Latest videos
A video showing the surgery of vaginal hysterectomy Operation
A great video showing Total Abdominal Hysterectomy
This patented device replaces cumbersome metal retractors for a variety of surgical procedures. The surgeon has maximum unobstructed exposure and the size of the required incision is minimized.
Endometrial Polyp is removed using a IUR (Smith@Nephew)by B.C. Schoot Gynaecologist dept OB/GYN Catharina Hospital Eindhoven The Netherlands
daVinci Robotic hysterectomy, pelvic, and para-aortic lymphadenectomy for endometrial cancer
The surgical video details a robotic assisted hysterectomy in a patient with early stage endometrial/uterine cancer. Anatomy of the pelvis and the technique of a robotic hysterectomy is demonstrated in this video.
Operation performed by Dr D. Vitobello
Director of Division of Gynaecology and Obstetrics. Abano Terme Hospital, Padova (Italy)
Vaginal Hysterectomy utilizing the PlasmaSeal Open Forceps presented by Kristi Keil, MD.
This video shows vaginal breech birth which is recommended to be delivered by C.Section in modern obstetrics
A video showing ventouse delivery or child birth
a video showing the process of child birth or delivery using forceps
Anterior and Posterior Vaginal Repair Plus IVS Tunne
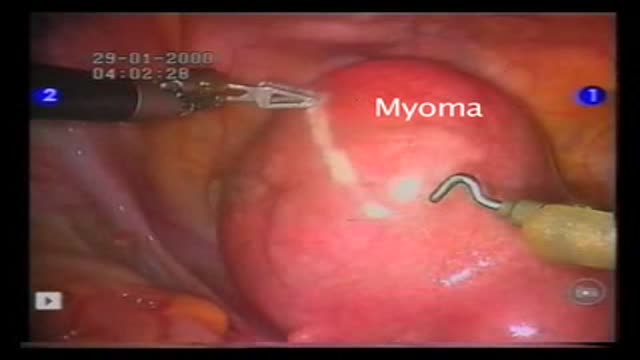
Myomectomy means the surgical removal of just the fibroid, with reconstruction and repair of the uterus. There are now a number of techniques used to perform myomectomy: through an abdominal incision, vaginal incision, with a laparoscope
Removal of fibroid with keyhole surgery. A 8cm fibroid is removed from the top of the womb. The womb incision is repaired with laparoscopic suturing using monocryl stitch.
Breast cancer is a malignant tumor that develops from the cells of
the breast. It is the most common type of cancer among women in
the United States. It is most often curable when found early. The
normal breast consists of three main components: the lobules
(milk-producing glands), the ducts (thin tubes that connect the
lobules to the nipple) and the stroma (fatty tissue and ligaments
surrounding the ducts and lobules, blood vessels, and lymphatic
vessels). About 80% of breast cancers start in the ducts.
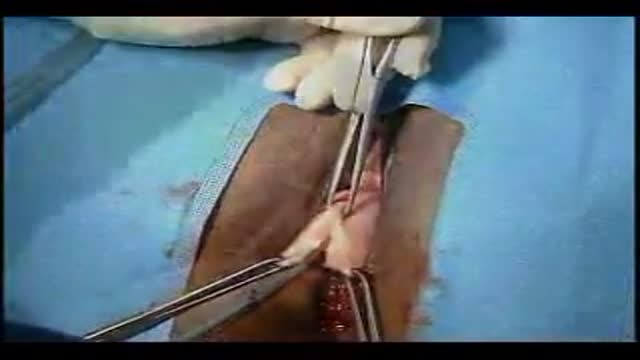
catheterization of the male urethra by a foley catheter
Acclaimed sexologist Hanny Lightfoot-Klein, author of several highly illuminating books on genital mutilation, discusses compromises in orgasm after male circumcision. Also commenting is cultural anthropologist James De Meo.From the groundbreaking documentary film, "Whose Body, Whose Rights?"
Laparoscopic Excision of Hydatid cyst Of liver
The dilatation and Curettage procedure that is commonly performed (D and C)Part 2