Latest videos
Video showing normal vagina delivery and child birth
aricose veins are gnarled, enlarged veins. Any vein may become varicose, but the veins most commonly affected are those in your legs and feet. That's because standing and walking upright increases the pressure in the veins of your lower body. For many people, varicose veins and spider veins — a common, mild variation of varicose veins — are simply a cosmetic concern. For other people, varicose veins can cause aching pain and discomfort. Sometimes varicose veins lead to more-serious problems.
Fertilization of the egg with sperm generally occurs during the two weeks following the first day of your last menstrual period.1 The week of pregnancy that you are entering is dated from the first day of your last period. This means that in the first two weeks or so, you are not actually pregnant - your body will be preparing for ovulation as normal.
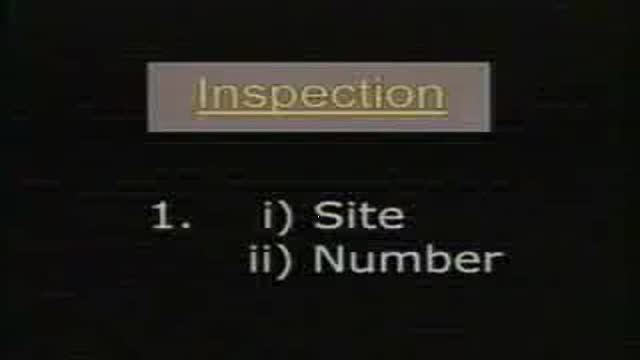
examination of a case of inguino-scrotal swelling as in cases of oblique inguinal hernia..etc
A testicular examination is mainly performed on male patients who present with testicular pathology e.g. pain, swelling, a lump. Although titled testicular examination it involves the examination of the penis, scrotum and testes. As this is an intimate examination it is pertinent to gain a good rapport with your patient, maintain good communication and ensure the patient’s dignity at all times. Remember to offer a chaperone for this skill. For the purposes of your exam, you will most likely be examining a mannequin.
Hypothyroidism and Hyperthyroidism Symptoms: Swollen Neck. A goiter is an enlargement of the thyroid gland. As shown here, an enlarged thyroid can be seen as a swelling in the front of the neck. A goiter can occur with either hypothyroidism or hyperthyroidism
ost of us come across this particular sign quite often. Of course, you can just jump to the numerous investigations and one after another, rule out the possible causes, finally getting to the diagnosis. For me, that’s no fun at all. Although I still don’t know whether I am going to become a surgeon or not (embarassing for me, since I’m going to be done with med-school this year), its pretty fascinating. If I were to work in a country whether investigations aren’t that expensive, I would definitely just perform a small examination and take a short history, sending off my patient to get a myriad of investigations, reporting to me after a while, with the diagnosis in his reports.
Peripheral vascular disease, also called PVD, refers to any disease or disorder of the circulatory system outside of the brain and heart. The term can include any disorder that affects any blood vessels. It is, though, often used as a synonym for peripheral artery disease. PVD is the most common disease of the arteries. The build-up of fatty material inside the vessels, a condition called atherosclerosis or hardening of the arteries, is what causes it. The build up is a gradual process. Over time, the artery becomes blocked, narrowed, or weakened.
full pediatric examination of lymph nodes
The HEENT, or Head, Eye, Ear, Nose and Throat Exam is usually the initial part of a general physical exam, after the vital signs. Like other parts of the physical exam, it begins with inspection, and then proceeds to palpation. It requires the use of several special instruments in order to inspect the eyes and ears, and special techniques to assess their special sensory function. This module reviews some of the relevant surface anatomy and describes the basic HEENT exam. The module includes an introduction to use of the ophthalmoscope.
Pediatric musculoskeletal examination
If your body makes too little melanin, your skin gets lighter. Vitiligo is a condition that causes patches of light skin. Albinism is a genetic condition affecting a person's skin. A person with albinism may have no color, lighter than normal skin color, or patchy missing skin color.
Meningitis is a common life-threatening medical emergency caused by infectious and non-infectious agents. Rapid and accurate evaluation by history and clinical examination is helpful to guide further specific investigation and treatment. Kernig's sign, Brudzinski's sign, and nuchal rigidity are bedside diagnostic signs used to evaluate suspected cases of meningitis. The presence of meningeal irritation, however, is not pathognomonic for meningitis.
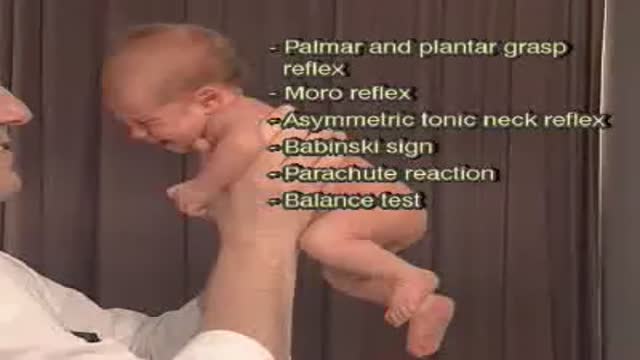
In a normal person, when a muscle tendon is tapped briskly, the muscle immediately contracts due to a two-neuron reflex arc involving the spinal or brainstem segment that innervates the muscle. The afferent neuron whose cell body lies in a dorsal root ganglion innervates the muscle or Golgi tendon organ associated with the muscles; the efferent neuron is an alpha motoneuron in the anterior horn of the cord. The cerebral cortex and a number of brainstem nuclei exert influence over the sensory input of the muscle spindles by means of the gamma motoneurons that are located in the anterior horn; these neurons supply a set of muscle fibers that control the length of the muscle spindle itself. Hyporeflexia is an absent or diminished response to tapping. It usually indicates a disease that involves one or more of the components of the two-neuron reflex arc itself. Hyperreflexia refers to hyperactive or repeating (clonic) reflexes. These usually indicate an interruption of corticospinal and other descending pathways that influence the reflex arc due to a suprasegmental lesion, that is, a lesion above the level of the spinal reflex pathways.
Pediatrics abdominal examination
examination of the lungs and respiration of newborn and children
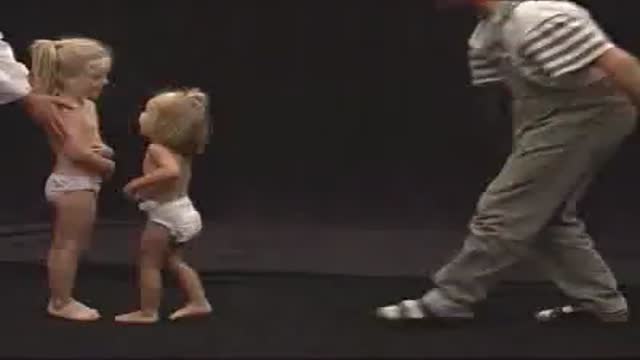
Primitive reflexes are reflex actions originating in the central nervous system that are exhibited by normal infants, but not neurologically intact adults, in response to particular stimuli. These reflexes are absent due to the development of the frontal lobes as a child transitions normally into child development.
Pediatric examination of muscle strength and muscle tone
Examination of pulse, blood pressure and capillary refilling time
full examination of the heart