Top videos

Here we’ll explain the symptoms of pancreatitis, how alcohol causes the condition and the other health problems it can lead to. You probably don’t pay much attention to your pancreas. But that small, tadpole-shaped organ behind your stomach and below your ribcage is pretty important. It produces two essential substances: digestive juices which your intestines use to break down food, and hormones that are involved in digestion, such as insulin, which regulates your blood sugar levels. Pancreatitis is when your pancreas becomes inflamed and its cells are damaged. Heavy drinking can cause pancreatitis. But if you drink within the government’s low risk unit guidelines, you should avoid upsetting this important organ.
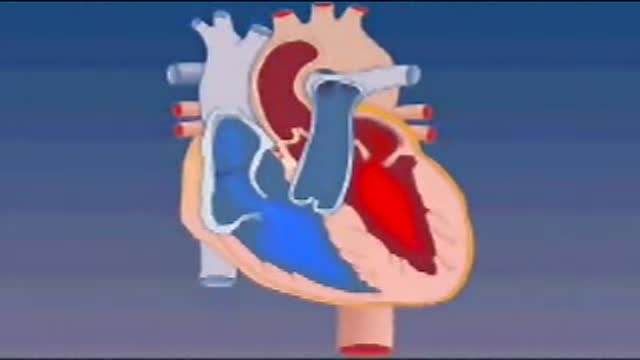
Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium. As the atrium contracts, blood flows from your right atrium into your right ventricle through the open tricuspid valve.

Surfactant. Surfactants are compounds that lower the surface tension (or interfacial tension) between two liquids or between a liquid and a solid. Surfactants may act as detergents, wetting agents, emulsifiers, foaming agents, and dispersants.

Physical assessment is taking an educated, systematic look at all aspects of an individual’s health status utilizing knowledge, skills and tools of health history and physical exam. To collect data- information about the client’s health, including physiological, psychological, sociocultural and spiritual aspects To establish actual and potential problems To establish the nurse-client relationship Method: The history is done first, then the physical examination focuses on finding data associated with the history. Health History- obtained through interview and record review. Physical exam- accomplished by tools and techniques ** A complete assessment is not necessarily carried out each time. A comprehensive assessment is part of a health screening examination. On admission, you will do an admission assessment (not necessarily including everything presented here) and document it on the admission form. You will do a daily shift assessment (patient systems review). And, if client has a specific problem, you may assess only that part of the body (focused). Data Collection: Information is organized into objective and subjective data: Subjective: Apparent only to person affected; includes client’s perceptions, feelings, thoughts, and expectations. It cannot be directly observed and can be discovered only asking questions. Objective: Detectable by an observer or can be tested against an acceptable standard; tangible, observable facts; includes observation of client behavior, medical records, lab and diagnostic tests, data collected by physical exam. ** To obtain data for the nursing health history, you must utilize good interview techniques and communications skills. Record accurately. DO NOT ASSUME. D. Frameworks for Health Assessment There are two main frameworks utilized in health assessment: Head to Toe- systematic collection of data starting with the head and working downward. Functional Health Assessment- Gordon’s 11 functional health patterns that address the behaviors a person uses to maintain health. PERSON is the ACC-ADN framework for assessment. It is similar to Gordon's functional health patterns.

A visual prosthesis, often referred to as a bionic eye, is an experimental visual device intended to restore functional vision in those suffering from partial or total blindness. In 1983 Joao Lobo Antunes, a Portuguese doctor, implanted a bionic eye in a person born blind.
The maneuver is commonly used during some activities: Straining to have a bowel movement Blowing a stuffy nose Certain medical tests or exams As a pressure equalization technique by scuba divers, sky divers and airplane passengers The effect of the Valsalva Maneuver is a drastic increase in the pressure within the thoracic cavity.

While an anal abscess is an infection within one or more of the anal spaces, an anal fistula (Choice B) is a tunneling between the anus or rectum and another epithelial lined space (eg, the skin overlying the drainage site). Fifty percent of patients with anal abscesses will go on to develop a chronic fistula from the involved anal gland to the overlying skin. Patients with fistulas typically present with an anal abscess that persists after incision and drainage, or with a pustule-like lesion in the perianal or ischiorectal area that continually drains. Surgical repair is usually necessary to eliminate the fistula while preserving fecal continence.

The fuel for the process leading to orgasm is testosterone, a hormone produced in steady supply by the testicles. The testicles also make millions of sperm each day, which mature and then are mixed with whitish, protein-rich fluids. These fluids nourish and support the sperm so they can live after ejaculation for a limited time. This mixture of fluid and sperm, known as semen, is what is moved through the urethra and out the penis during orgasm.

Hysteroscopy is a procedure that allows your doctor to look inside your uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.

Dilation and curettage (D&C) is a procedure to remove tissue from inside your uterus. Doctors perform dilation and curettage to diagnose and treat certain uterine conditions — such as heavy bleeding — or to clear the uterine lining after a miscarriage or abortion.