Top videos

Colposcopy (kol-POS-kuh-pee) is a procedure to closely examine your cervix, vagina and vulva for signs of disease. During colposcopy, your doctor uses a special instrument called a colposcope. Your doctor may recommend colposcopy if your Pap test has shown abnormal results.

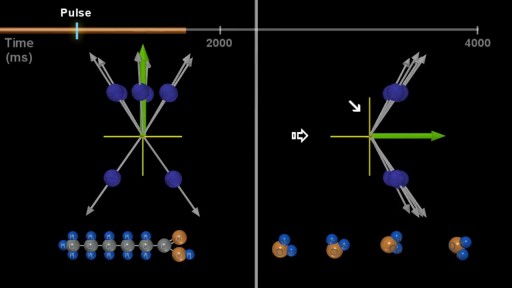
Hemodialysis is the process of cleaning the patient’s blood outside the body. Learn more about this renal replacement therapy option.
Read more: http://www.freseniusmedicalcar....e.com/en/patients-fa
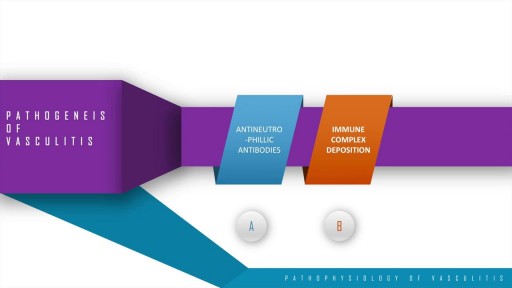
A step wise approach to the pathogenesis, types, disease entities and diagnosis of vasculitis. This discussion also includes the management options of vasculitis and their adverse drug reactions. In essence, vasculitis is a clfinicopathologic process characterised by inflammation and damage of blood vessels. This may be mainly due to three pathological processes which include immune complex deposition, anti-neutrophillic antibody formation and pathological T lymphocyte response and granuloma formation. The disease entities include Wegner's granulomatosis, Churg Strauss and many others. These present with palpable purpura, unexplained renal dysfunction etc which can be diagnosed based on biopsy and angiogram.

This video was taken 4 days after the surgery. This Patient had a facial rejuvenation procedure performed by Dr. Handal. He was exceptionally pleased with the results. Contact us for a consultation on how our team can help you to look better, (561) 912-9888. https://www.handalplasticsurgery.com

The Combitube is a twin lumen device designed for use in emergency situations and difficult airways. It can be inserted without the need for visualization into the oropharynx, and usually enters the esophagus. It has a low volume inflatable distal cuff and a much larger proximal cuff designed to occlude the oro- and nasopharynx.
If the tube has entered the trachea, ventilation is achieved through the distal lumen as with a standard ETT. More commonly the device enters the esophagus and ventilation is achieved through multiple proximal apertures situated above the distal cuff. In the latter case the proximal and distal cuffs have to be inflated to prevent air from escaping through the esophagus or back out of the oro- and nasopharynx.
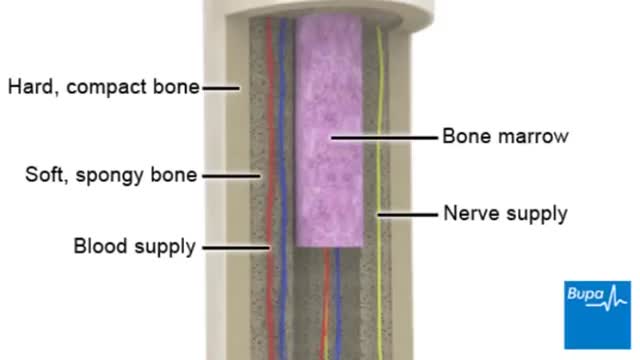
Osteoporosis is a disease in which bones become brittle and fragile due to low bone mass and bone tissue loss. It's the most common type of bone disease, according to the National Institutes of Health (NIH), and increases your risk of fractures, particularly of the hips, spine, and wrists. Prevalence In the United States, nearly 54 million people ages 50 and older were living with osteoporosis or osteopenia (low bone mass ) in 2010, according to a 2014 article in the Journal of Bone and Mineral Research. More specifically, 10.2 million adults had osteoporosis, and 43.4 million adults had osteopenia, which puts a person at high risk for osteoporosis.

http://www.mediplus.co.uk A new and safer method of inserting a Foley catheter suprapubically. The technique allows the insertion to be carried out in an Outpatient setting, thus saving time, cost and effort. By using the Seldinger technique, the product reduces the chances of bowel or bladder perforation and resultant morbidity.
The product has been chosen by The NHS National Technology Adoption Centre to help facilitate adoption of the product.
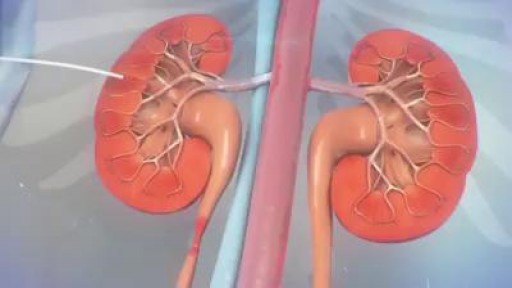
The ureter can become obstructed due to conditions such as kidney stones, tumors, infection, or blood clots. When this happens, physicians can use image guidance to place stents or tubes in the ureter to restore the flow of urine to the bladder. A ureteral stent is a thin, flexible tube threaded into the ureter.