Top videos
A detailed description of the Hepato-pulmonary syndrome including its definition, pathophysiology, diagnosis and treatment. The pathophysiology includes nitric oxide in the pulmonary vasculature which results in intrapulmonary vasodilatation. This causes the classical and unique symptom of platypnea and orthodeoxia.
http://eliminar-celulite.plus101.com -- Como Tirar Celulite, Como Acabar Com A Celulite Das Pernas, Como Tirar Celulite Das Coxas. Esses 5 fatores contêm o segredo para conhecer algumas das causas dos furinhos, caroços e cavidades nas regiões problemáticas e pontos críticos da mulher comum. 1 – Muito Stress pode Causar Celulite ou Piorá-la Grande parte das mulheres nem ao menos sabe pelo nível de stress que elas têm passado em tempo integral. O ritmo da vida e sociedade moderna e a sobrecarga de fontes naturais estimulantes externas causa hiperatividade subconsciente. Isso se manifesta em vários níveis de preocupação, desassossego e uso desnecessário de energia mental e emocional. Mas pegue isso e adicione às ocorrências corriqueiras e intensas de stress que ocorrem em todas as nossas vidas em diversos momentos, em diferentes graus. Por exemplo: a doença de um ente querido, a morte de um amigo, divórcio, dificuldades no emprego, brigas familiares... Todos esses fatores de stress têm um impacto direto nos hormônios. Cortisol, epinefrina, e oxitocina, só para dar nome a alguns, são afetados pelo stress. Os níveis e frequência desses e de outros hormônios no corpo podem influenciar muitas características físicas. Uma delas sendo a sua integridade celular. Se as células de seu corpo estão sendo bombardeadas com níveis de hormônios que estão fora de sintonia, então os diversos resultados aparecerão. Músculos, tecido conectivo e células da pele ficarão moles, fracos e flácidos. Isto pode inclusive acontecer com mulheres que estão dando o seu melhor com exercícios e nutrição apropriados. Confira o vídeo abaixo e saiba como: http://eliminar-celulite.plus101.com
Key facts
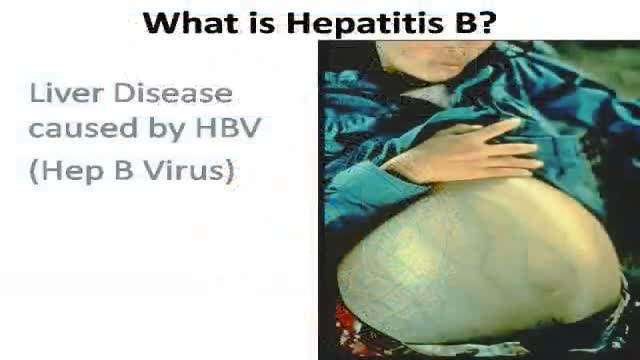
Hepatitis B is a viral infection that attacks the liver and can cause both acute and chronic disease.
The virus is transmitted through contact with the blood or other body fluids of an infected person - not through casual contact.
About 2 billion people worldwide have been infected with the virus and about 350 million live with chronic infection. An estimated 600 000 persons die each year due to the acute or chronic consequences of hepatitis B.
About 25% of adults who become chronically infected during childhood later die from liver cancer or cirrhosis (scarring of the liver) caused by the chronic infection.
The hepatitis B virus is 50 to 100 times more infectious than HIV.
Hepatitis B virus is an important occupational hazard for health workers.
Hepatitis B is preventable with a safe and effective vaccine.
-----------------------------------
Hepatitis B is a potentially life-threatening liver infection caused by the hepatitis B virus. It is a major global health problem and the most serious type of viral hepatitis. It can cause chronic liver disease and puts people at high risk of death from cirrhosis of the liver and liver cancer.
Worldwide, an estimated two billion people have been infected with the hepatitis B virus (HBV), and more than 350 million have chronic (long-term) liver infections.
A vaccine against hepatitis B has been available since 1982. Hepatitis B vaccine is 95% effective in preventing HBV infection and its chronic consequences, and is the first vaccine against a major human cancer.
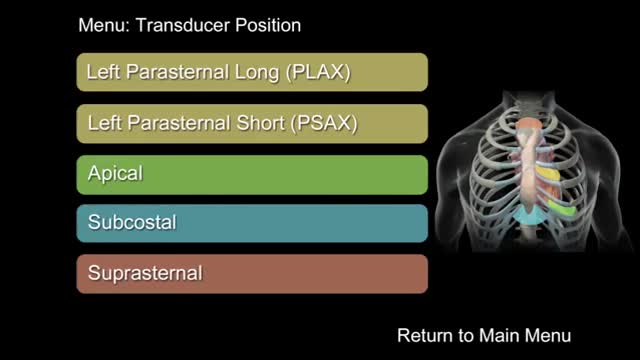
"How to Perform a Transthoracic Echocardiographic Study Volume 1: Transducer Position and Anatomy" is an instructional video, offered by ASE, and can be used for professional lectures and offers an interactive section for flexible presentations. The video includes an overview of relevant cardiac anatomy, a step by step presentation of all Transducer Positions, and the sequential transducer movements to acquire standard echo images needed to complete a Transthoracic Echocardiographic Study.

💥Patellar Tendon Pain AKA “Jumper’s Knee”👇
💥If you have this, it’s likely because your patellar tendon was over-stressed beyond what it can currently handle (due to loads that are too high or lack of recovery).
🔑 Try 5 reps of 45 second holds
🔑 2 min of rest in between each rep
🔑 Keep your knees at roughly 60 deg angle
🔑 7/10 intensity
🔑Should not increase pain during or after exercise
📚A research article found that this protocol using a knee extension machine provided significant short term pain relief. Most people don’t have a knee extension machine at home, so you could try out a wall sit instead!
🔑It may be useful during the season of competition to decrease pain and allow the athlete to compete, if needed.
❤️ Share this video with a friend who needs it!

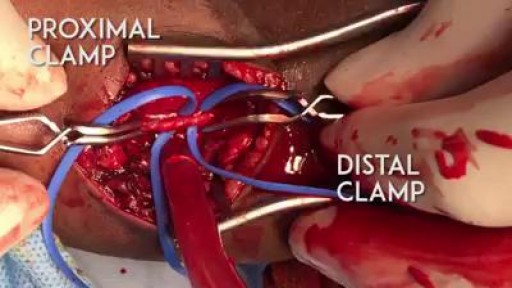
Follow one family's journey through the agony of waiting for a donor, a 31-hour surgery, and the prospect of a long road to recovery.
➡ Watch the full documentary here: https://youtu.be/fFua9-Rc4pw
➡ Access our digital archive by becoming a member of National Geographic: https://on.natgeo.com/39wAStK
#NationalGeographic #KatieStubblefield #FaceTransplant
About National Geographic:
National Geographic is the world's premium destination for science, exploration, and adventure. Through their world-class scientists, photographers, journalists, and filmmakers, Nat Geo gets you closer to the stories that matter and past the edge of what's possible.
Get More National Geographic:
Official Site: http://bit.ly/NatGeoOfficialSite
Facebook: http://bit.ly/FBNatGeo
Twitter: http://bit.ly/NatGeoTwitter
Instagram: http://bit.ly/NatGeoInsta
TikTok: http://www.tiktok.com/@natgeo
Tenor: http://on.natgeo.com/31b3Koc
To learn more, please read on here:
https://on.natgeo.com/2vQE1SO
Youngest Face Transplant Recipient in U.S. | National Geographic https://youtu.be/quU9s7I1NLI
National Geographic
https://www.youtube.com/natgeo

Can Birth Control Be a Dysmenorrhea Treatment? || Common gynaecological problems in women Dysmenorrhea is the medical term used for when you have painful menstrual cramps that occur immediately before or during your period. The pain can be so bad that it limits your daily activities. Dysmenorrhea is the most commonly reported menstrual disorder. It can affect up to 90 percent of young women. The Pill (as well as other hormonal contraceptives) can help in the treatment of dysmenorrhea.

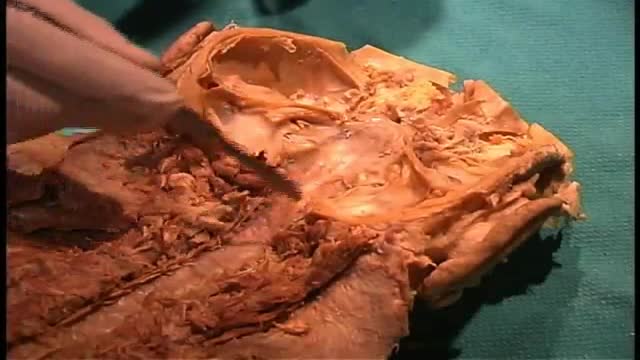
Syringomyelia is a cystic cavitation of the spinal cord associated with Chiari I malformation (70%) or basilar invagination (10%) or tumor. It may be a post-traumatic condition. There are 2 main forms: communicating with the central canal or subarachnoid spaces (Chiari I malformation); non communicating (trauma, tumors).