Latest videos
Dr. Fizan Abdullah is head of the Division of Pediatric Surgery and vice chair of the Department of Surgery at Ann & Robert H. Lurie Children's Hospital of Chicago. His special interests include Chest wall deformities, pectus excavatum, abdominal wall defects, neonatal surgery, pulmonary and upper airway malformations, congenital diaphragmatic hernia, esophageal and gastrointestinal anomalies, hernia repair, tissue engineering, extracorporeal membrane oxygenation (ECMO), surgical safety protocols and surgical infections.
Learn more at www.luriechildrens.org
Children are special patients, and their medical needs are unique, including their surgical needs. At UNC Hospitals, an expert and experienced team of physicians treat children in a kid-friendly and family-centered environment. UNC Pediatric Surgeon Dr. Timothy Weiner explains
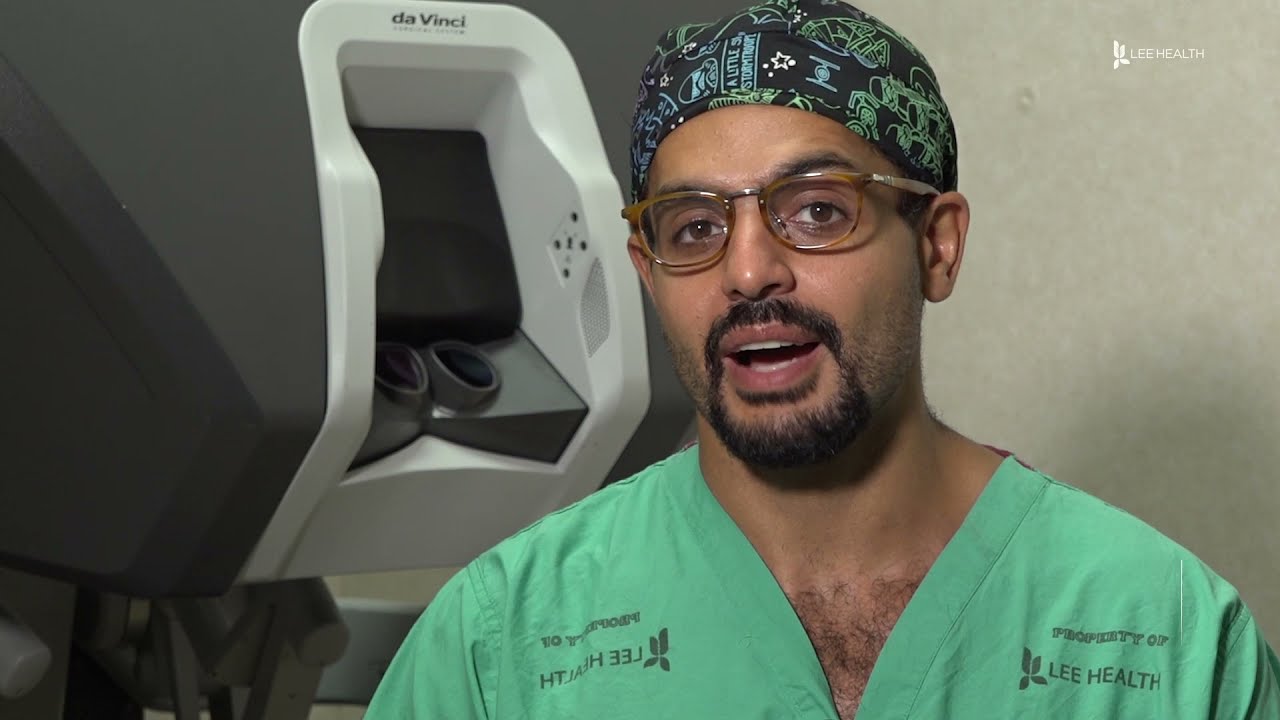
From across the room, using controls and pedals—pediatric surgeons at Golisano Children’s Hospital are now able to operate on patients without even touching them. “It allows performances of deep surgeries in the pelvis or abdomen through tiny, little incisions as opposed to a traditional, large incision to get access to the areas where urologists often operate,” explained Dr. Rahman Abd-El-Barr, a pediatric urologist with Golisano Children’s Hospital of Southwest Florida.
The DaVinci robot is a robotic platform that allows surgeons to do minimally invasive surgery, leaving patients with smaller incisions and a quicker recovery. “This is important because it allows us to minimize recovery time, pain, bleeding with surgery, and especially with kids, it helps them to get back on their feet right away,” he said.
So when high school athlete, Reagan Rebeor found out she needed to have kidney surgery, she decided to have it robotically. “Thankfully, I did that because if not, I would have had a long scar down my stomach instead of small holes, small incisions. I had pain for three days, three or four days. Then after that, I was fine,” she said.
While it’s not an option for all pediatric surgeries, doctors say it can be very beneficial for teenage and adult patients needing reconstructive surgery. An option that allows patients a quicker and easier recovery.
View More Health Matters video segments at LeeHealth.org/Healthmatters/
Lee Health in Fort Myers, FL is the largest network of health care facilities in Southwest Florida and is highly respected for its expertise, innovation and quality of care. For more than 100 years, we’ve been providing our community with personalized preventative health services and primary care to highly specialized care services and robotic assisted surgeries. Lee Health - Caring People. Inspiring Care.
Visit LeeHealth.org
Children are not little adults, which is why even the simplest of procedures requires a hospital that is 100 percent dedicated to caring for children. Children’s Mercy is one of only 10 centers in the country to be as recognized as a Level 1 Children’s Surgery Center, the highest possible rating. The result? An organization with pediatrics specialists in every subspecialty that sets the standard of care instead of just practicing it.
Mr Brian MacCormack talking about Paediatric Surgery Emergencies. This talk is part of the Paediatric Emergencies 2022 event. To get your CME certificate for watching the video please visit https://www.paediatricemergenc....ies.com/conference/p
#PaediatricEmergencies #PaediatricEmergencies2022 #PaediatricSurgery
Sanjeev Dutta, MD, FACS discusses the fascinating new world of surgical technology. The pediatric general surgeon shares how medicine and technology have combined to achieve less invasive procedures and healthier outcomes for surgical patients.
Dr. Dutta is a pediatric general surgeon at Lucile Packard Children's Hospital. He is also an Associate Professor of Surgery at Stanford School of Medicine and Surgical Director of the Multidisciplinary Initiative for Surgical Technology Research.
Learn more about Stanford Children's Health. http://www.stanfordchildrens.org.
This title in the new Surgical Techniques Atlas series presents state-of-the-art updates on the full range of pediatric surgical techniques performed today. Expand your repertoire and hone your clinical skills thanks to the expert advice, procedural videos, and online access at expertconsult.com. For more information, please visit http://www.us.elsevierhealth.com/product.jsp?sid=EHS_US_BS-SPE-59&isbn=9781416046899&dmnum=null&elsca1=CriticalCare&elsca2=soc_med&elsca3=null&elsca4=youtube_ELSpromovideos
Following Dr. Eric Skarsgard on his grueling 19-hour day at BC Children's Hospital, we meet several of his patients -- some of who need surgery that day, and some who have chronic conditions and need regular check-ups with him -- and learn how he works with medical students and on research projects as time allows.
Not sure what to expect with your child's upcoming surgery at Wesley Children's Hospital? This guided tour will walk you through the process to make both patients and families feel as comfortable as possible.
As you consider Fort HealthCare and our Pediatric Surgical Services, here is a quick tour to give you and your child an idea of what to expect.
We look forward to helping you.
To find out more information, please visit forthealthcare.com/PediatricSurgery
Video production by Highlights Media, LLC
Having surgery can be frightening for anyone, but it's especially scary for kids who don't always understand what's going on, or what the grown-ups are saying. We're here to help!
Join Avrie, who had surgery at the Sacred Heart Children's Hospital pediatric surgery center in Spokane, WA. Maybe after watching and hearing her story, you and your kiddo will feel better about having surgery in the hospital.
Follow Avrie's trip - from check-in, vital signs and pre-op checks; meeting the doctor who will do his surgery, along with the anesthesiologist, surgery nurse and the Child Life Specialist; the trip to the Operating Room; waking up in the recovery room with his mom by his side; and getting ready to go home.
To learn more about the pediatric surgery center at Sacred Heart Children's Hospital, visit https://washington.providence.....org/locations-direct
Johns Hopkins Children’s Center Surgeon-in-Chief David Hackam provides information about general pediatric surgery and when it is time to see a general pediatric surgeon. #PediatricSurgery #JohnsHopkins
For more information on general pediatric surgery at Johns Hopkins Children's Center, visit https://www.hopkinsmedicine.or....g/johns-hopkins-chil
FAQ's
0:02 What is a general pediatric surgeon?
0:31 When is it time to see a pediatric surgeon?
1:02 What are some of the most common surgical problems seen by general pediatric surgeons?
1:43 Describe research being done in the field.
2:15 Why choose Johns Hopkins Children's Center for general pediatric surgery?
MUSC Children’s Health offers South Carolina’s only Level 1 Children’s Surgery Center, representing excellence in inpatient surgery at MUSC Shawn Jenkins Children’s Hospital, as well as outpatient surgery at R. Keith Summey Medical Pavilion. These two state-of-the-art facilities are equipped with a team of pediatric board-certified providers utilizing pediatric-specific devices and the most technologically advanced tools.
World-renowned surgeons at Shriners Hospitals for Children – Northern California provide complex pediatric surgery for children one-year and older with congenital and acquired conditions. Children from throughout the Western United States with chest wall malformations, gastro-intestinal disease, ano-rectal disorders, urologic conditions and other complex surgical needs benefit from the expert care. The pediatric surgery team is devoted to the development of innovative and minimally invasive surgical techniques.
What to expect during the day of a pediatric surgery at Sutter Children's Center Sacramento.
For more information, visit https://ukhealthcare.uky.edu/doctors.
When your child needs surgery, it can be overwhelming and sometimes scary. At Mayo Clinic Children’s Center, our highly skilled surgeons apply deep experience and specialized training to offer individualized care for your child and your family.
Pediatric surgeons at Texas Children’s Hospital West Campus perform general surgical procedures such as circumcisions, removal of foreign objects, hernia repair, and suturing of minor lacerations. While more complex surgeries take place at the Texas Children’s Main Campus, pre-operative and follow-up outpatient care for those procedures is available at the West Campus.
Everything about Texas Children’s Hospital West Campus is dedicated to the health and wellness of children. As greater Houston's first suburban hospital designed exclusively for children, we offer the expert care you've come to trust from Texas Children's Hospital coupled with a location that's convenient and accessible for area families. Our facility is located just off the westbound feeder road of the Katy Freeway (at I-10 and Barker Cypress).
For more information about Texas Children's Hospital West Campus, visit http://www.texaschildrens.org/....Locate/In-the-Commun
Meet Dr. Allen Milewicz, chief of community surgery at Texas Children's West Campus
https://www.youtube.com/watch?v=uMoCdipuKfA&index=16&list=PLiN68C9rloPBD-E9ChWhVy73h7V3SEMlm
Our surgeons take a compassionate, family-centered approach to both inpatient and outpatient care. We’re committed to making sure both you and your child understand our process. Told through a kid's eyes, this video tour reveals our caring approach.
To learn more about pediatric surgery at Stamford Hospital, visit: https://www.stamfordhealth.org..../care-treatment/pedi