Latest videos
Detailed examination of the joints is usually not included in the routine medical examination. However, joint related complaints are rather common, and understanding anatomy and physiology of both normal function and pathologic conditions is critically important when evaluating the symptomatic patient. By gaining an appreciation for the basic structures and functioning of the joint, you'll be able to "logic" your way thru the exam, even if you can't remember the eponym attached to each specific test!
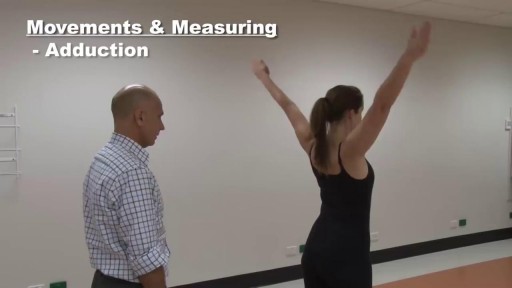
houlder examination frequently appears in OSCEs. You’ll be expected to pick up the relevant clinical signs using your examination skills. This shoulder examination OSCE guide provides a clear step by step approach to examining the shoulder, with an included video demonstration.
The major elements of the cardiac exam include observation, palpation and, most importantly, auscultation (percussion is omitted). As with all other areas of the physical exam, establishing adequate exposure and a quiet environment are critical. Initially, the patient should rest supine with the upper body elevated 30 to 45 degrees. Most exam tables have an adjustable top. If not, use 2 or 3 pillows. Remember that although assessment of pulse and blood pressure are discussed in the vital signs section they are actually important elements of the cardiac exam.
This brief exam will help you to quickly detect major risks and prompt you to refer patients to appropriate specialists.
How to Prepare, Apply & Remove a Total Contact Cast
Total Contact Casting is the gold standard for treating diabetic foot ulcers; it's the most evidence-based treatment available. The Wound Care team at IU Health Methodist Hospital provides custom Total Contact Casting that completely offloads the wound, allowing it to heal in a matter of weeks.
Presence of several characteristic diabetic foot pathologies such as infection, diabetic foot ulcer and neuropathic osteoarthropathy is called diabetic foot syndrome. Due to the peripheral nerve dysfunction associated with diabetes (diabetic neuropathy), patients have a reduced ability to feel pain.
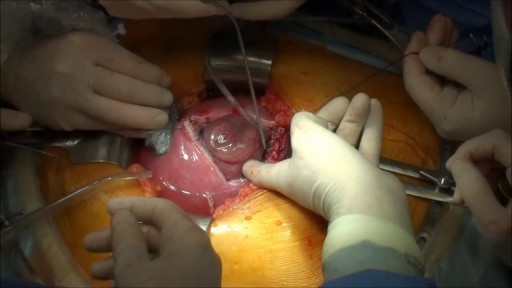
Majority of patients these days prefer PCNL ( Minimal Invasive Telescopic removal of kidney stones broken with lithoclast, removed through a button hole incision ). This patient with a big stone in the pelvis of the kidney wanted it open only so I did an open pyelolithotomy for this patient after a long time as I use to do it in routine in the past. Except for the long incision and scar as compared to PCNL the recovery time was the same and patient went home third day happily walking and eating.
Treatment consists of diet modifications and laxatives A high-fiber diet can be effective, along with over-the-counter medications, such as stool softeners. In some cases, a medical procedure to remove the hemorrhoid may be needed to provide relief.
- A baby born with two heads is expected to survive after doctors removed the parasitic twin that was “feeding off” her blood supply. The baby girl, who is yet to be named, was born via C-section at Ram Snehi Hospital in northern India last month
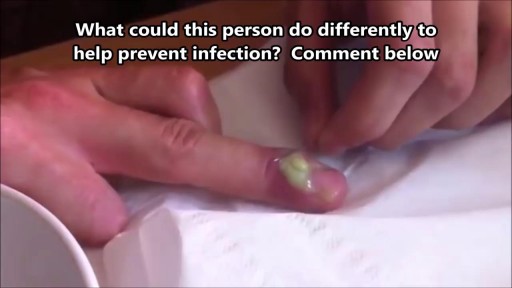
What Is a Paronychia (Nail Infection)? An infection that develops along the edge of the fingernail or toenail is called a paronychia (pear-ah-NIK-ee-ah). It is the most common hand infection and, if left untreated, can progress to a more severe infection of the entire finger or toe. Paronychia is distinguished from other infections such as onychomycosis and herpetic whitlow by its location and appearance.
What is an ingrown hair cyst? An ingrown hair cyst refers to an ingrown hair that turns into a cyst — a large bump that extends between the skin’s surface and deep underneath it. The appearance is a cross between a regular ingrown hair and an acne cyst, though this is a different condition. These types of cysts are common among people who shave, wax, or use other methods to remove their hair. Although you may be eager to get rid of these cysts simply because of their appearance, it’s also important to watch for signs of an infection. Keep reading to learn what causes these cysts to form, plus how to treat them and prevent them from returning.
What Is It? Your wisdom teeth (third molars) usually start to erupt (enter your mouth) during the late teen years. Sometimes, there's not enough room for them. They may come into your mouth partially or not at all. Partial eruption of a wisdom tooth can create a flap of gum tissue next to the tooth. The flap can trap bits of food and debris. It can turn into a hotbed for bacteria. It's called pericoronitis if the tissue around the tooth becomes inflamed. Pericoronitis also can occur around a wisdom tooth that is still completely under the gums. Symptoms Symptoms include: Painful, swollen gum tissue in the area of the affected tooth. It can be difficult to bite down comfortably without catching the swollen tissue between your teeth. A bad smell or taste in the mouth Discharge of pus from the gum near the tooth More serious symptoms include: Swollen lymph nodes under your chin (the submandibular nodes) Muscle spasms in the jaw Swelling on the affected side of the face Diagnosis Usually, someone with pericoronitis goes to the dentist, complaining of pain in the area of the back tooth. Pericoronitis is diagnosed during the clinical exam. Your dentist will see inflamed gum tissue in the area of the unerupted or partly erupted wisdom tooth. The gums may be red, swollen or draining fluid or pus. Expected Duration Pericoronitis can be managed with antibiotics and warm salt water rinses. It goes away in about one week. However, it can return. This is likely to happen if the tooth does not completely enter the mouth and food and bacteria keep building up under the gum. Prevention You can help to prevent pericoronitis by brushing any erupting wisdom tooth and flossing around it. This will help make sure that food and bacteria do not build up under the gums. However, sometimes these steps do not work. If pericoronitis returns, you may need to have the flap of gum tissue removed. In some cases, the flap of tissue grows back and the wisdom tooth will need to be extracted. Treatment Pericoronitis can be tricky to treat. That's because the flap of gum tissue won't go away until the wisdom tooth emerges naturally, the tissue is removed or the tooth is removed. Your dentist will clean the area thoroughly by rinsing under the flap with water to remove bits of food and pus. Your dentist also may need to remove damaged tissue. If the area is infected, you'll most likely be given antibiotics. Your dentist will explain how to keep the area clean, which is the best way to prevent the problem from returning. This usually involves brushing and flossing daily and rinsing your mouth with water several times a day. These steps will help to prevent food from getting stuck under the gum flap. In some cases, your dentist may suggest removing the erupting tooth. Or the dentist may want to remove the tooth above it, which bites down on the gum below. If your dentist thinks the tooth may erupt fully into the mouth without problems, he or she may leave it alone. However, if pericoronitis comes back, the tooth may be extracted. Pericoronitis that causes symptoms should be treated as soon as possible. If it is not, the infection can spread to other areas of your mouth. The most severe cases are treated in a hospital. They sometimes require intravenous antibiotics and surgery. When To Call a Professional If you have symptoms of pericoronitis, make an appointment to see your dentist. If your wisdom teeth are coming in, visit your dentist at least twice a year for regular checkups. During those visits, the dentist can check on the progress of your wisdom teeth. Prognosis Pericoronitis does not cause any long-term effects. If the affected tooth is removed or erupts fully into the mouth, the condition cannot return.
WHAT IS BURN DEBRIDEMENT? A burn is damage to body tissues caused by sunlight, heat, fire, electricity, friction, radiation, chemicals, hot water or steam. Burns may become infected. Infected burns and the swelling that happens as a result can cause severe damage to the organs and tissues underneath the burned area by putting pressure on the tissues, nerves, and blood vessels. To allow healthy tissue to heal and to prevent more damage or infection, burned tissue is removed in a procedure called burn debridement. Burn debridement can be done by several different methods. They include surgical, chemical, mechanical, or autolytic tissue removal. Debridement may need to be done multiple times as the burned area heals.
Debridement is the removal of necrotic tissue, foreign debris, bacterial growth, callus, wound edge, and wound bed tissue from chronic wounds in order to stimulate the wound healing process. Stimulation of wound healing mediated by debridement is thought to occur by the conversion of a chronic non-healing wound environment to an acute healing environment through the removal of cells that are not responsive to endogenous healing stimuli. Debridement is used commonly in standard wound treatment of diabetic foot ulcers (DFUs). Methods of debridement include surgery (sharp debridement), chemical debridement (antiseptics, polysaccharide beads, pastes), autolytic (hydrogels, hydrocolloids and transparent films), biosurgery (maggots), mechanical (hydrodebridement), and biochemical debridement (enzyme preparations). Callus is a buildup of keratinized skin formed under conditions of repeated pressure or friction and may contribute to ulcer formation by creating focal areas of high plantar pressure. The debridement of callus has been proposed to be relevant for both treatment and prevention of DFU. The purpose of this report is to retrieve and review existing evidence of comparative clinical effectiveness of different methods of debridement for the treatment of DFUs. Additionally examined in this report is the clinical effectiveness for treatment and prevention of DFU using callus debridement. Cost-effectiveness, and existing debridement guidelines for the treatment of DFUs will also be reviewed.
Masturbating is totally healthy, and totally normal. There are tons of myths out there meant to scare you into thinking masturbation is wrong or bad. But the truth is masturbation is perfectly safe. Masturbating won't make you blind, crazy, or stupid. It won’t damage your genitals, cause pimples, or stunt your growth. It doesn’t use up all your orgasms or ruin other kinds of sex. In fact, masturbation can actually be good for you. Here are some benefits of masturbation: Masturbation is safer than any other type of sex. You can’t get pregnant or get any sexually transmitted infections from masturbating. Masturbation can help you learn what you like and don’t like sexually. And if you decide to have sex with someone, you can know what you do/don’t want to do. BONUS: getting comfortable talking about sex and your body with your partner makes it easier to talk about protecting yourself against STDs and pregnancy, too. Exploring your body and learning how to give yourself sexual pleasure can be empowering and help improve your body image. Masturbation can lower stress and help you relax. It even helps some people fall asleep. Having an orgasm releases endorphins — feel good chemicals in your brain. Orgasms can be a natural painkiller and can even help with period cramps. Mutual masturbation (masturbating with a partner) is a really safe way to have sex and let the other person know what feels good to you. If you share a sex toy, use condoms on the toy and clean it before swapping. And if you touch each other’s genitals, wash your hands before touching your own. Can I get an STD from masturbating? Nope. Masturbating is the safest sexual activity out there. There is virtually NO chance of getting an STD or any other infection from touching your own genitals (and there’s also no chance of pregnancy). STDs have to be passed from one person to another, so you can’t give yourself an STD. The one exception to this is herpes - so if you have any cold sores on your mouth and touch them, make sure to wash your hands before masturbating. But it IS possible to get an STD if you’re masturbating with another person and touching each other’s genitals. Anytime semen (cum) or vaginal fluids are spread to someone else’s body, or your genitals rub against each other, there’s a risk of STDs. So if you touch each other’s genitals, wash your hands before touching your own. STDs can also be spread by sharing sex toys with another person. You can help protect yourself by using condoms on any toys that you share (even if they’re not shaped like a penis). Put a new condom on anytime a different person uses it. If you’re the only one using your sex toys, you don’t have to worry about STDs. But if you use them with other people, protect those sex toys just like you’d protect your own genitals — put a condom on ‘em! It’s possible for masturbation to cause irritation or infections if your body is sensitive to the way you masturbate or the things you masturbate with — but this isn’t the same thing as an STD. Lotions, Vaseline, oils, and scented or flavored stuff may irritate your vulva and vagina. Masturbating roughly and not using lubrication can also lead to irritation because of friction. And germs from the anus can cause vaginal infections — so never put something in your vagina that’s been in your butt without washing it or covering it with a condom. If you’re worried that you have an STD because of pain, itching, or discomfort in your genitals, go to your doctor or your local Planned Parenthood health center.
A walk through of an interactive about male to female sex reassignment surgery.
During open carpal tunnel release surgery, the transverse carpal ligament is cut, which releases pressure on the median nerve and relieves the symptoms of carpal tunnel syndrome. An incision is made at the base of the palm of the hand. This allows the doctor to see the transverse carpal ligament.
A Texas baby, born with part of her heart outside her body ( Ectopia Cordis) , defies the odds and leaves hospital following a successful surgery.
Prenatal repair of myelomeningocele (MMC), the most common and severe form of spina bifida, is a delicate surgical procedure where fetal surgeons open the uterus and close the opening in the baby's back while they are still in the womb.