Top videos
Aortic valve replacement is a procedure in which a patient's failing aortic valve is replaced with an artificial heart valve. The aortic valve can be affected by a range of diseases; the valve can either become leaky (aortic insufficiency / regurgitation) or partially blocked (aortic stenosis).

Virtual Ports, Ltd. (http://www.virtual-ports.com) is a medical device company developing and marketing instruments to improve minimally invasive laparoscopic procedures.
The EndoGrab retraction system reduces the number of ports needed for surgery by eliminating the need for traditional hand held retraction. For the surgeon, this simple solution results in the need for less auxiliary personnel, a decreased overall surgery cost, and more control over the surgery. The EndoGrab also offers added benefit to the patient who will experience less post-operative discomfort and scarring.
The EndoGrab is an internally anchored, hands-free retracting device that is introduced at the start of surgery through a 5mm trocar by means of a proprietary Applier tool. The Surgeon uses the Applier to attach the EndoGrab to both the organ requiring retraction and to the internal abdominal wall, thereby removing the organ from the operative field. The Applier is then removed and the port is free for use by other instruments.
3D video animation produced by Virtual Point Multimedia (http://virtual-point.com)

Testing for the four features of Gerstmann Syndrome in this patient with two separate left sided strokes (left frontoparietal ischaemic stroke followed by left posterior parietal haemorrhagic stroke). He exhibits (i) acalculia, (ii) agraphia, (iii) left-right disorientation, and (iv) finger agnosia. Complicating the issue is his obvious nonfluent aphasia (expressive dysphasia) with paraphasic errors (replacing words with associated words (e.g. says 'fork' instead of 'spoon')) and some comprehension issues.
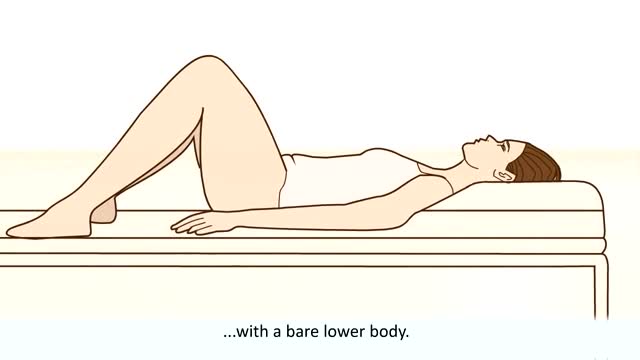
Women are routinely invited to have cervical screening tests (also called smear tests). The tests are done to prevent cervical cancer, not to diagnose cancer. During each test some cells are removed from the neck of the womb (cervix), with a plastic brush. The cells are examined under a microscope to look for early changes that, if ignored and not treated, could develop into cancer of the cervix. You are very unlikely to develop cervical cancer if you have regular cervical screening tests at the times advised by your doctor. If the test shows any abnormality, you will have treatment to stop you ever getting cancer of the cervix. So, an abnormal test does not mean you have cancer. It means you should have some treatment to stop you getting cancer.

The spleen is one of the most frequently injured intraperitoneal organs, and management of splenic injuries may require splenectomy .. The spleen is an wedge-shaped organ that lies in relation to the ninth and 11th ribs, located in the left hypochondrium and partly in the epigastrium; thus, it is situated between the fundus of the stomach and the diaphragm. The spleen is highly vascular and reddish purple; its size and weight are variable. A normal spleen is not palpable. The spleen's key function is the removal of old red blood cells "RBCs", defective circulating cells, and circulating bacteria. In addition, the spleen helps maintain normal erythrocyte morphology by processing immature erythrocytes, removing their nuclei, and changing the shape of the cellular membrane. Other functions of the spleen include the removal of nuclear remnants of RBCs, denatured hemoglobin, and iron granules ..
Que Es Bueno Para La Diabetes Medicina Natural. Porque Con Este Método Que Voy a Revelarte que es 10 Veces Más Efectivo Que Cualquier Otro Podrás Vencer A Tu Diabetes RÁPIDAMENTE. Si no hubiera sido por el poderoso método inusual pero PROBADO que usé para obtener RESULTADOS rápidos y controlar la diabetes. La genialidad de este gran descubrimiento es que está diseñado para controlar, frenar y vencer a la diabetes. con la “complicidad” de tu propio cuerpo que se auto regenera si se le instalan los comando correctos en el metabolismo. Sin importar si tienes 7 ó 90 años. Sin importar si tu nivel de azúcar es más incontrolable que un caballo salvaje, o tu tipo de diabetes. Sin importar cuantas veces tu doctor te ha dicho que la diabetes no tiene cura. Sin importar si has fallado una docena de veces con tratamientos, medicamentos o métodos convencionales que NO SIRVEN. Estás a punto de descubrir cómo controlar la diabetes usando la Solución Natural más exitosa jamás revelada que transformará tu cuerpo en una máquina generadora de salud y energía – ¡en tan solo unos pocos días! haciendo click aqui. http://vencer-la-diabetes-rapido.info-pro.co

Traumatic penile injury can be due to multiple factors. Penile fracture, penile amputation, penetrating penile injuries, and penile soft tissue injuries are considered urologic emergencies and typically require surgical intervention. The goals of treatment for penile trauma are universal: preservation of penile length, erectile function, and maintenance of the ability to void while standing. Traumatic injury to the penis may concomitantly involve the urethra.[1, 2] Urethral injury and repair is beyond the scope of this article but details can be found in Urethral Trauma. Penile fracture Penile fracture is the traumatic rupture of the corpus cavernosum. Traumatic rupture of the penis is relatively uncommon and is considered a urologic emergency.[3] Sudden blunt trauma or abrupt lateral bending of the penis in an erect state can break the markedly thinned and stiff tunica albuginea, resulting in a fractured penis. One or both corpora may be involved, and concomitant injury to the penile urethra may occur. Urethral trauma is more common when both corpora cavernosa are injured.[4] Penile rupture can usually be diagnosed based solely on history and physical examination findings; however, in equivocal cases, diagnostic cavernosography or MRI should be performed. Concomitant urethral injury must be considered; therefore, preoperative retrograde urethrographic studies should generally be performed. See the images below.
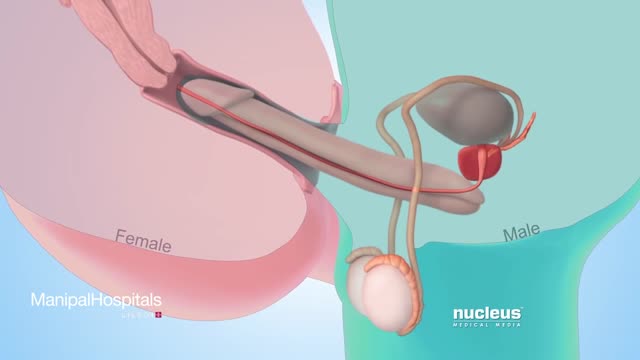
Testicular sperm aspiration (TESA) is a procedure performed for men who are having sperm retrieved for in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). It is done with local anesthesia in the operating room or office and is coordinated with their female partner's egg retrieval.
![So You Want to Be a CARDIOTHORACIC SURGEON [Ep. 13]](https://i.ytimg.com/vi/sdxz242qDFA/maxresdefault.jpg)
So you want to be a cardiothoracic surgeon. You like the idea of open heart surgery and the glory that comes with being a CT surgeon. Let’s debunk the public perception myths of what it means to be a cardiothoracic surgeon, and give it to you straight. This is the reality of cardiothoracic surgery.
✒️ Accompanying Blog Post: https://medschoolinsiders.com/....medical-student/so-y
💌 Sign up for my weekly newsletter - https://medschoolinsiders.com/newsletter
🌍 Website & blog - https://medschoolinsiders.com
📸 Instagram - https://instagram.com/medschoolinsiders
🐦 Twitter - https://twitter.com/medinsiders
🗣️ Facebook - https://facebook.com/medschoolinsiders
🎥 My Youtube Gear: https://kit.co/kevinjubbalmd/
👀 Hand Picked Productivity Tools: https://www.amazon.com/shop/medschoolinsiders
🎵My Study Playlist: https://open.spotify.com/user/....1231934998/playlist/
TIME STAMPS:
00:41 - What is Cardiothoracic Surgery?
04:08 - How to Become a Cardiothoracic Surgeon
06:29 - Subspecialties within Cardiothoracic Surgery
07:49 - What You’ll Love About Cardiothoracic Surgery
09:10 - What You Won’t Love About Cardiothoracic Surgery
10:04 - Should You Become a Cardiothoracic Surgeon?
LINKS FROM VIDEO:
So You Want to Be Playlist: https://www.youtube.com/playli....st?list=PL2ADAFpTg5a
Day in the Life Playlist: https://www.youtube.com/playli....st?list=PLTCN43UFAlB
#medicalschool #cardiothoracicsurgery #soyouwanttobe
====================
Disclaimer: Content of this video is my opinion and does not constitute medical advice. The content and associated links provide general information for general educational purposes only. Use of this information is strictly at your own risk. Kevin Jubbal, M.D. and Med School Insiders LLC will not assume any liability for direct or indirect losses or damages that may result from the use of information contained in this video including but not limited to economic loss, injury, illness or death. May include affiliate links to Amazon. As an Amazon Associate, I may earn a commission on qualifying purchases made through them (at no extra cost to you).
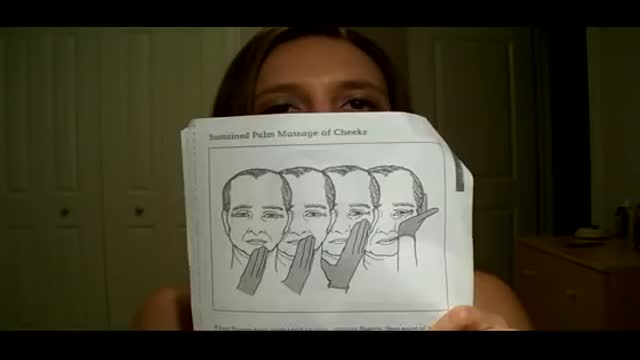
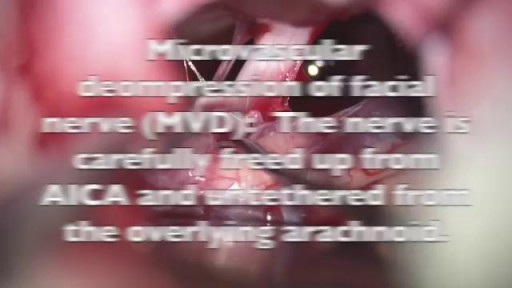
Bell's palsy is a form of facial paralysis resulting from damage or trauma to the facial nerves. The facial nerve-also called the 7th cranial nerve-travels through a narrow, bony canal (called the Fallopian canal) in the skull, beneath the ear, to the muscles on each side of the face. For most of its journey, the nerve is encased in this bony shell. Each facial nerve directs the muscles on one side of the face, including those that control eye blinking and closing, and facial expressions such as smiling and frowning. Additionally, the facial nerve carries nerve impulses to the lacrimal or tear glands, the saliva glands, and the muscles of a small bone in the middle of the ear called the stapes. The facial nerve also transmits taste sensations from the tongue. When Bell's palsy occurs, the function of the facial nerve is disrupted, causing an interruption in the messages the brain sends to the facial muscles. This interruption results in facial weakness or paralysis. Bell's palsy is named for Sir Charles Bell, a 19th century Scottish surgeon who described the facial nerve and its connection to the condition. The disorder, which is not related to stroke, is the most common cause of facial paralysis. Generally, Bell's palsy affects only one of the paired facial nerves and one side of the face, however, in rare cases, it can affect both sides.

Overweight does not necessarily equal unhealthy. There are actually plenty of overweight people who are in excellent health (1). Conversely, many normal weight people have the metabolic problems associated with obesity (2). That’s because the fat under the skin is actually not that big of a problem (at least not from a health standpoint, it’s more of a cosmetic problem). It’s the fat in the abdominal cavity, the belly fat, that causes the biggest issues (3). If you have a lot of excess fat around your waistline, even if you’re not very heavy, then you should take some steps to get rid of it. Belly fat is usually estimated by measuring the circumference around your waist. This can easily be done at home with a simple tape measure. Anything above 40 inches (102 cm) in men and 35 inches (88 cm) in women, is known as abdominal obesity. There are actually a few proven strategies that have been shown to target the fat in the belly area more than other areas of the body.