Top videos
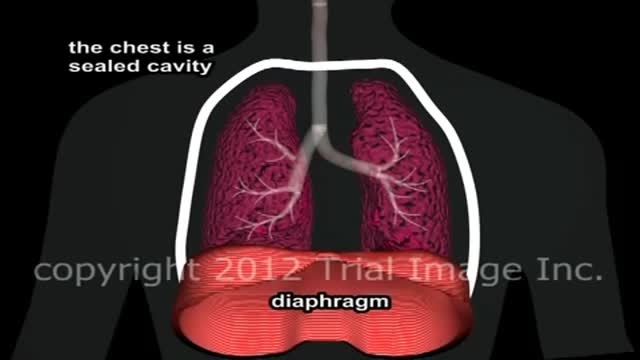
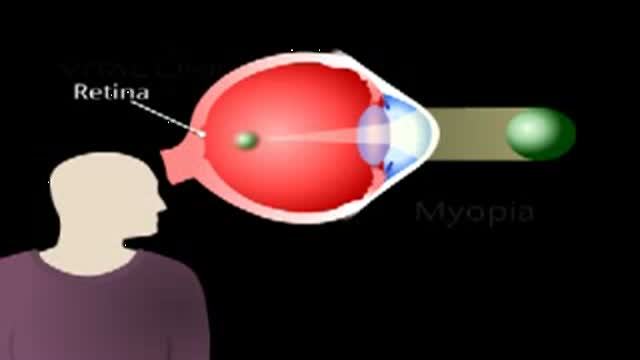
Pulmonary edema Email this page to a friend Email this page to a friend Facebook Twitter Google+ Pulmonary edema is an abnormal buildup of fluid in the lungs. This buildup of fluid leads to shortness of breath. Causes Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs. As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs. This fluid reduces normal oxygen movement through the lungs. These two factors combine to cause shortness of breath.

Symptoms Of Anxiety, Anxiety Disorder Symptoms, What Is Social Anxiety, Zoloft For Anxiety --- http://panic-attacks-anxiety.good-info.co --- Panic attacks and anxiety While there are times for doctors, I want you to consider this: MOST of your anxiety is under the radar… Masquerading as “just feeling a bit nervous”... or “just a tad irritable thanks to this diet plan”... or, “let’s skip the party and just stay home tonight.” And, I’m telling you, that anxiety not only destroys your fat burning power: It often leads to all-out panic disorder, if you just ignore it. Fortunately for you, there’s a 60-Second Solution that restores your calm, removes those anxious feelings, and allows you to keep burning body fat for energy. Now, this exact same technique works for all-out panic and even more serious anxiety issues, too… The man who delivers this presentation had panic attacks in “everyday” situations… and he too had feelings of anxiety whenever he tried to diet-off body fat… This Simple Trick Stops Panic Attacks And Anxiety Click Here: http://panic-attacks-anxiety.good-info.co

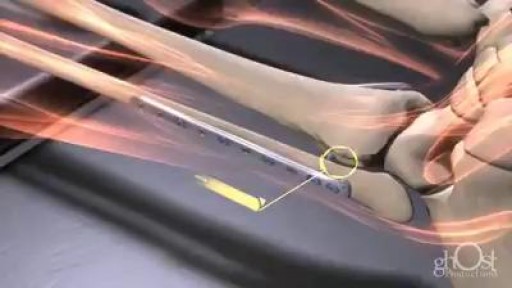
IV cannulation is a skill that has scared a lot of student nurses and even professionals. Perhaps it’s because IV insertion is an invasive procedure, and nurses are too worried that they might hurt their patients. Or maybe it’s because they are just clueless about IV therapy do’s and don’ts–things that one can only fully understand through constant practice.
Key facts
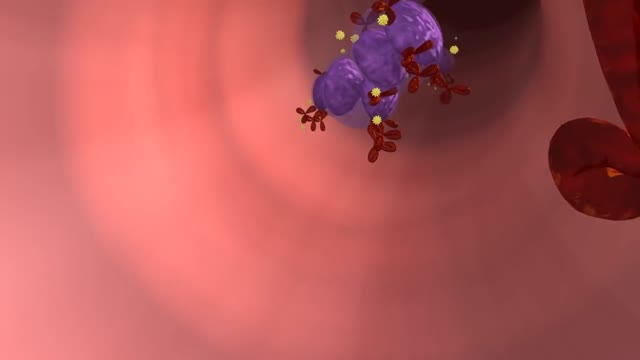
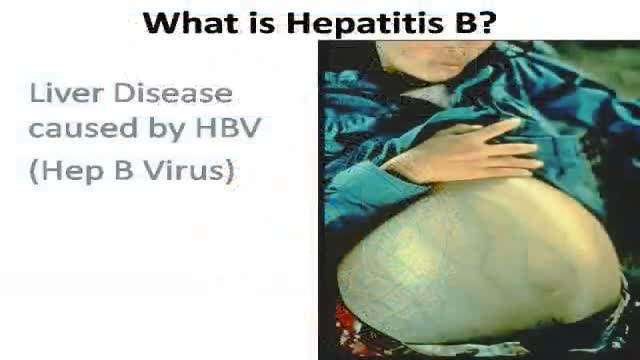
Hepatitis B is a viral infection that attacks the liver and can cause both acute and chronic disease.
The virus is transmitted through contact with the blood or other body fluids of an infected person - not through casual contact.
About 2 billion people worldwide have been infected with the virus and about 350 million live with chronic infection. An estimated 600 000 persons die each year due to the acute or chronic consequences of hepatitis B.
About 25% of adults who become chronically infected during childhood later die from liver cancer or cirrhosis (scarring of the liver) caused by the chronic infection.
The hepatitis B virus is 50 to 100 times more infectious than HIV.
Hepatitis B virus is an important occupational hazard for health workers.
Hepatitis B is preventable with a safe and effective vaccine.
-----------------------------------
Hepatitis B is a potentially life-threatening liver infection caused by the hepatitis B virus. It is a major global health problem and the most serious type of viral hepatitis. It can cause chronic liver disease and puts people at high risk of death from cirrhosis of the liver and liver cancer.
Worldwide, an estimated two billion people have been infected with the hepatitis B virus (HBV), and more than 350 million have chronic (long-term) liver infections.
A vaccine against hepatitis B has been available since 1982. Hepatitis B vaccine is 95% effective in preventing HBV infection and its chronic consequences, and is the first vaccine against a major human cancer.

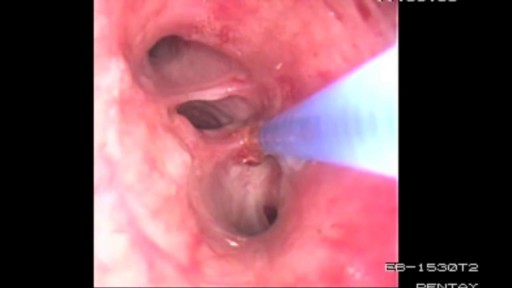
http://barretts-esophagus-cure.info-pro.co Barrett's Esophagus, Barrett's Esophagus Metaplasia, Barrett's Esophagus Bulimia. Are you lost, scared, frustrated, or confused? Have you been recently diagnosed with Barrett’s? Maybe your loved one or a close family member is now a victim of this painful disease. If so, I’d like to share with you some possibly life changing information on how I personally cured my own Barrett’s Esophagus. But before I do I’d like you to take a deep breath, relax for a moment, and let your worry subside because. Even though the Society of Thoracic Surgeons has determined that people with Barrett’s Esophagus are 40x’s more likely to get esophageal cancer, this diagnosis isn’t always a death sentence. Having been a victim of Barrett’s myself, I can relate to the excruciating pain this disease can cause. Maybe you’re like I was, trying to hide the symptoms when the burning, the heartburn, and the PAIN would become so unbearable I’d try doing anything to block it out. I can clearly recall the feeling of those scorching corroding acids inside my throat that would burn like fire, tearing up my esophagus from the inside out. It’s a pain I will NEVER forget. For me, maybe like you, many of my days were spent in anguish and painful agony. Barrett’s Reversed Without Surgery, Pills, PPI Pumps, Antacids, or Drugs. Clicking Here http://barretts-esophagus-cure.info-pro.co

Michigan Medicine’s Cardiac Surgery Simplified series highlights a multitude of surgical procedures in order to educate patients, healthcare providers, and trainees interested in learning about cardiac surgery performed at the Frankel Cardiovascular Center.
Like and subscribe to our channel to learn more about our pioneering procedures including minimally invasive valve surgery and safer methods to repair aortic aneurysms and dissections.
To learn more about cardiac surgery at Michigan Medicine, visit: https://medicine.umich.edu/dept/cardiac-surgery
To learn more about Frankel Cardiovascular Center, visit: https://www.umcvc.org/
To watch the full playlist, visit: https://www.youtube.com/playli....st?list=PLNxqP-XbH8B
-------------------------------------------------------
Subscribe to Michigan Medicine’s YouTube channel for upcoming videos and future live streams featuring our experts answering your questions.
-------------------------------------------------------
Follow Michigan Medicine on Social:
Twitter: https://twitter.com/umichmedicine
Instagram: https://www.instagram.com/umichmedicine/
Facebook: https://www.facebook.com/MichiganMedi...
Follow the U-M Frankel Cardiovascular Center on Social:
Twitter: https://twitter.com/umichcvc
Facebook: https://www.facebook.com/Universityof...
#MichiganMedicine #MedEd #CardiacSurgery #UniversityOfMichiganHealth #FrankelCardiovascularCenter #Cardiology
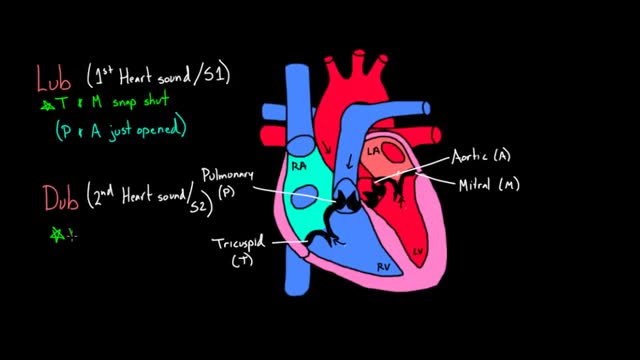
The heart and circulatory system (also called the cardiovascular system) make up the network that delivers blood to the body's tissues. With each heartbeat, blood is sent throughout our bodies, carrying oxygen and nutrients to all of our cells.