Top videos
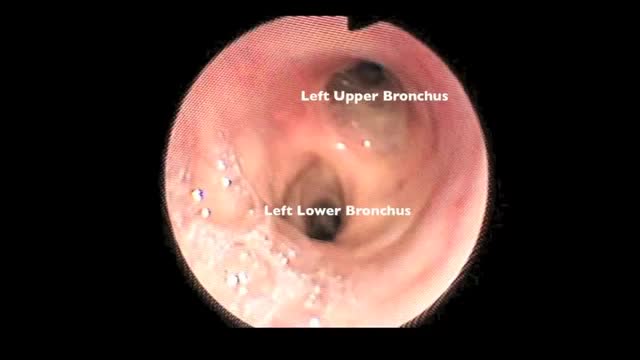
Flexible bronchoscopy is a procedure that allows a clinician to examine the breathing passages (airways) of the lungs (figure 1). Flexible bronchoscopy can be either a diagnostic procedure (to find out more about a possible problem) or a therapeutic procedure (to try to treat an existing problem or condition).
Aspirin is a salicylate (sa-LIS-il-ate). It works by reducing substances in the body that cause pain, fever, and inflammation. Aspirin is used to treat pain, and reduce fever or inflammation. It is sometimes used to treat or prevent heart attacks, strokes, and chest pain (angina).
How To Get Pregnant, Ways To Get Pregnant, Best Days To Get Pregnant, Easiest Way To Get Pregnant.
http://how-to-get-pregnant.info-pro.co
Signs Of Infertility
What Exactly Is Infertility?
The problems with either conceiving a child, or with carrying out the pregnancy to its eventual fruitful end, fall under the definition of infertility. Infertility is the incapability of an individual to become pregnant, in case of females, or the incapability to induce pregnancy, in case of the males.
The inability of an individual to carry out a pregnancy to its full term is also dubbed infertility. How does one recognize infertility? What are the signs of infertility?
Signs of infertility in women:
Children At Age 43 After Years Of "Trying".
You Can Too! Here's How...": http://how-to-get-pregnant.info-pro.co
For More Information
http://how-to-get-pregnant.info-pro.co
http://natural-fertility-remedies.blogspot.com/
Subscribe To Our Channel
https://www.youtube.com/watch?v=R6gRskH4WxY
How To Get Pregnant, Ways To Get Pregnant, Best Days To Get Pregnant, Easiest Way To Get Pregnant, preparing for pregnancy, pills to get pregnant, tricks for getting pregnant, help with pregnancy, help me get pregnant faster, how you get pregnant fast, i really want to get pregnant, male infertility treatments, get me pregnant, natural tips to get pregnant, tips on getting pregnant, how to help get pregnant faster
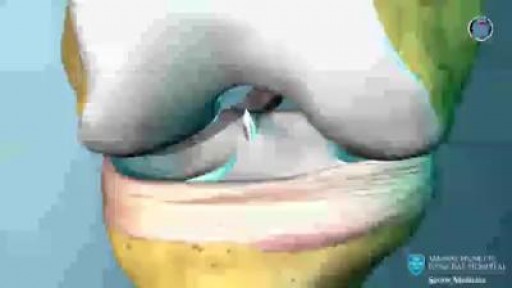
In nonsurgical treatment, progressive physical therapy and rehabilitation can restore the knee to a condition close to its pre-injury state and educate the patient on how to prevent instability.37, 38 This may be supplemented with the use of a hinged knee brace. However, many people who choose not to have surgery may experience secondary injury to the knee due to repetitive instability episodes. Surgical treatment is usually advised in dealing with combined injuries (ACL tears in combination with other injuries in the knee). However, deciding against surgery is reasonable for select patients. Nonsurgical management of isolated ACL tears is likely to be successful or may be indicated in patients:
![So You Want to Be a CARDIOTHORACIC SURGEON [Ep. 13]](https://i.ytimg.com/vi/sdxz242qDFA/maxresdefault.jpg)
So you want to be a cardiothoracic surgeon. You like the idea of open heart surgery and the glory that comes with being a CT surgeon. Let’s debunk the public perception myths of what it means to be a cardiothoracic surgeon, and give it to you straight. This is the reality of cardiothoracic surgery.
✒️ Accompanying Blog Post: https://medschoolinsiders.com/....medical-student/so-y
💌 Sign up for my weekly newsletter - https://medschoolinsiders.com/newsletter
🌍 Website & blog - https://medschoolinsiders.com
📸 Instagram - https://instagram.com/medschoolinsiders
🐦 Twitter - https://twitter.com/medinsiders
🗣️ Facebook - https://facebook.com/medschoolinsiders
🎥 My Youtube Gear: https://kit.co/kevinjubbalmd/
👀 Hand Picked Productivity Tools: https://www.amazon.com/shop/medschoolinsiders
🎵My Study Playlist: https://open.spotify.com/user/....1231934998/playlist/
TIME STAMPS:
00:41 - What is Cardiothoracic Surgery?
04:08 - How to Become a Cardiothoracic Surgeon
06:29 - Subspecialties within Cardiothoracic Surgery
07:49 - What You’ll Love About Cardiothoracic Surgery
09:10 - What You Won’t Love About Cardiothoracic Surgery
10:04 - Should You Become a Cardiothoracic Surgeon?
LINKS FROM VIDEO:
So You Want to Be Playlist: https://www.youtube.com/playli....st?list=PL2ADAFpTg5a
Day in the Life Playlist: https://www.youtube.com/playli....st?list=PLTCN43UFAlB
#medicalschool #cardiothoracicsurgery #soyouwanttobe
====================
Disclaimer: Content of this video is my opinion and does not constitute medical advice. The content and associated links provide general information for general educational purposes only. Use of this information is strictly at your own risk. Kevin Jubbal, M.D. and Med School Insiders LLC will not assume any liability for direct or indirect losses or damages that may result from the use of information contained in this video including but not limited to economic loss, injury, illness or death. May include affiliate links to Amazon. As an Amazon Associate, I may earn a commission on qualifying purchases made through them (at no extra cost to you).
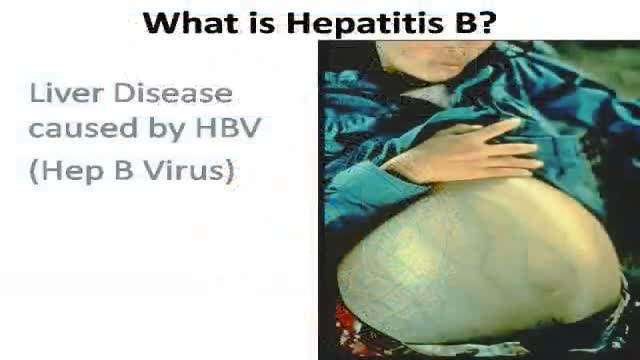
Key facts
Hepatitis B is a viral infection that attacks the liver and can cause both acute and chronic disease.
The virus is transmitted through contact with the blood or other body fluids of an infected person - not through casual contact.
About 2 billion people worldwide have been infected with the virus and about 350 million live with chronic infection. An estimated 600 000 persons die each year due to the acute or chronic consequences of hepatitis B.
About 25% of adults who become chronically infected during childhood later die from liver cancer or cirrhosis (scarring of the liver) caused by the chronic infection.
The hepatitis B virus is 50 to 100 times more infectious than HIV.
Hepatitis B virus is an important occupational hazard for health workers.
Hepatitis B is preventable with a safe and effective vaccine.
-----------------------------------
Hepatitis B is a potentially life-threatening liver infection caused by the hepatitis B virus. It is a major global health problem and the most serious type of viral hepatitis. It can cause chronic liver disease and puts people at high risk of death from cirrhosis of the liver and liver cancer.
Worldwide, an estimated two billion people have been infected with the hepatitis B virus (HBV), and more than 350 million have chronic (long-term) liver infections.
A vaccine against hepatitis B has been available since 1982. Hepatitis B vaccine is 95% effective in preventing HBV infection and its chronic consequences, and is the first vaccine against a major human cancer.

Varicose veins are generally benign. The cause of this condition is not known. For many people, there are no symptoms and varicose veins are simply a cosmetic concern. In some cases, they cause aching pain and discomfort or signal an underlying circulatory problem. Treatment involves compression stockings, exercise, or procedures to close or remove the veins.

Cervical cancer occurs when abnormal cells on the cervix camera.gif grow out of control. The cervix is the lower part of the uterus that opens into the vagina. Cervical cancer can often be successfully treated when it's found early. It is usually found at a very early stage through a Pap test.

This is an example of a surgery to fix a femur (thigh bone) fracture utilizing an intramedullary nail. This is a minimally invasive way of fixing this surgical problem and allows for immediate range of motion and full weight-bearing.