Top videos
For strong lungs, chew 3 to 5 peppermint leaves each day. To treat congestion, add a few drops of peppermint oil to a pot of hot water and inhale the steam. You can also drink 2 cups of peppermint tea daily. To make the tea, add 1 teaspoon of dried peppermint leaves to a cup of hot water.

The surgical procedure uses your own fat, so it is the most natural way to augment your buttocks. Over the last few years, the buttocks have received more press coverage than ever before. People of all ages and body types are having the Brazilian Butt Lift procedure.
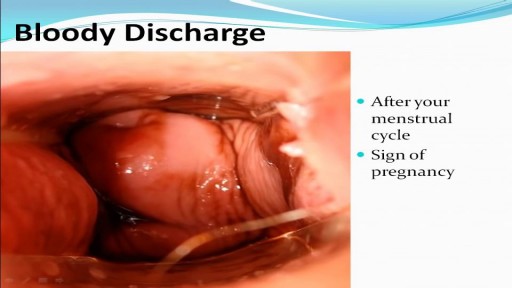
The anus is close to the vagina and sometimes it’s hard to say what’s going on inside the body. Is it possible to get pregnant from anal sex? The answer is yes and this video explains the circumstances. Please protect yourselves and stay curious.
Though the risk of HIV transmission through oral sex is very low, but several factors might increase the risk, including sores in the mouth or vagina or on the penis, bleeding gums, having an oral contact with menstrual blood, and the presence of other sexually transmitted diseases. But still the risk is low. by the way better to think twice before having the Oralsex with strangers. because you are not safe 100%.

ow does a perforation of the eardrum occur? There are many ways an eardrum perforation can occur. An infection behind the eardrum in the middle ear may cause a rupture of the eardrum. Trauma to the ear may result from an object entering the ear canal and puncturing the eardrum. A traumatic blow to the ear with a cupped hand can rupture the eardrum. Hot welding slag can burn a hole through the eardrum. After a ventilation tube has been extruded or is removed, the opening usually closes; in some cases a permanent opening of the eardrum may occur. Chronic ear problems such as deep retraction pockets and cholesteatoma can weaken and erode the eardrum, resulting in a defect or perforation.

The G-SHOT® (clinical description: G-Spot Amplification™ or GSA™), is a simple, nonsurgical, physician-administered treatment that can temporarily augment the Grafenburg spot (G-Spot) in sexually active women with normal sexual function.

There are lots of fallacies about the missionary position being the best position for getting pregnant. With the woman on her back and her partner on top, it is thought that gravity will assist the sperm to swim upwards towards the egg.

Identify the anatomy and explain the physiology of the breast on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the breast, including the clock and quadrant methods, and targeted examinations based on mammographic findings.
Describe the various diagnostic pathways that may lead to a sonographic breast examination, and explain how the ultrasound findings are correlated with other imaging modalities.
Identify and describe sonographic images of benign and malignant features and common breast pathologies.
Explain biopsy techniques for breast tumors.
Define and use related medical terminology.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference

Identify the anatomy and explain the physiology of the scrotum on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the scrotum.
Identify and describe sonographic images of congenital abnormalities of the scrotum.
Identify and describe sonographic images of pathologies of the scrotum.
Identify and describe sonographic images of extratesticular disease processes.
Identify the anatomy and explain the physiology of the prostate on diagrams and sonograms.
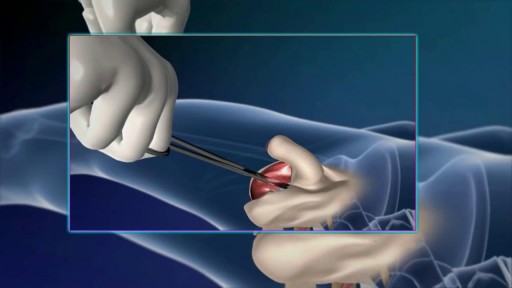
Describe and demonstrate the protocol for transabdominal and endorectal sonographic scanning of the prostate.
Identify and describe sonographic images of benign and malignant pathologies of the prostate, including benign hyperplasia, prostatitis, carcinoma, and calculi.
Explain the technique for prostate biopsy.
Define the criteria for an ultrasound appearance of prostate tumor staging.
Explain the technique for radiation seed implantation.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).