Top videos

Furosemide is used to reduce extra fluid in the body (edema) caused by conditions such as heart failure, liver disease, and kidney disease. This can lessen symptoms such as shortness of breath and swelling in your arms, legs, and abdomen. This drug is also used to treat high blood pressure. Lowering high blood pressure helps prevent strokes, heart attacks, and kidney problems. Furosemide is a "water pill" (diuretic) that causes you to make more urine. This helps your body get rid of extra water and salt.
on bald hair loss man at 408-356-8600 by Dr. Diep with photos, of middle eastern man, Asian, Caucasian, Hispanic & Black, most advance hair treatment, treating male pattern baldness, bald head hair loss, receding hairline.

You may have heard that some positions, such as your partner on top (missionary position), are better than others for getting pregnant. In fact, there's no evidence to back these theories up. Experts just haven't done the research yet. What experts have done, though, is use scanning to show what's going on inside when you're doing the deed. The research looked at two positions: the missionary position and doggy style. (Doggy style being when you're on all fours, and your partner enters you from behind). Common sense tells us that these positions allow for deep penetration. This means that they're more likely to place sperm right next to your cervix (the opening of your uterus). The scans confirm that the tip of the penis reaches the areas between the cervix and vaginal walls in both of these positions. The missionary position allows the penis to reach the area at the front of the cervix. The rear entry position reaches the area at back of the cervix. It's amazing what some experts spend their time doing, isn't it! Other positions, such as standing up, or woman on top, may be just as good for getting sperm right next to the cervix. We just don't know yet. So, in the meantime, enjoy some variety in your sex life and keep it fun while you're trying for a baby. And talk to others who are hoping to get pregnant by joining our Actively trying group. Do I have to have an orgasm to conceive? Obviously, it's very important for your partner to reach orgasm if you are trying for a baby. There is no evidence, however, that you need to orgasm to conceive. The female orgasm is all about pleasure and satisfaction. It doesn't really help to get the sperm to the egg. Gentle contractions in your uterus can help the sperm along, but these happen without you having an orgasm. So, it's really not vital for you to reach orgasm after your partner, or even to reach orgasm at all, for you to conceive.
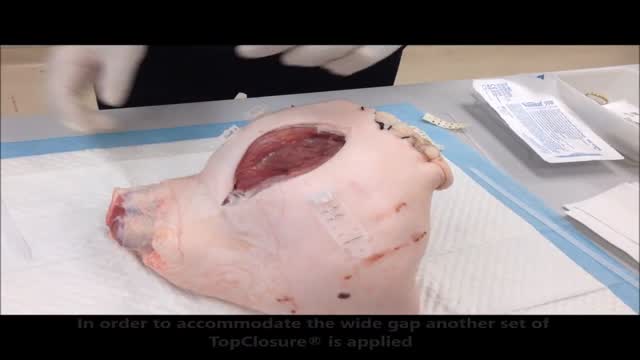
Stress-relaxation is a well-established mechanism for laboratory skin stretching, with limited clinical application in conventional suturing techniques due to the inherent, concomitant induction of ischemia, necrosis and subsequent suture failure. Skin defects that cannot be primarily closed are a common difficulty during reconstructive surgery. The TopClosure tension-relief system (TRS) is a novel device for wound closure closure, providing secured attachment to the skin through a wide area of attachment, in an adjustable manner, enabling primary closure of medium to large skin defects. The aim of this study was to evaluate the efficiency of the TopClosure TRS as a substitute for skin grafting and flaps for primary closure of large soft tissue defects by stress-relaxation. We present three demonstrative cases requiring resection of large to huge tumors customarily requiring closure by skin graft or flaps. TRS was applied during surgery serving as a tension-relief platform for tension sutures, to enable primary skin-defect closure by cycling of stress-relaxation, and following surgery as skin-secure system until complete wound closure. All skin defects ranging from 7 to 26 cm in width were manipulated by the TRS through stress-relaxation, without undermining of skin, enabling primary skin closure and eliminating the need for skin grafts and flaps. Immediate wound closure ranged 26 to 135 min. TRS was applied for 3 to 4 weeks. Complications were minimal and donor site morbidity was eliminated. Surgical time, hospital stay and costs were reduced and wound aesthetics were improved. In this case series we present a novel technology that enables the utilization of the viscoelastic properties of the skin to an extreme level, extending the limits of primary wound closure by the stress-relaxation principle. This is achieved via a simple device application that may aid immediate primary wound closure and downgrade the complexity of surgical procedures for a wide range of applications on a global scale.

Dr Allen’s device provides a new kidney stones treatment that tackles the cause of kidney stone formation which is hidden at the capillary level, read at http://www.finetreatment.co.uk. The unique natural Thermobalancing Therapy does not use harmful medication or shock waves and, of course, surgery. Learn by watching this video about kidney stones cause and how to dissolve kidney stone or kidney stones at home by using Dr Allen’s natural therapeutic device.
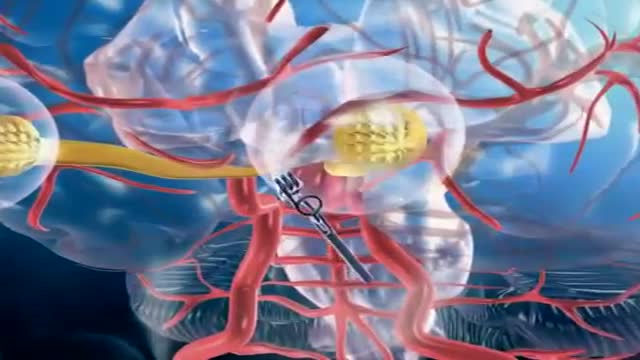
A brain (cerebral) aneurysm is a bulging, weak area in the wall of an artery that supplies blood to the brain. In most cases, a brain aneurysm causes no symptoms and goes unnoticed. In rare cases, the brain aneurysm ruptures, releasing blood into the skull and causing a stroke. When a brain aneurysm ruptures, the result is called a subarachnoid hemorrhage. Depending on the severity of the hemorrhage, brain damage or death may result. The most common location for brain aneurysms is in the network of blood vessels at the base of the brain called the circle of Willis. What causes a brain aneurysm? A person may inherit the tendency to form aneurysms, or aneurysms may develop because of hardening of the arteries (atherosclerosis) and aging. Some risk factors that can lead to brain aneurysms can be controlled, and others can't. The following risk factors may increase your risk for an aneurysm or, if you already have an aneurysm, may increase your risk of it rupturing: Family history. People who have a family history of brain aneurysms are more likely to have an aneurysm than those who don't. Previous aneurysm. People who have had a brain aneurysm are more likely to have another. Gender. Women are more likely to develop a brain aneurysm or to suffer a subarachnoid hemorrhage. Race. African Americans are more likely than whites to have a subarachnoid hemorrhage. High blood pressure. The risk of subarachnoid hemorrhage is greater in people who have a history of high blood pressure. Smoking. In addition to being a cause of high blood pressure, the use of cigarettes may greatly increase the chances of a brain aneurysm rupturing.
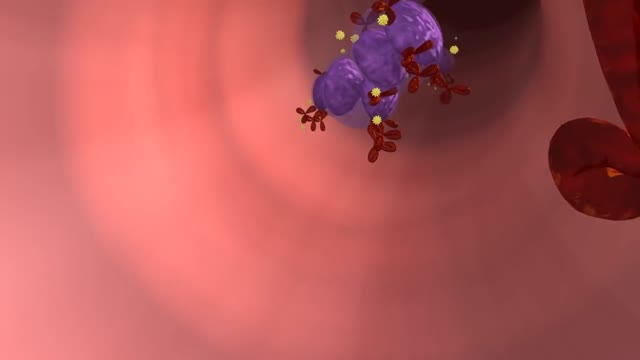
In multiple sclerosis, the immune system attacks the protective sheath called myelin, that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause the nerves to deteriorate or become damaged.