Top videos
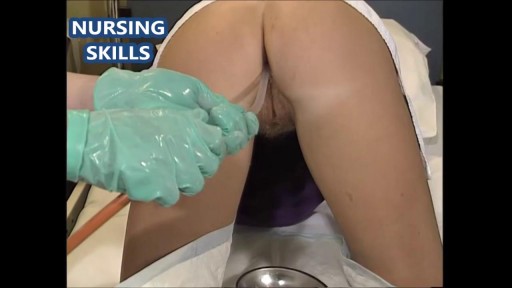
A digital rectal examination (DRE) is a simple procedure doctors use to examine the lower rectum and other internal organs. A DRE is done for a number of reasons. It's a quick, easy way to check the health of a man's prostate gland. It can detect conditions like an enlarged prostate

Patient Greg Grindley communicates with host Bryant Gumbel and his wife for the first time while undergoing deep brain stimulation surgery at University Hospital's Case Medical Center in Cleveland, Ohio.
➡ Subscribe: http://bit.ly/NatGeoSubscribe
About National Geographic:
National Geographic is the world's premium destination for science, exploration, and adventure. Through their world-class scientists, photographers, journalists, and filmmakers, Nat Geo gets you closer to the stories that matter and past the edge of what's possible.
Get More National Geographic:
Official Site: http://bit.ly/NatGeoOfficialSite
Facebook: http://bit.ly/FBNatGeo
Twitter: http://bit.ly/NatGeoTwitter
Instagram: http://bit.ly/NatGeoInsta
Greg's First In-Surgery Conversation | Brain Surgery Live
https://youtu.be/zvqV_2zncNU
National Geographic
https://www.youtube.com/natgeo

Most women have vaginal discharge at many different times throughout their cycle. During ovulation, white and watery discharge is common and accepted as normal. But, discharge after ovulation is widely believed to be a sign of pregnancy.
This video: Multiple myeloma is a cancer that forms in a type of white blood cell called a plasma cell. Plasma cells help you fight infections by making antibodies that recognize and attack germs. Multiple myeloma causes cancer cells to accumulate in the bone marrow, where they crowd out healthy blood cells. Rather than produce helpful antibodies, the cancer cells produce abnormal proteins that can cause kidney problems. Treatment for multiple myeloma isn't always necessary. If you're not experiencing signs and symptoms, you may not require treatment. If signs and symptoms develop, a number of treatments can help control your multiple myeloma.
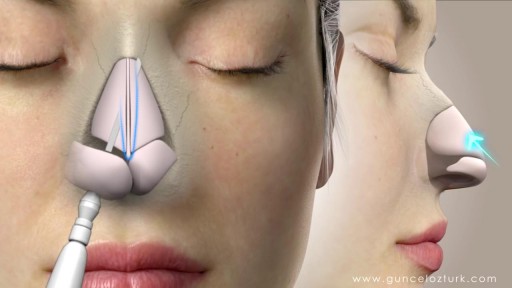
Rhinoplasty, sometimes referred to as a "nose job" or "nose reshaping" by patients, enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. What surgical rhinoplasty can treat Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone's face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion. Rhinoplasty to correct a deviated septum Nose surgery that's done to improve an obstructed airway requires careful evaluation of the nasal structure as it relates to airflow and breathing. Correction of a deviated septum, one of the most common causes of breathing impairment, is achieved by adjusting the nasal structure to produce better alignment.