Top videos
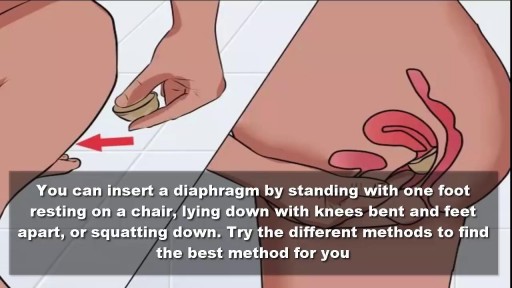
To use the diaphragm, first cover the inside of it with spermicide. Then insert it into your vagina so that it covers your cervix. You can insert the diaphragm up to 6 hours before sex. You should leave it in for at least 6 hours after the last time you have sex.

Detailed examination of the joints is usually not included in the routine medical examination. However, joint related complaints are rather common, and understanding anatomy and physiology of both normal function and pathologic conditions is critically important when evaluating the symptomatic patient. By gaining an appreciation for the basic structures and functioning of the joint, you'll be able to "logic" your way thru the exam, even if you can't remember the eponym attached to each specific test!
The venipuncture procedure is complex, requiring both knowledge and skill to perform. Each phlebotomist generally establishes a routine that is comfortable for her or him. Several essential steps are required for every successful collection procedure: Identify the patient. Assess the patient's physical disposition (i.e. diet, exercise, stress, basal state). Check the requisition form for requested tests, patient information, and any special requirements. Select a suitable site for venipuncture. Prepare the equipment, the patient and the puncture site. Perform the venipuncture. Collect the sample in the appropriate container. Recognize complications associated with the phlebotomy procedure. Assess the need for sample recollection and/or rejection. Label the collection tubes at the bedside or drawing area. Promptly send the specimens with the requisition to the laboratory.

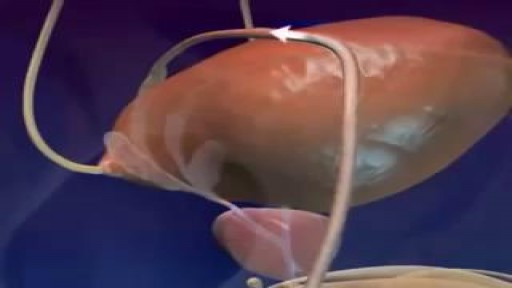
Each month inside your ovaries, a group of eggs starts to grow in small, fluid-filled sacs called follicles. Eventually, one of the eggs erupts from the follicle (ovulation). It usually happens about 2 weeks before your next period. Hormones Rise After the egg leaves the follicle, the follicle develops into something called the corpus luteum. The corpus luteum releases a hormone that helps thicken the lining of your uterus, getting it ready for the egg. The Egg Travels to the Fallopian Tube After the egg is released, it moves into the Fallopian tube. It stays there for about 24 hours, waiting for a single sperm to fertilize it. All this happens, on average, about 2 weeks after your last period.
Throughout the body, there are several points at which blood vessels unite. The junctions are termed anastomoses. In the simplest sense, an anastomosis is any connection (made surgically or occurring naturally) between tube-like structures. Naturally occurring arterial anastomoses provide an alternative blood supply to target areas in cases where the primary arterial pathway is obstructed. They are most abundant in regions of the body where the blood supply may can be easily damaged or blocked (such as the joints or intestines). This article focuses on the arterial anastomotic networks of the upper limb.

There are lots of fallacies about the missionary position being the best position for getting pregnant. With the woman on her back and her partner on top, it is thought that gravity will assist the sperm to swim upwards towards the egg.

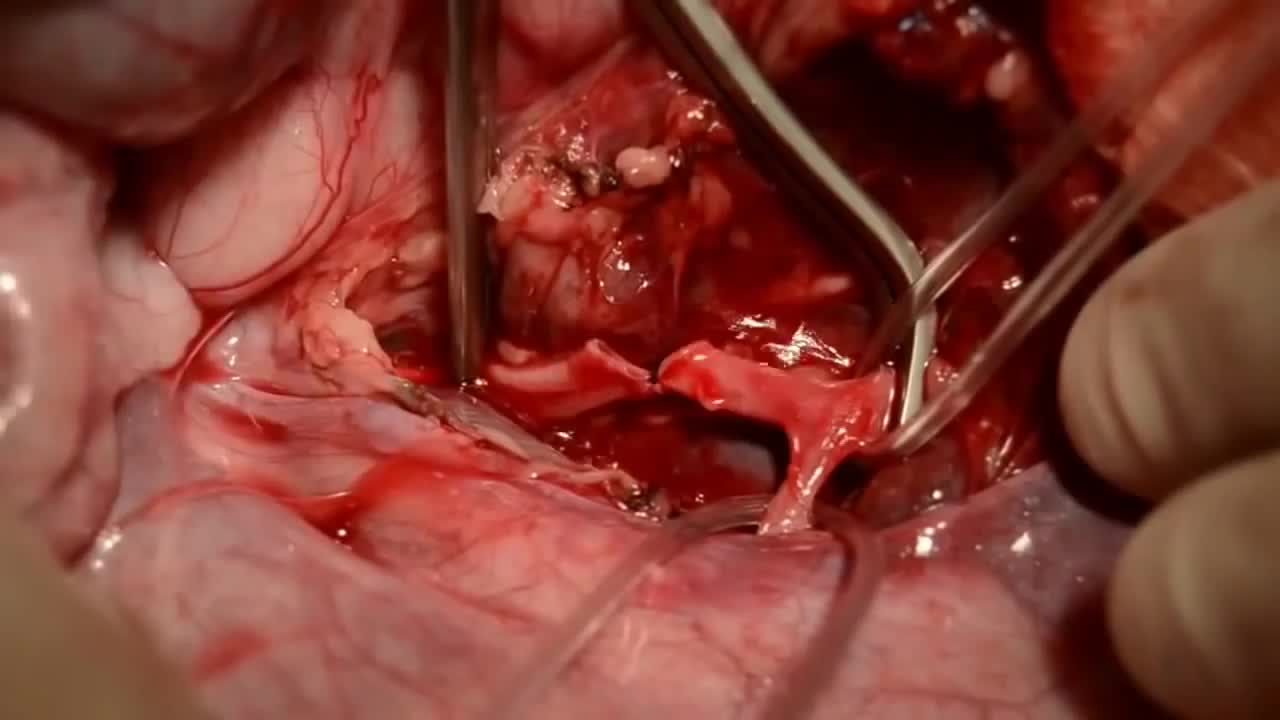
If the artery were severed, blood would flow out unimpeded, although the artery wall would contract in an effort to stop the bleeding. After losing >30% of one's blood volume blood pressure would start dropping, and with less pressure the rate of bleeding would go down. At this stage if the blood loss wasn't replaced the person could die. Losing halve to two thirds of one's blood volume is considered to be fatal even if later on blood transfusion is attempted. One's total blood volume at 70ml/kg is estimated to be between 5 to 7 liters, so that makes a blood loss of between 2,5 to 4,7 L.
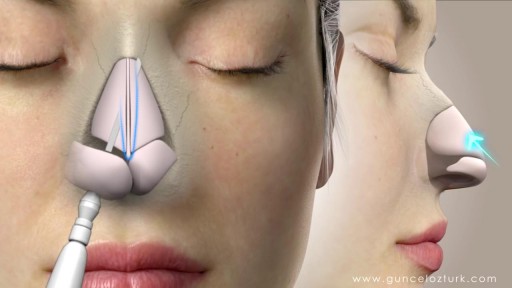
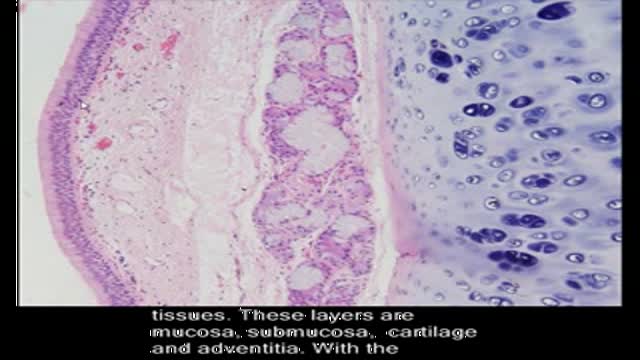
Rhinoplasty, sometimes referred to as a "nose job" or "nose reshaping" by patients, enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. What surgical rhinoplasty can treat Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone's face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion. Rhinoplasty to correct a deviated septum Nose surgery that's done to improve an obstructed airway requires careful evaluation of the nasal structure as it relates to airflow and breathing. Correction of a deviated septum, one of the most common causes of breathing impairment, is achieved by adjusting the nasal structure to produce better alignment.

Breast abscesses are often linked to mastitis – a condition that causes breast pain and swelling (inflammation), and usually affects women who are breastfeeding. Infections can occur during breastfeeding if bacteria enter your breast tissue, or if the milk ducts (tiny tubes) become blocked. This can cause mastitis which, if not treated, can result in an abscess forming. Women who aren't breastfeeding can also develop mastitis if bacteria enter the milk ducts through a sore or cracked nipple, or a nipple piercing. White blood cells are sent to attack the infection, which causes tissue at the site of the infection to die. This creates a small, hollow area that fills with pus (an abscess).
The male orgasm is a common subject but usually misunderstood at the same time. Men are sometimes led to believe that ejaculating often is a bad thing, particularly if you masturbate. The truth is that ejaculation is important to every man due to a number of reasons. The main goal of this post is to shed some light on reasons why men need to ejaculate.