Top videos

Dr Allen’s device provides a new kidney stones treatment that tackles the cause of kidney stone formation which is hidden at the capillary level, read at http://www.finetreatment.co.uk. The unique natural Thermobalancing Therapy does not use harmful medication or shock waves and, of course, surgery. Learn by watching this video about kidney stones cause and how to dissolve kidney stone or kidney stones at home by using Dr Allen’s natural therapeutic device.
ormal sperm densities range from 15 million to greater than 200 million sperm per milliliter of semen. You are considered to have a low sperm count if you have fewer than 15 million sperm per milliliter or less than 39 million sperm total per ejaculate.

The surgical procedure uses your own fat, so it is the most natural way to augment your buttocks. Over the last few years, the buttocks have received more press coverage than ever before. People of all ages and body types are having the Brazilian Butt Lift procedure.
How To Help Your Child Learn To Read, Help My Child Learn To Read, Best Way To Teach Reading---- http://children-learning-reading.good-info.co -- how to help your child learn to read - Help My Child Learn to Read The ability to read is vital for success. It helps your child succeed in school, helps them build self-confidence, and helps to motivate your child. Being able to read will help your child learn more about the world, understand directions on signs and posters, allow them to find reading as an entertainment, and help them gather information. Learning to read is very different from learning to speak, and it does not happen all at once. There is a steady progression in the development of reading ability over time. The best time for children to start learning to read is at a very young age - even before they enter pre-school. Once a child is able to speak, they can begin developing basic reading skills. Very young children have a natural curiosity to learn about everything, and they are naturally intrigued by the printed texts they see, and are eager to learn about the sounds made by those letters. You will likely notice that your young child likes to look at books and thoroughly enjoys being read to. They will even pretend to behave like a reader by holding books and pretend to read them. As parents, you're the most important first step in your children's journey into the wonderful world of reading. It is up to you to create the most supportive environment that turns your child on to reading - such as reading aloud to them often during the day and before bedtime, and placing age appropriate books for children around the house, so that the child will have access to plenty of books. Reading often to your child will help develop their interest in books and stories, and soon they will want to read stories on their own. >>Teach your child to read and enable your child to become a fast and fluent reader! Click here to help your child learn to read http://children-learning-reading.good-info.co
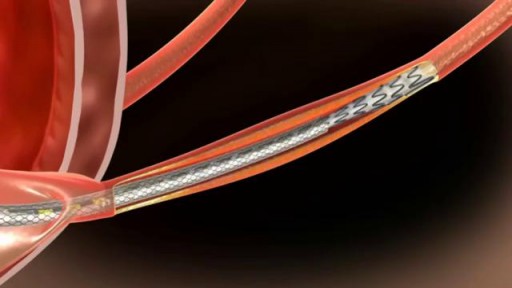
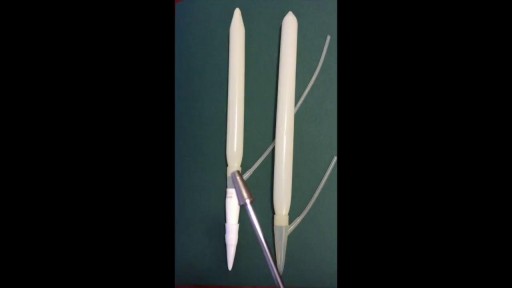
he Allium Ureteral Stents are intended for temporary long or short-term use in malignant or benign chronic Ureteral Stenosis. Allium Ureteral Stents are mounted on a ready to use 8 or 10Fr delivery system. By using the appropriate delivery system their deployment procedure can be performed either retrogradely or percutaneously. Indicated for all chronic ureteral stricturesLarge caliber for intra-lumenal flowLong dwelling timeAntegrade or retrograde insertionEasy insertion and stent positioningExcellent patient comfortNo tissue in-growthAnti-reflux designEasy removal of the device
http://www.HypothyroidismCure.blog300.com - Hypothyroidism Treatment Natural - Hypothyroidism Recipes Treatment
Let’s Get Something Straight…
* You’re here because you’re serious about overcoming your hypothyroidism…
* You’re here because you’re serious about and taking back your life…
* You know there’s no magic pill to cure your hypothyroidism and never will be…
Hypothyroidism Treatment Natural - Hypothyroidism Recipes Treatment
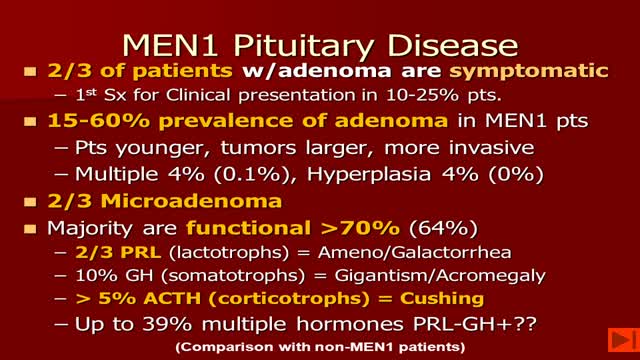
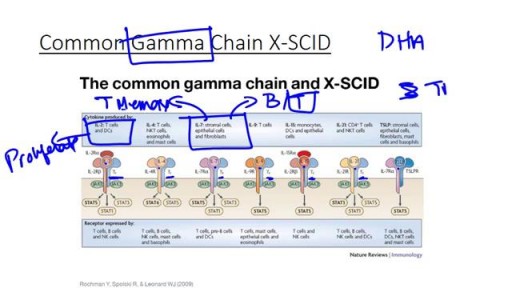
-MEN1 syndrome is composed of hyperparathyroidism, gastrinoma (pancreatic tumor) and pituitary tum or(remember the 3 Ps). Hyperparathyroidism in MEN1 is caused by hyperplasia of the parathyroid glands. Removal of 3 1/2 glands or total parathyroidectomy with autotransplantation is necessary.

If you’re like me, you probably hook your chest tube up to a Pleur-Evac, put it on the ground, then back away slowly. Who knows what goes on in that mysterious bubbling white box? Hopefully this will post shed some light. Isn’t this just a container for stuff that comes out of the chest? Why does it look so complicated? It’s complicated because the detection/collection of air and fluid require different setups. Most commercial models also allow you to hook the drainage system to wall suction, so you can quickly evacuate the pleural space. This requires its own setup. Because of the need to juggle air, fluid and suction, the most common commercial system includes 3 distinct chambers. If you were to simplify the device, or build one out of spare bottles and tubes, it might look like this:
Chronic obstructive pulmonary disease (COPD) is defined as progressive, chronic airflow obstruction due to chronic bronchitis, emphysema, or both. The majority of patients have components of both, although one of these entities will frequently dominate the clinical picture. Emphysema�airspace enlargement distal to the terminal bronchioles due to destruction of alveolar septa. Chronic bronchitis�chronic airway inflammation and bronchospasm. Clinically defined as productive cough lasting for at least 3 mo over 2 consecutive years. Although COPD is irreversible, patients with acute exacerbations do have reversible bronchospastic and inflammatory components.