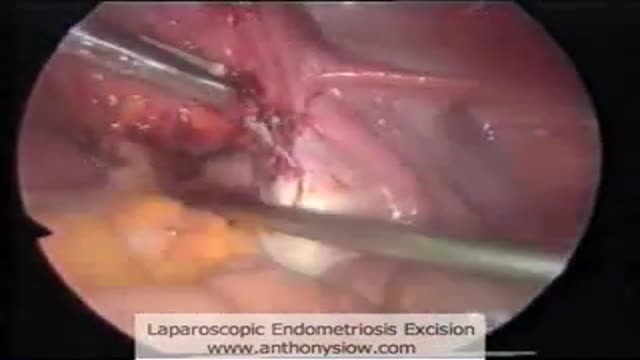
Laparoscopic excision of endometriosis
laparoscopic management of ovarian cyst
laparoscopic polymyomectomy
Removal of the womb by keyhole surgery. The womb is detached from its pelvic attachments and removed through the birth canal. The birth canal is then stitched closed.
Hysterectomy done laparoscopically is a relative new approach to the classical hysterectomy procedure, the advantages are better anatomic views, less bleeding, less surgical time and less recovery time
A video showing the surgery of vaginal hysterectomy Operation
A great video showing Total Abdominal Hysterectomy
This patented device replaces cumbersome metal retractors for a variety of surgical procedures. The surgeon has maximum unobstructed exposure and the size of the required incision is minimized.
Endometrial Polyp is removed using a IUR (Smith@Nephew)by B.C. Schoot Gynaecologist dept OB/GYN Catharina Hospital Eindhoven The Netherlands