Latest videos

When diving into a Breast Reduction procedure, there are many things to consider. Even as a patient, being aware of any concerns and how the procedure works is important. Therefore, when a plastic surgeon operates on a patient, the results are clear. Dr. Linder, a Breast surgeon specialist in Beverly Hills, helps explain what goes into a Breast Reduction Procedure.
Breast implants do not last forever, and during its lifetime, it may rupture. Dr. Linder, Beverly Hills breast surgeon specialist, breaks down how removing breast implants works. To learn more about Dr. Stuart Linder and his expertise, Visit: www.drlinder.com
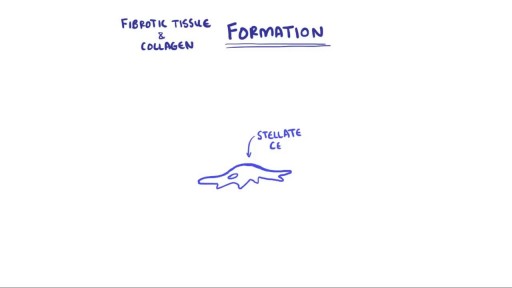
Hepatitis and chronic alcohol abuse are frequent causes. Liver damage caused by cirrhosis can't be undone, but further damage can be limited. Initially patients may experience fatigue, weakness, and weight loss. During later stages, patients may develop jaundice (yellowing of the skin), gastrointestinal bleeding, abdominal swelling, and confusion. Treatments focus on the underlying cause. In advanced cases, a liver transplant may be needed.

With the help of vitamin K, the liver produces proteins that are important in blood clotting. It is also one of the organs that break down old or damaged blood cells. The liver plays a central role in all metabolic processes in the body. In fat metabolism the liver cells break down fats and produce energy.
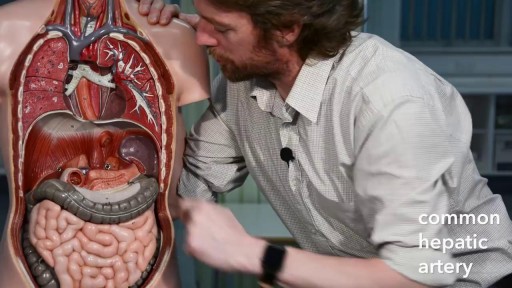
The primary functions of the liver are: Bile production and excretion. Excretion of bilirubin, cholesterol, hormones, and drugs. Metabolism of fats, proteins, and carbohydrates. Enzyme activation. Storage of glycogen, vitamins, and minerals. Synthesis of plasma proteins, such as albumin, and clotting factors.
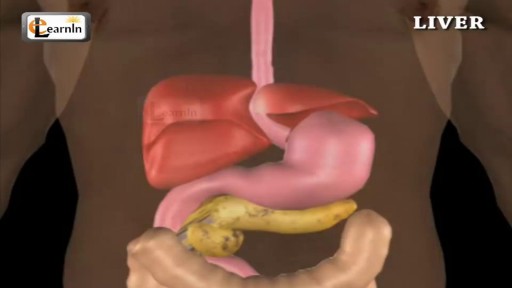
The liver regulates most chemical levels in the blood and excretes a product called bile. ... Production of bile, which helps carry away waste and break down fats in the small intestine during digestion. Production of certain proteins for blood plasma.

Nystagmus is a vision condition in which the eyes make repetitive, uncontrolled movements. These movements often result in reduced vision and depth perception and can affect balance and coordination. These involuntary eye movements can occur from side to side, up and down, or in a circular pattern.

Central vestibular nystagmus results from stimulation, injury, disease of the central vestibular pathways of the brainstem or the cerebellum, or lesion of the vestibular nuclei. It is typically a jerk nystagmus, which can be purely horizontal, vertical or torsional.

Mammogram are great technologies, however, sometimes it cannot detect many things under our bodies. In this video, Dr. Linder is performing a breast implant removal and revision on a patient who has a rupture breast implants. Dr. Stuart Linder is a Beverly Hills board certified plastic surgeon, specializing in body sculpting and reconstructive procedures including breast augmentation, reduction, lift, liposuction and tummy tuck. He is board-certified by the American Board of Plastic Surgery and is affiliated with the American College of Surgeons, the American Society of Plastic and Reconstructive Surgeons and the American Medical Association.
There many concerns and questions about how a breast augmentation procedure works. Dr. Linder a highly qualified plastic surgeon based in Beverly Hills, demystifies those worries. Dr. Stuart Linder is a Beverly Hills board certified plastic surgeon, specializing in body sculpting and reconstructive procedures including breast augmentation, reduction, lift, liposuction and tummy tuck. He is board-certified by the American Board of Plastic Surgery and is affiliated with the American College of Surgeons, the American Society of Plastic and Reconstructive Surgeons and the American Medical Association. Website: www.drlinder.com
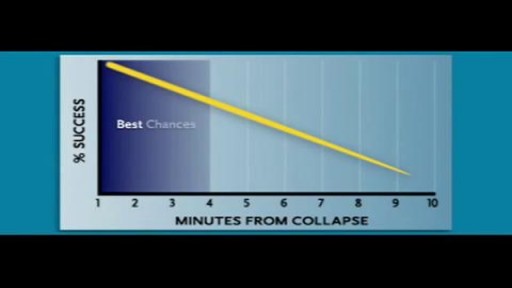
Cardiac arrest usually results from an electrical disturbance in the heart. It's not the same as a heart attack. The main symptom is loss of consciousness and unresponsiveness. This medical emergency needs immediate CPR or use of a defibrillator. Hospital care includes drugs, an implantable device, or other procedures.
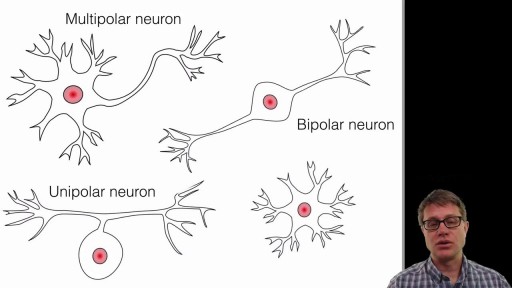
A neuron, also known as a neurone (British spelling) and nerve cell, is an electrically excitable cell that receives, processes, and transmits information through electrical and chemical signals. These signals between neurons occur via specialized connections called synapses.
t’s the brain, after all, that devises experiments and interprets their results. How the brain perceives, how it makes decisions and judgments, and how those judgments can go awry are at least as important to science as knowing the intricacies of nonbiotic experimental machinery. And as any brain scientist will tell you, there’s still a long way to go before understanding the brain will get crossed off science’s to-do list. But there has been progress. A recent special issue of the journal Neuron offers a convenient set of “perspective” papers exploring the current state of understanding of the brain’s inner workings. Those papers show that a lot is known. But at the same time they emphasize that there’s a lot we don’t know.

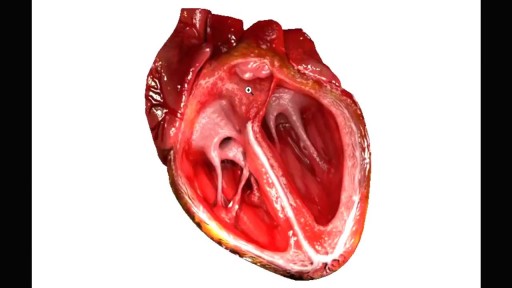
The cardiovascular system is a closed system if the heart and blood vessels. The heart pumps blood through a closed system of blood vessels. Blood vessels allow blood to circulate to all parts of the body. Arteries usually colored red because oxygen rich, carry blood away from the heart to capillaries within the tissues. Veins usually colored blue because oxygen poor, carry blood to the heart from the capillaries.
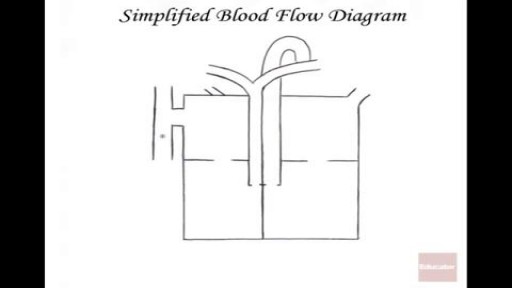
The heart itself is made up of 4 chambers, 2 atria and 2 ventricles. De-oxygenated blood returns to the right side of the heart via the venous circulation. It is pumped into the right ventricle and then to the lungs where carbon dioxide is released and oxygen is absorbed. The oxygenated blood then travels back to the left side of the heart into the left atria, then into the left ventricle from where it is pumped into the aorta and arterial circulation.

The cardiac cycle is the sequence of events that occurs when the heart beats. As the heart beats, it circulates blood through pulmonary and systemic circuits of the body. There are two phases of the cardiac cycle. In the diastole phase, the heart ventricles are relaxed and the heart fills with blood