Top videos

What is Venipuncture? While venipuncture can refer to a variety of procedures, including the insertion of IV tubes into a vein for the direct application of medicine to the blood stream, in phlebotomy venipuncture refers primarily to using a needle to create a blood evacuation point. As a phlebotomist, you must be prepared to perform venipuncture procedures on adults, children, and even infants while maintaining a supportive demeanor and procedural accuracy. Using a variety of blood extraction tools, you must be prepared to respond to numerous complications in order to minimize the risk to the patient while still drawing a clean sample. In its entirety, venipuncture includes every step in a blood draw procedure—from patient identification to puncturing the vein to labeling the sample. Patient information, needle placement, and emotional environment all play a part in the collection of a blood sample, and it's the fine details that can mean the difference between a definite result and a false positive. After placing the tourniquet and finding the vein, it's time for the phlebotomist to make the complex choice on what procedure will best suit the specific situation. Keeping this in mind, it should be noted that the following information is not an instructional guide on how to perform these phlebotomy procedures. Rather, the information below is intended to serve as an educational resource to inform you of the equipment and procedures you will use. Venipuncture Technqiues Venipuncture with an Evacuated or Vacuum Tube: This is the standard procedure for venipuncture testing. Using a needle and sheath system, this procedure allows multiple sample tubes to be filled through a single puncture. This procedure is ideal for reducing trauma to patients. After drawing the blood, the phlebotomist must make sure the test stopper is correctly coded and doesn't contact exposed blood between samples. Venipuncture with a Butterfly Needle : This is a specialized procedure that utilizes a flexible, butterfly needle adaptor. A butterfly needle has two plastic wings (one on either side of the needle) and is connected to a flexible tube, which is then attached to a reservoir for the blood. Due to the small gauge of the needle and the flexibility of the tube, this procedure is used most often in pediatric care, where the patients tend to have smaller veins and are more likely to move around during the procedure. After being inserted into a vein at a shallow angle, the butterfly needle is held in place by the wings, which allow the phlebotomist to grasp the needle very close to the skin. Phlebotomists should be careful to watch for blood clots in the flexible tubing. Venipuncture with a Syringe: This technique is typically only used when there is a supply shortage, or when a technician thinks it is the appropriate method. It uses the classic needle, tube, and plunger system, operating in a similar manner to the vacuum tube but requiring multiple punctures for multiple samples. Additionally, after the blood is drawn it must be transferred to the appropriate vacuum tube for testing purposes. If you choose to use this method, remember to check for a sterile seal, and use a safety device when transferring the sample. Fingerstick (or Fingerprick): This procedure uses a medical lance to make a small incision in the upper capillaries of a patient's finger in order to collect a tiny blood sample. It is typically used to test glucose and insulin levels. When performing a Fingerstick, the phlebotomist should remember to lance the third or fourth finger on the non-dominant arm. Never lance the tip or the center of the finger pad; instead, lance perpendicular to the fingerprint lines. Heelstick (or Heelprick): Similar to the Fingerstick procedure, this process is used on infants under six months of age. A medical lance is used to create a small incision on the side of an infant's heel in order to collect small amounts of blood for screening. As with a Fingerstick, the incision should be made perpendicular to the heel lines, and it should be made far enough to the left or right side of the heel to avoid patient agitation. Before performing a Heelstick, the infant's heel should be warmed to about 42 degrees Celsius in order to stimulate capillary blood and gas flow. Therapeutic Phlebotomy: This involves the actual letting of blood in order to relieve chemical and pressure imbalances within the blood stream. Making use of a butterfly needle, this therapy provides a slow removal of up to one pint of blood. Though the blood removed is not used for blood transfusions, the procedure and concerns are the same as with routine blood donation. As with any phlebotomy procedure, one should pay close attention to the patient in order to prevent a blood overdraw. Bleeding Time: A simple diagnostic test that is used to determine abnormalities in blood clotting and platelet production. A shallow laceration is made, followed by sterile swabbing of the wound every 30 seconds until the bleeding stops. Average bleed times range between one and nine minutes. As a phlebotomist, you should familiarize yourself with the application and cross-application of these procedures in order to recognize when a procedure is necessary, and what the risks are for each.

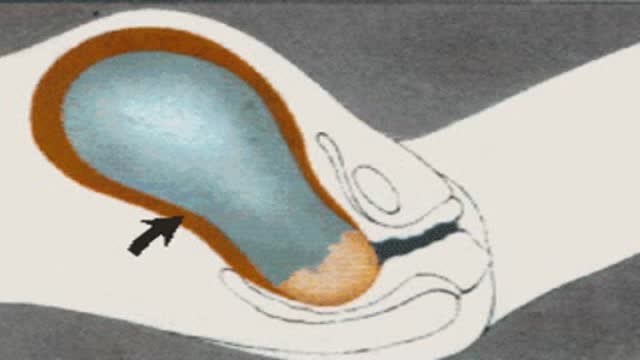
This patient presented to the ER for umbilical pain and had a history of umbilical hernia. He was concerned about the possibility of incarceration of the hernia.
In this video we explain how the clinical exam helps to differentiate a simple painful hernia from an incarcerated one.
***Thanks to the patient for sharing his history and exam with YouTube world***

http://penilepapules.plus101.com/ ----- White Spots On Shaft, Pearly Penile Papules Treatment Cream, Single Red Bump On Shaft, Ppp Surgery. Common Home Made Remedies for Pearly Penile Papules. When it comes to treating pearly penile papules many people find it very difficult to reach one of the medical treatments. This is mainly because they are highly expensive and not many people can afford spending large amounts of money on surgery and recovery. In addition to that, these procedures have been reported as being quite risky, which make the men suffering from pearly penile papules think twice before going for one of the available surgeries. This is why, along the time, many homemade, natural treatments have been experienced, so that a cheaper and less risky way of curing pearly penile papules would be found. Some of the methods which have been tried proved to be very less effective, while some did not have any effect at all. Yet, there have also been methods which not only proved to be effective, but they were also considered to be much better than the medical treatment. Most of those who have tried the tea tree oil treatment reported significant diminish of the number of the papules from their penises. In addition to the clearing of the skin, they have also noticed that there were no side effects and the skin remained soft after the papules were removed. As the method was quite simple to put in practice (it requires the application of tea tree oil on the affected area with a cotton swab for three or four times per day), many men decided this was indeed a great solution to their problem.
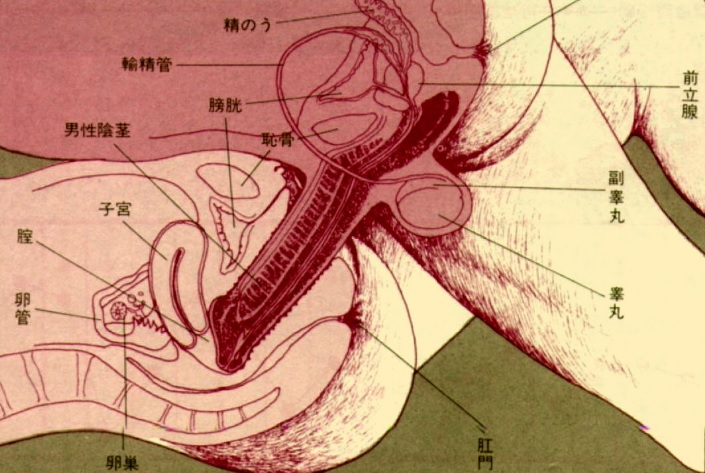
Childbirth (also called labour, birth, partus or parturition) is the culmination of a human pregnancy or gestation period with birth of one or more newborn infants from a woman’s uterus. The process of normal human childbirth is categorized in three stages of labour: the shortening and dilation of the cervix, descent and birth of the infant, and birth of the placenta. In some cases, childbirth is achieved through caesarean section, the removal of the neonate through a surgical incision in the abdomen, rather than through vaginal birth

A vaginoplasty is a surgical procedure that tightens the vagina. This is done by removing excess vaginal lining and tightening the surrounding soft tissues and muscles. During delivery of a baby the vagina and surrounding tissues and muscles become stretched. After delivery the vagina may return to a more “normal” size, but it often fails to return to its’ pre pregnancy diameter. Generally, the more vaginal deliveries, the worse the condition gets. Many women will complain of decreased sensation and sexual satisfaction during intercourse. Commonly this is due to a lack of friction. Often their partner may notice a change although he may say nothing. Kegel exercises are often recommended but rarely succeed in restoring vaginal tightness.

Best and 100% Successful Hymen Repair Surgery in Delhi with Latest Ultrafine Hymen repair Technology. 100% successful , Secure and Private. for more information visit: http://www.olmeccosmeticsurgery.com/best-hymenoplasty-surgery-india-delhi/
Urogenital neoplasms spreading to the inguinal lymph nodes are penile carcinoma (the most frequent), urethral and scrotum cancers, tumors of the testis with scrotal violation. Penile carcinoma is an uncommon malignant disease and accounts for as many 0.4-0.6% of male cancers. Most patients are elder...ly. It rarely occurs in men under age 60 and its incidence increases progressively until it reaches a peak in the eighth decade 1. The risk of a lymph node invasion is greater with high grade and high stage tumors 2. Some investigators have reported the inaccuracy of the sentinel node biopsy 3, 4, described by Cabanas 5. Patients with metastatic lymph node penis cancer have a very poor prognosis if penectomy only is performed. Ilioinguinal lymphadenectomy is basically carried out as a treatment modality and not only as a staging act. Patients with lymph node invasion have a 30-40% cure rate. Ilioinguinal lymphadenectomy should be also performed in patients with disseminated neoplasms for the local control of the disease. The 5 years survival rate of patients with clinically negative lymph nodes treated with a modified inguinal lymphadenectomy is 88% versus 38% in patients not initially treated with lymphadenectomy 6. This video-tape clearly shows a therapeutic algorithm, the anatomy of the inguinal lymph nodes, according to Rouviere 7 and Daseler 8, the radical ilioinguinal node dissection with transposition of the sartorius muscle and the modified inguinal lymphadenectomy proposed by Catalona 9. References: 1. Lynch D.F. and Schellhammer P: Tumors of the penis. In Campbell’s Urology Seventh Edition, edited by Walsh P.C., Retik A.B., Darracott Vaughan E. and Wein A.J. W.B. Saunders Company, Vol. 3, chapt. 79, p. 2458, 1998. 2. Pizzocaro G., Piva L., Bandieramonte G., Tana S. Up-to-date management of carcinoma of the penis. Eur. Urol. 32: 5-15, 1997 3. Perinetti E., Crane D.B. and Catalona W.J. Unreliability of sentinel lymph node biopsy for staging penile carcinoma. J. Urol. 124: 734, 1980 4. Fowler J.E. Jr. Sentinel lymph node biopsy for staging penile cancer. Urology 23: 352, 1984 5. Cabanas R.M. An approach for the treatment of penile carcinoma. Cancer 39: 456, 1977 6. Russo P. and Gaudin P. Management strategies for carcinoma of the penis. Contemporary Urology;5:48-66, 2000 7. Rouviere H. Anatomy of the human lymphatic system. Edwards Brothers, p. 218, 1938 8. Daseler E.H., Anson B.J., Reimann A.F. Radical excision of the inguinal and iliac lymph glands: a study based on 450 anatomical dissections and upon supportive clinical observations. Surg. Gynecol. Obstet. 87: 679, 1948 9. Catalona W.J. Modified inguinal lymphadenectomy for carcinoma of the penis with preservation of saphenous veins: technique and preliminary results. J. Urol. 140: 306-310, 1988
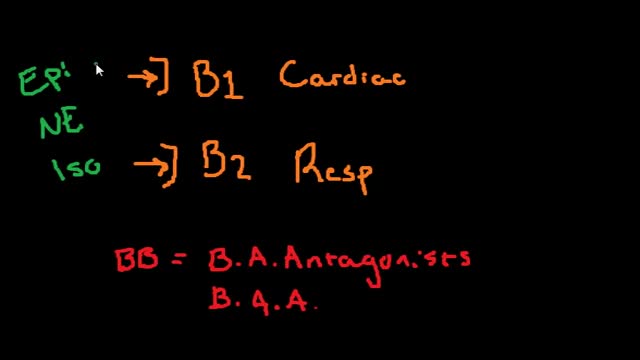
Beta blockers, also known as beta-adrenergic blocking agents, are medications that reduce your blood pressure. Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. When you take beta blockers, your heart beats more slowly and with less force, thereby reducing blood pressure. Beta blockers also help blood vessels open up to improve blood flow. Examples of beta blockers Some beta blockers mainly affect your heart, while others affect both your heart and your blood vessels. Which one is best for you depends on your health and the condition being treated. Examples of oral beta blockers include: Acebutolol (Sectral) Atenolol (Tenormin) Bisoprolol (Zebeta) Metoprolol (Lopressor, Toprol-XL) Nadolol (Corgard) Nebivolol (Bystolic) Propranolol (Inderal LA, InnoPran XL)