Top videos

Genital warts are one of the most common types of sexually transmitted infections. At least half of all sexually active people will become infected with human papillomavirus (HPV), the virus that causes genital warts, at some point during their lives. Women are somewhat more likely than men to develop genital warts. As the name suggests, genital warts affect the moist tissues of the genital area. Genital warts may look like small, flesh-colored bumps or have a cauliflower-like appearance. In many cases, the warts are too small to be visible. Like warts that appear elsewhere on your body, genital warts are caused by the human papillomavirus (HPV). Some strains of genital HPV can cause genital warts, while others can cause cancer. Vaccines can help protect against certain strains of genital HPV
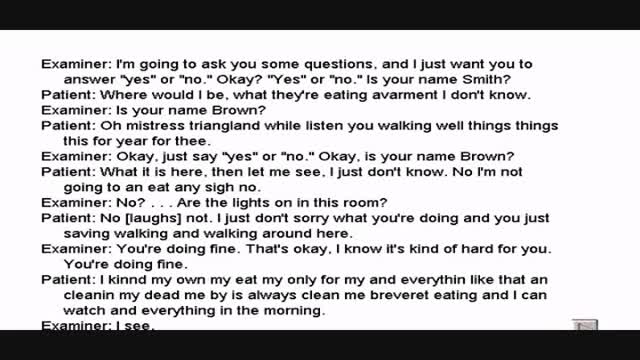
Wernicke's aphasia is a neurological disorder typically caused by stroke. It affects the Wernicke's region in the brain's left hemisphere which is reasoned to be responsible for processing of meaning, especially as it relates to verbal communication, hence the problems with speech witnessed in these patients

There are lots of fallacies about the missionary position being the best position for getting pregnant. With the woman on her back and her partner on top, it is thought that gravity will assist the sperm to swim upwards towards the egg.
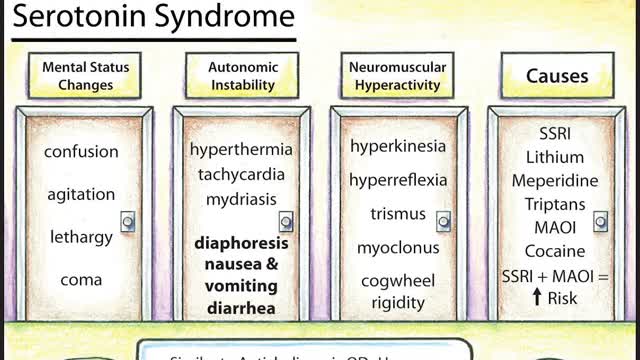
Symptoms of serotonin syndrome include a classic triad of mental status changes (eg, anxiety, delirium, confusion, restlessness), autonomic dysregulation (eg, diaphoresis, tachycardia, hypertension, hyperthermia, diarrhea, mydriasis), and neuromuscular hyperactivity (eg, hyperreflexia, tremor, rigidity, myoclonus, ocular clonus). Serotonin syndrome is clinically diagnosed and laboratory tests are used to rule out other etiologies. It usually occurs due to inadvertent interactions between drugs, therapeutic use of multiple serotonergic agents, or serotonergic medication overdose. Treatment involves discontinuation of serotonergic drugs, supportive measures, and sedation with benzodiazepines. In severe cases, a serotonin antagonist (cyproheptadine) may be used.

Candida Albicans is more than just yeast- for most people, it's already mutated into a more aggressive fungal form that eats holes through the intestinal tract causing many of todays health problems like food allergies, autoimmune disorders, Crohn's disease, IBS, low energy and many more aggressive diseases. People need to know what it is and what to do about it.

A VCUG (Voiding Cystourethrogram) is a test that looks at how well your child's kidneys, ureters and bladder are working. Your child's kidneys make urine. The urine flows from the kidneys through thin tubes (called ureters) into your child's bladder.

UPDATE 2/6/15: A new version of this animation is now available! https://www.youtube.com/watch?v=E1ljClS0DhM
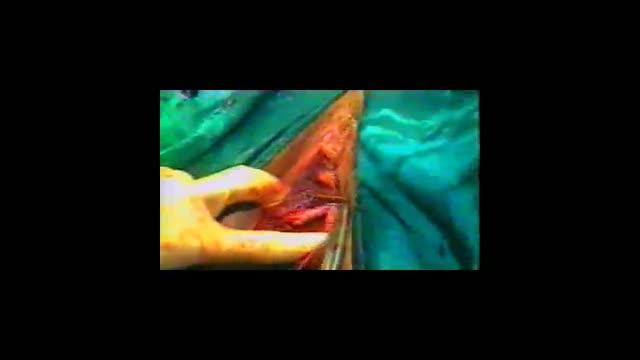
This 3D medical animation depicts the surgical removal of the appendix (appendectomy) using laparoscopic instruments. The surgery animation begins by showing an inflamed appendix (appendicitis), followed by the placement of the laparoscope. Afterward, one can see the surgical device staple, cut and remove the inflamed appendix. Following the removal of the appendix the abdomen is flushed with a sterile saline solution to ensure all traces of infection have been removed.
ANCE00183

Possible complications could include: Difficulty healing. Infection. Stump pain (severe pain in the remaining tissue) Phantom limb pain (a painful sensation that the foot or toe is still there) Continued spread of gangrene, requiring amputation of more areas of your foot, toes or leg. Bleeding. Nerve damage.