Top videos
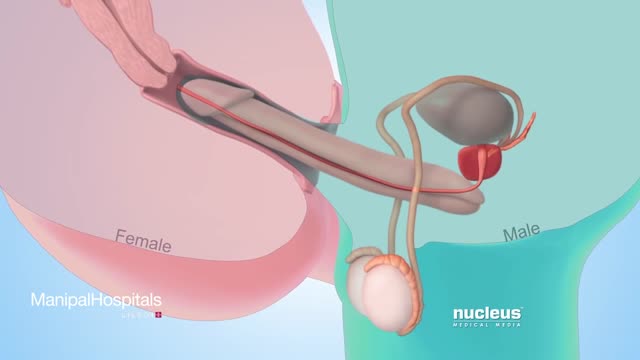
Testicular sperm aspiration (TESA) is a procedure performed for men who are having sperm retrieved for in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). It is done with local anesthesia in the operating room or office and is coordinated with their female partner's egg retrieval.
Que Es Bueno Para La Diabetes Medicina Natural. Porque Con Este Método Que Voy a Revelarte que es 10 Veces Más Efectivo Que Cualquier Otro Podrás Vencer A Tu Diabetes RÁPIDAMENTE. Si no hubiera sido por el poderoso método inusual pero PROBADO que usé para obtener RESULTADOS rápidos y controlar la diabetes. La genialidad de este gran descubrimiento es que está diseñado para controlar, frenar y vencer a la diabetes. con la “complicidad” de tu propio cuerpo que se auto regenera si se le instalan los comando correctos en el metabolismo. Sin importar si tienes 7 ó 90 años. Sin importar si tu nivel de azúcar es más incontrolable que un caballo salvaje, o tu tipo de diabetes. Sin importar cuantas veces tu doctor te ha dicho que la diabetes no tiene cura. Sin importar si has fallado una docena de veces con tratamientos, medicamentos o métodos convencionales que NO SIRVEN. Estás a punto de descubrir cómo controlar la diabetes usando la Solución Natural más exitosa jamás revelada que transformará tu cuerpo en una máquina generadora de salud y energía – ¡en tan solo unos pocos días! haciendo click aqui. http://vencer-la-diabetes-rapido.info-pro.co

Results Sinusitis was characterized as acute in 26 patients, subacute in 5 (including 1 pyocele), and chronic in 8 (including 2 fungal infections). No tumors were found. Isolated sinus cysts were excluded from the study. Headache, the main symptom in 32 patients (82%), was localized most commonly on the vertex. Other common complaints were rhinitis, dizziness, eye symptoms, and fever. In 2 patients, the finding was occult. Eight patients (21%) presented with cranial nerve deficits, and 1 patient had an intracranial complication. Sinus irrigation was performed in 16 patients (41%) and sphenoidotomy was performed in 10 (26%). Fifteen patients (38%) were treated with antibiotic drugs alone. Within 3 months, 31 (84%) of 37 patients had recovered from the illness; 5 still experienced headaches despite having normalized radiographic findings; and 1 had permanent unilateral visual loss. Two patients were lost to follow-up.

Virtual Ports, Ltd. (http://www.virtual-ports.com) is a medical device company developing and marketing instruments to improve minimally invasive laparoscopic procedures.
The EndoGrab retraction system reduces the number of ports needed for surgery by eliminating the need for traditional hand held retraction. For the surgeon, this simple solution results in the need for less auxiliary personnel, a decreased overall surgery cost, and more control over the surgery. The EndoGrab also offers added benefit to the patient who will experience less post-operative discomfort and scarring.
The EndoGrab is an internally anchored, hands-free retracting device that is introduced at the start of surgery through a 5mm trocar by means of a proprietary Applier tool. The Surgeon uses the Applier to attach the EndoGrab to both the organ requiring retraction and to the internal abdominal wall, thereby removing the organ from the operative field. The Applier is then removed and the port is free for use by other instruments.
3D video animation produced by Virtual Point Multimedia (http://virtual-point.com)

Dieta Alcalina Pdf, Tabla De Alimentos Alcalinos, Beneficios Del Agua Alcalina, Frutas Para Adelgazar--- http://dieta-alcalina-alimentos.good-info.co --- Eligiendo los alimentos para una Dieta Alcalina Es en verdad fácil adoptar una dieta rica en alimentos alcalinos. La mayoría de las frutas y vegetales son excelentes opciones. La carne roja no es una buena opción, pero puedes añadir abundante proteínas a tus comidas usando los productos a base de soya, deliciosos frijoles, legumbres y tanto nueces como almendras. Deberías eliminar las grasas insalubres de tu dieta, pero puedes consumir las grasas buenas como el aceite de oliva, canola y la semilla de lino. El alto contenido graso de los productos lácteos debe ser evitado, pero puedes beber leche de soya y de cabra. Los quesos hechos de leche de soya y cabra también serían buenas opciones. Remplaza las calorías vacías de la soda con delicioso té frío de hierbas, té verde y agua con limón. El café debe ser evitado, pero puedes tomar bebidas calientes a base de té o té verde. Remplaza la pasta con cereales integrales como arroz integral (salvaje), mijo y quinoa. Cuando endulces tus comidas, usa productos naturales como stevia y miel. Como puedes ver, tendrás muchas opciones nutritivas, todas deliciosas y altas en propiedades alcalinizantes. Descubre como la dieta alcalina funciona & por qué los alimentos alcalinos son altamente recomendados para tu salud. Haz clic aquí http://dieta-alcalina-alimentos.good-info.co
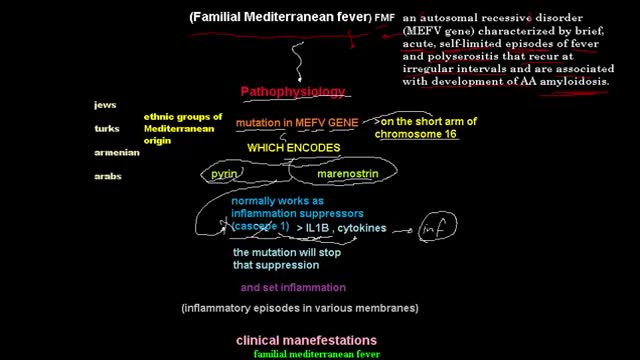
Familial Mediterranean fever is an inflammatory disorder that causes recurrent fevers and painful inflammation of your abdomen, lungs and joints. Familial Mediterranean fever is an inherited disorder that usually occurs in people of Mediterranean origin — including Sephardic Jews, Arabs, Greeks, Italians, Armenians and Turks. But it may affect any ethnic group. Familial Mediterranean fever is typically diagnosed during childhood. While there's no cure for this disorder, you may be able to relieve signs and symptoms of familial Mediterranean fever — or even prevent them altogether — by sticking to your treatment plan.

Testing for the four features of Gerstmann Syndrome in this patient with two separate left sided strokes (left frontoparietal ischaemic stroke followed by left posterior parietal haemorrhagic stroke). He exhibits (i) acalculia, (ii) agraphia, (iii) left-right disorientation, and (iv) finger agnosia. Complicating the issue is his obvious nonfluent aphasia (expressive dysphasia) with paraphasic errors (replacing words with associated words (e.g. says 'fork' instead of 'spoon')) and some comprehension issues.

MRCPCH Clinical Revision - more videos at http://mrcpch.paediatrics.co.uk
Revise for your MRCPCH Clinical exam, with videos and high quality content created by the London Paediatrics Trainees Committee.
Video Credits: Dr Caroline Fertleman, Dr Hermione Race, Dr Camilla Sen, Dr Chloe Macaulay, Dr Emma McLaren, Chris Knapp

Suck reflex. ... Babies also have a hand-to-mouth reflex that goes with rooting and sucking and may suck on fingers or hands. Moro reflex. The Moro reflex is often called a startle reflex because it usually occurs when a baby is startled by a loud sound or movement.

The spleen is one of the most frequently injured intraperitoneal organs, and management of splenic injuries may require splenectomy .. The spleen is an wedge-shaped organ that lies in relation to the ninth and 11th ribs, located in the left hypochondrium and partly in the epigastrium; thus, it is situated between the fundus of the stomach and the diaphragm. The spleen is highly vascular and reddish purple; its size and weight are variable. A normal spleen is not palpable. The spleen's key function is the removal of old red blood cells "RBCs", defective circulating cells, and circulating bacteria. In addition, the spleen helps maintain normal erythrocyte morphology by processing immature erythrocytes, removing their nuclei, and changing the shape of the cellular membrane. Other functions of the spleen include the removal of nuclear remnants of RBCs, denatured hemoglobin, and iron granules ..