Top videos

The colonoscope is slowly withdrawn during this screening colonoscopy down from the transverse colon, back around the splenic flexure, and down the descending colon, and reveals this finding a colonic diverticula. Diverticulosis is a common, acquired, age-related occurrence affecting over 50% of the... western adult population over the age of 50. It is seen rarely in Africa and Asia where the dietary fiber content is traditionally higher. Thus most investigators feel that low fiber diets are related to the development of this condition. Ironically, colonic diverticula are not true diverticula but rather pseudodiverticula in that the sac includes layers of the mucosa and submucosa that push through rather than include the outer muscular layer. As with the small bowel the colon has an inner circular muscular layer, but the outer longitudinal layer is composed of three bands of muscle that run the length of the colon known as teniae. Diverticula occur in rows between the mesenteric and two antimesenteric teniae where the colonic wall is further weakened by the defect caused by the perforating vasa recti artery which supplies the colonic mucosa. Occasionally, the anatomic propensity of diverticula to form in rows is quite apparent as seen when this clip is replayed in slow motion. Most often, however, the arrangement of the diverticula appears random due to the angulation of the bowel and thickening of the semi lunar folds. The conditions that cause these pulsion diverticula are not know with certainty but may include high intrahaustral pressures, muscular hypertrophy, and age related alterations in collagen cross linking. Diverticula can bleed or can abscess and perforate. The incidence of diverticulitis or diverticular bleeding is in the range of 1:1,000 patients with diverticulosis.

For benign colorectal diseases, totally laparoscopic left-sided colectomy was already reported on some papers. Nowadays, there is increasingly demanded minimally invasive surgerys on malignant bowel diseases including colorectal cancers and so we developed the new techniques in that specimen is del...ivered through the open rectal stump, especially, using Sani Sleeve(TM). In this operation video, you can see that an anvil was fixed to proximal colonic stump with intracorporeal purse-string suture using Endo-stitch(TM). (SETA : Specimen Extraction Through Anus)

Bilateral High flex knee replacements for British patient. 81 year old Ken Perris is highly satisfied after double flexible knee replacements in Chennai hospital by Orthopaedic surgeon Dr.A.K.Venkatachalam of www.kneeindia.com. High flex or flexible knee replacements confer the ability to kneel, squat, sit cross legged. Minimally invasive surgical approaches reduce pain and hasten recovery.
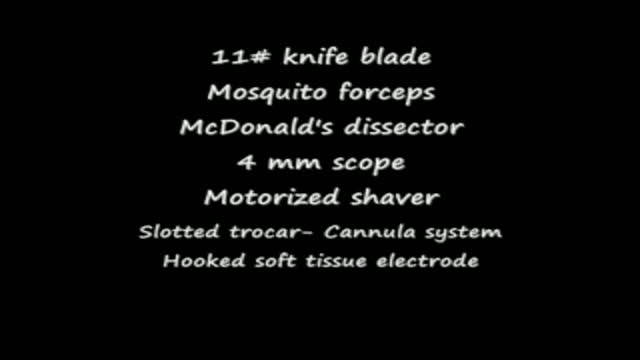
plantar fasciitis and calcaneal spur can be treated by EPFR with calcanean drilling - endoscopic plantar fascia release علاج الشوكة العظمية للكعب بالمنظار د. أسامة الشاذلي مدرس جراحة العظام واستشاري جراحات و مناظير القدم والكاحل كلية الطب جامعة عين شمس