Top videos

The purpose of this video is to help you learn what to expect while you are in hospital, and how to care for yourself after surgery so that you can have the best recovery possible.
----------------------------------
At Horizon Health Network, we are helping people be healthy! Chez le Réseau de santé Horizon, nous aidons les gens à être en santé!
For more information, visit/Pour plus d'information, cliquez-ici:
https://news.horizonnb.ca
Facebook: https://facebook.com/HorizonNB
Twitter: https://twitter.com/HorizonHealthNB
Instagram: https://instagram.com/horizonhealthnb/
Linkedin: https://linkedin.com/company/h....orizon-health-networ

Watch this clinical examination video to learn how to diagnose inguinal related groin pain.
This video clip is part of the FIFA Diploma in Football Medicine and the FIFA Medical Network. To enrol or to find our more click on the following link http://www.fifamedicalnetwork.com
The Diploma is a free online course designed to help clinicians learn how to diagnose and manage common football-related injuries and illnesses. There are a total of 42 modules created by football medicine experts. Visit a single page, complete individual modules or finish the entire course.
The network provides the opportunity for clinicians around the world to meet and share ideas relating to football medicine. Ask about an interesting case, debate current practice and discuss treatment strategies. Create a profile and log on to interact with other health professionals from around the globe.
This is not medical advice. The content is intended as educational content for health care professionals and students. If you are a patient, seek care of a health care professional.

The MORE subscribers we have the MORE unintentional ASMR videos we can post, so please SUBSCRIBE http://bit.ly/UASMR, hit that 🔔 and LIKE this video for more medical exam ASMR like this! So... here is the BEST medical exam ASMR on YouTube edited specifically for unintentional ASMR to become the best video to help fall asleep at night. Our medical exam ASMR playlist: http://bit.ly/MedicalASMR
🔴 Support the channel and get access to extra perks by becoming a member here: https://www.youtube.com/channe....l/UCWCk81c_nQOsm5M-x
Try out the MOST comfortable sleep mask I've ever worn here ➜ https://bit.ly/MantaDiscount.
Prefer SOOTHING music for sleep? Here's what I use ➜ https://bit.ly/3lOPqe2
This hour long medical exam has a quiet doctor performing a routine medical exam with minimal talking. The video is 100% accidental ASMR and features a real doctor doing a head to toe assessment. This is honestly one of the best medical exam ASMR videos and on my all time favourite unintentional ASMR videos. This audio for this video has been significantly edited for maximum ASMR.
EXCLUSIVE: You can get 10% off any SleepPhones products with the code SLEEPNOW here: https://bit.ly/2YrrKQC
For the best unintentional ASMR and sleep aid videos we can't post here see http://ineedtosleepnow.com/
Medical ASMR: http://bit.ly/MedicalASMR
Female ASMR: http://bit.ly/FemaleASMR
Best of the best: http://bit.ly/BestUnintentionalASMR
Celeb ASMR: http://bit.ly/CelebASMR
Show and tell ASMR: http://bit.ly/ShowTellASMR
Relaxing interviews: http://bit.ly/InterviewsASMR
Original un-edited videos:
Part 1: https://youtu.be/S5tK3Ikb7ug
Part 2: https://youtu.be/m_-ALfUmmiA
WHAT IS UNINTENTIONAL ASMR?
https://ineedtosleepnow.com/what-is-u...
💤 For MORE of the Best (Intentional) ASMR videos on YouTube click here: https://goo.gl/mTsEBN
🙂 Finding, editing and uploading these videos does take some time and I try to upload a new video each night. If you find these videos useful, please consider supporting us by doing your Amazon shopping through our affiliate link: https://www.amazon.ca/shop/pur....eunintentionalasmrby
Best Microphone for recording ASMR: https://amzn.to/34WJhn2
▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬
WANT TO MAKE A RECOMMENDATION? Contact us via:
Facebook ► https://www.facebook.com/uASMR/
Twitter ► https://twitter.com/AccidentalASMR
Instagram ► https://www.instagram.com/pureunintentionalasmr/
See what's coming next by checking out our FB group: https://www.facebook.com/groups/1649835798657192/
🔴 In case this channel is removed, please subscribe to our newsletter for updates on new videos locations: http://eepurl.com/ds-orr. We will never email you about anything other than a new channel.
▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬
More of the Pure ASMR channels:
Pure ASMR: http://bit.ly/PureASMR and hit that 🔔.
Pure Unintentional ASMR 2: https://bit.ly/PureUASMR2
Pure Natural ASMR: http://bit.ly/NatureASMR
Pure Audiobook ASMR: http://bit.ly/AudiobookChannel
Purr ASMR: http://bit.ly/CatASMR
▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬
NOTE: This video is being shared for #unintentionalASMR reasons only. The video has been edited from its original format for this purpose.
WHAT IS ASMR? http://ineedtosleepnow.com/what-is-asmr
ASMR definition: http://ineedtosleepnow.com/asmr-definition-what-is-the-definition-for-asmr
http://iNeedToSleepNow.com is a YouTube channel and website that curates calm softly spoken voices that serve as great unintentional #ASMR. This channel focuses primarily on soft speaking, calm softly spoken voices, unintentional ASMR interviews, relaxing voices, ASMR tingles and anything that helps you sleep.
Disclaimer: Some of these links are affiliate links where this channel could earn a small commission if you make a purchase. Shopping through these links is a great way to support the channel so we can keep making more videos for you. Thanks!

Shoulder Clinical Examination - Medical School Clinical Skills - Dr Gill
Personally, I find the shoulder examination the most complex examination possibly as there are so many variations and special tests. Some of which overlap and some will relate specifically to a patients presentation.
Often in a medical school syllabus, only select special tests will be used. In this shoulder exam demonstration, we include the Hawkins-Kennedy Test looking for impingement. This is dovetailed with examination for bicipital tendonitis as this is another possible cause of impingement type symptoms.
This shoulder upper limb exam follows the standard "Look, Feel, Move" orthopaedic exam approach, and overall order as set out in MacLeods Clinical Examination
Watch further orthopaedic examinations for your OSCE revision:
The Spine Examination:
https://youtu.be/pJxMHa6SCgU
Knee Examination
https://youtu.be/oyKH4EYfJDM
Hip Joint Clinical Examination
https://youtu.be/JC9GKq5nSdQ
________
Please note that there is no ABSOLUTE way to perform a clinical examination. Different institutions and even clinicians will have differing degrees of variations - the aim is the effectively identify medically relevant signs.
However during OSCE assessments. Different medical schools, nursing colleges, and other health professional courses will have their own preferred approach to a clinical assessment - you should concentrate on THEIR marks schemes for your assessments.
The examination demonstrated here is derived from Macleods Clinical Examination - a recognized standard textbook for clinical skills.
#ShoulderExamination #ClinicalSkills #DrGill

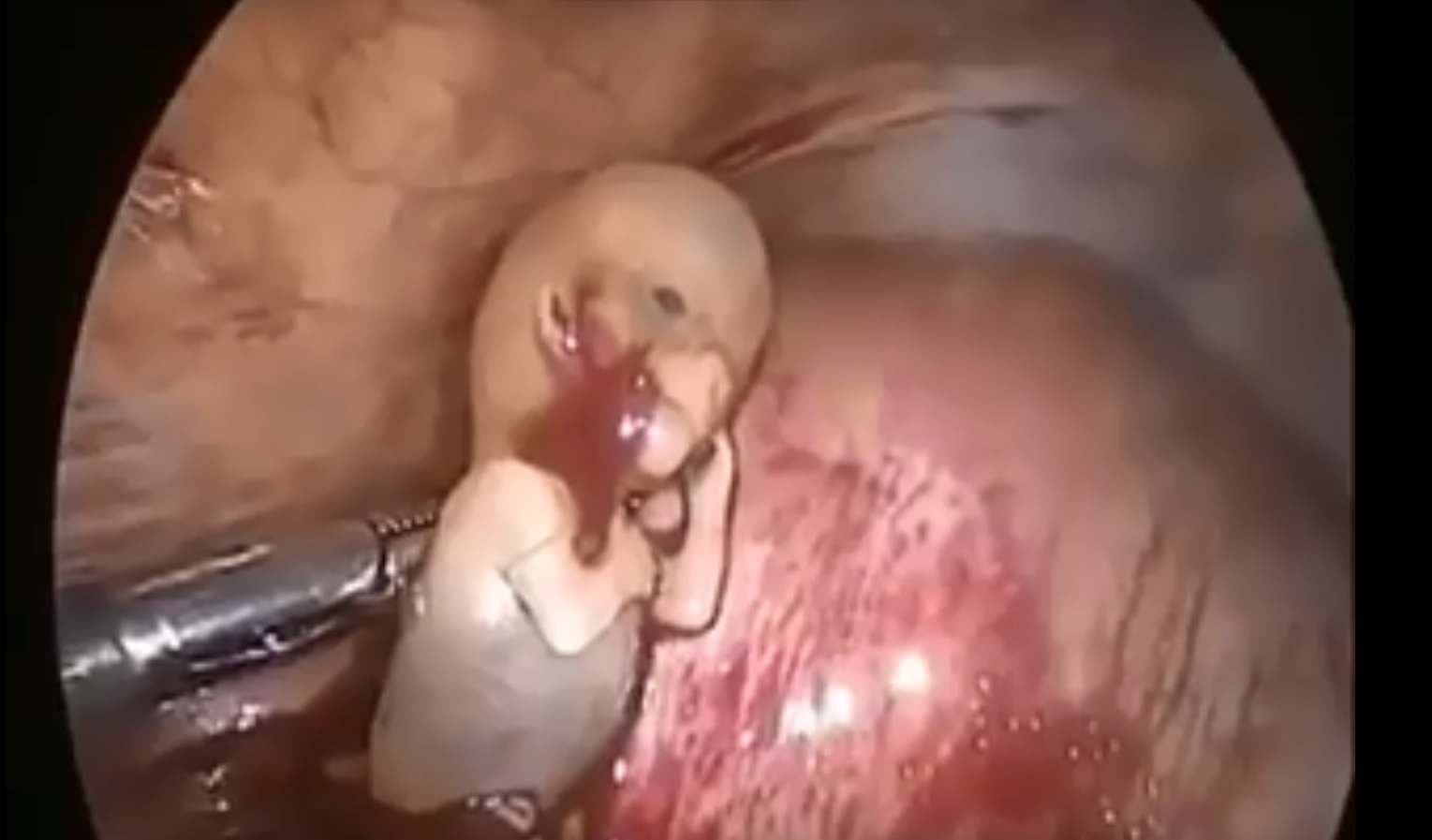
This is how Paraumbilical hernia looks like and how it is examined although it looks very simple but in exam it can be very difficult to perform all steps in small amount of time. This can be short case or even long of #cpsp #fcps #mbbs #medicalstudent #mbbsexams #plab2 #plab #plab1 and MS #genernalknowledge #surgery exams
#para-umbilical hernia
#umbilical hernia #paraumbilical #hernia repair#laparoscopic paraumbilical hernia repair. #umbilical defect, #vetral hernia surgery. #herniatreatment #herniatreatment #ventral hernia hernia,#laparoscopic ventral hernia repair,umbilicus,carl lowe jr,hernia repair,training,north carolina,hernia repair surgery,charlotte,operation,laparoscopic,bulge,surgery,surgeon,dr. lowe,ipom repair,live surgery,mesh,
#mesh #ipom repair
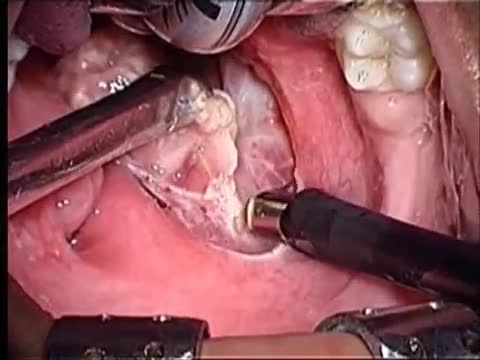
Tonsillectomy (ton-sih-LEK-tuh-me) is the surgical removal of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side. A tonsillectomy was once a common procedure to treat infection and inflammation of the tonsils (tonsillitis). Today, a tonsillectomy is usually performed for sleep-disordered breathing but may still be a treatment when tonsillitis occurs frequently or doesn't respond to other treatments. A tonsillectomy may also be necessary to treat breathing and other problems related to enlarged tonsils and to treat rare diseases of the tonsils.

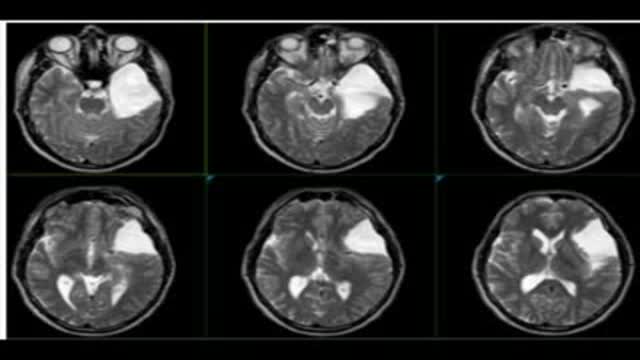
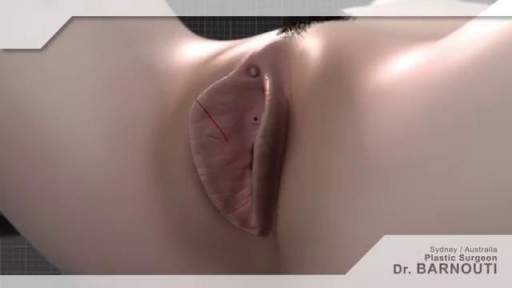
Urinary incontinence isn't a disease, it's a symptom. It can be caused by everyday habits, underlying medical conditions or physical problems. A thorough evaluation by your doctor can help determine what's behind your incontinence. Temporary urinary incontinence Certain drinks, foods and medications can act as diuretics — stimulating your bladder and increasing your volume of urine. They include: Alcohol Caffeine Decaffeinated tea and coffee Carbonated drinks Artificial sweeteners Corn syrup Foods that are high in spice, sugar or acid, especially citrus fruits Heart and blood pressure medications, sedatives, and muscle relaxants Large doses of vitamins B or C Urinary incontinence also may be caused by an easily treatable medical condition, such as: Urinary tract infection. Infections can irritate your bladder, causing you to have strong urges to urinate, and sometimes incontinence. Other signs and symptoms of urinary tract infection include a burning sensation when you urinate and foul-smelling urine. Constipation. The rectum is located near the bladder and shares many of the same nerves. Hard, compacted stool in your rectum causes these nerves to be overactive and increase urinary frequency. Persistent urinary incontinence Urinary incontinence can also be a persistent condition caused by underlying physical problems or changes, including: Pregnancy. Hormonal changes and the increased weight of the uterus can lead to stress incontinence. Childbirth. Vaginal delivery can weaken muscles needed for bladder control and also damage bladder nerves and supportive tissue, leading to a dropped (prolapsed) pelvic floor. With prolapse, the bladder, uterus, rectum or small intestine can get pushed down from the usual position and protrude into the vagina. Such protrusions can be associated with incontinence. Changes with age. Aging of the bladder muscle can decrease the bladder's capacity to store urine. Menopause. After menopause women produce less estrogen, a hormone that helps keep the lining of the bladder and urethra healthy. Deterioration of these tissues can aggravate incontinence. Hysterectomy. In women, the bladder and uterus are supported by many of the same muscles and ligaments. Any surgery that involves a woman's reproductive system, including removal of the uterus, may damage the supporting pelvic floor muscles, which can lead to incontinence. Enlarged prostate. Especially in older men, incontinence often stems from enlargement of the prostate gland, a condition known as benign prostatic hyperplasia. Prostate cancer. In men, stress incontinence or urge incontinence can be associated with untreated prostate cancer. But more often, incontinence is a side effect of treatments for prostate cancer. Obstruction. A tumor anywhere along your urinary tract can block the normal flow of urine, leading to overflow incontinence. Urinary stones — hard, stone-like masses that form in the bladder — sometimes cause urine leakage. Neurological disorders. Multiple sclerosis, Parkinson's disease, stroke, a brain tumor or a spinal injury can interfere with nerve signals involved in bladder control, causing urinary incontinence.

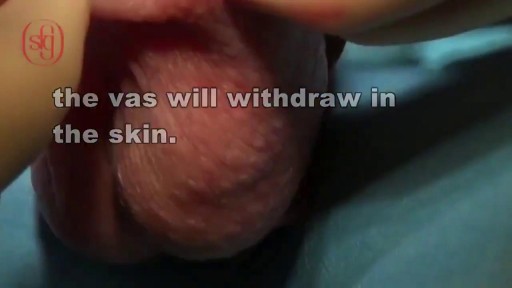
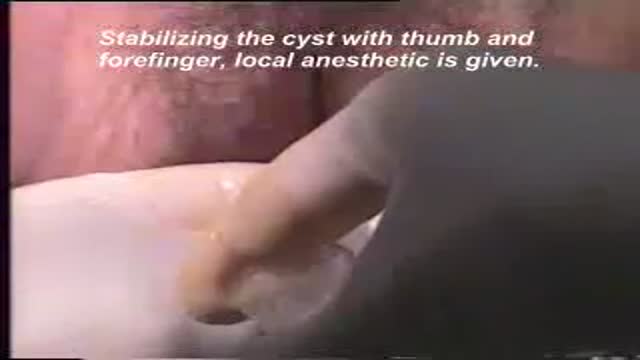
Identify the anatomy and explain the physiology of the scrotum on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the scrotum.
Identify and describe sonographic images of congenital abnormalities of the scrotum.
Identify and describe sonographic images of pathologies of the scrotum.
Identify and describe sonographic images of extratesticular disease processes.
Identify the anatomy and explain the physiology of the prostate on diagrams and sonograms.
Describe and demonstrate the protocol for transabdominal and endorectal sonographic scanning of the prostate.
Identify and describe sonographic images of benign and malignant pathologies of the prostate, including benign hyperplasia, prostatitis, carcinoma, and calculi.
Explain the technique for prostate biopsy.
Define the criteria for an ultrasound appearance of prostate tumor staging.
Explain the technique for radiation seed implantation.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).