Top videos
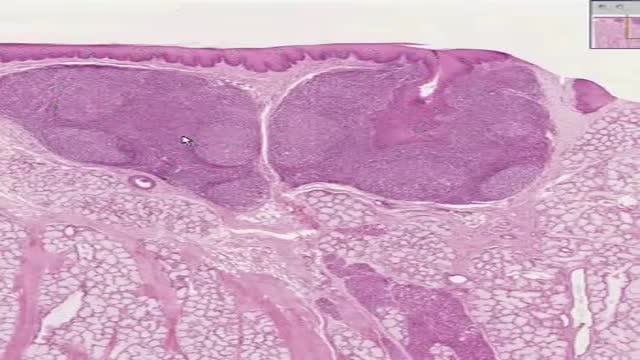
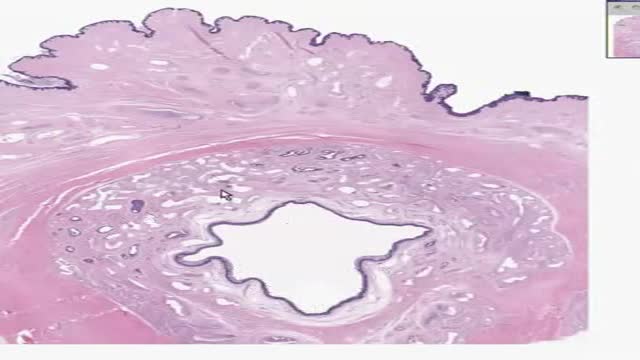
Hodgkin lymphoma has characteristics that distinguish it from other diseases classified as lymphoma, including the presence of Reed-Sternberg cells. These are large, cancerous cells found in Hodgkin lymphoma tissues, named for the scientists who first identified them. Hodgkin lymphoma is one of the most curable forms of cancer. NHL represents a diverse group of diseases distinguished by the characteristics of the cancer cells associated with each disease type. Most people with NHL have a B-cell type of NHL (about 85 percent). The others have a T-cell type or an NK-cell type of lymphoma. Some patients with fast-growing NHL can be cured. For patients with slow-growing NHL, treatment may keep the disease in check for many years.

Breath sounds can be either normal or abnormal. These sounds come from the lungs when you breathe in or out. These sounds can be heard using a stethoscope or simply when breathing. Abnormal breath sounds can indicate a lung problem, such as: an obstruction inflammation an infection fluid in the lungs asthma Listening to breath sounds is an important part of diagnosing many different medical conditions.