Top videos

A paralyzed teenager will make the first kick at the 2014 World Cup before the opening match between Brazil v. Croatia. The exoskeleton, which is enabling the paralyzed teen to walk and kick a soccer ball, has been designed by Duke University supported by the Walk Again Project. This monumental step in technology will make for a very exciting first kick, and let's not forget that this teenager will be walking when prior knowledge told us that was impossible. What are your thoughts on the opening kick?

This is a breast life surgery. Over the years, factors such as pregnancy, nursing and the force of gravity take their toll on a woman's breasts. As the skin loses its elasticity, the breasts often lose their shape and firmness and begin to sag. Breast lift is a surgical procedure to raise and reshape the breasts (at least for a time). If your breasts are small or have lost volume (for example from pregnancy) breast implants inserted in conjunction with mastopexy can increase both their firmness and their size.

This is an example of a surgery to fix a femur (thigh bone) fracture utilizing an intramedullary nail. This is a minimally invasive way of fixing this surgical problem and allows for immediate range of motion and full weight-bearing.

Formerly called toxemia, preeclampsia is a condition that pregnant women develop. It is marked by high blood pressure in women who have previously not experienced high blood pressure before. Preeclamptic women will have a high level of protein in their urine and often also have swelling in the feet, legs, and hands. This condition usually appears late in pregnancy, generally after the 20 week mark, although it can occur earlier

Pharyngitis is caused by swelling in the back of the throat (pharynx) between the tonsils and the voice box (larynx). Most sore throats are caused by colds, the flu, coxsackie virus or mono (mononucleosis). Bacteria that can cause pharyngitis in some cases: Strep throat is caused by group A streptococcus.

Sialadenitis is an infection of the salivary glands. It is usually caused by a virus or bacteria . The parotid (in front of the ear) and submandibular (under the chin) glands are most commonly affected. Sialadenitis may be associated with pain, tenderness, redness, and gradual, localized swelling of the affected area.
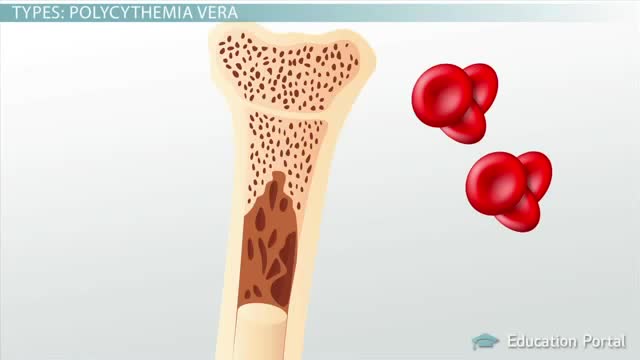
Polycythemia vera (pol-e-sigh-THEE-me-uh VEER-uh) is a slow-growing type of blood cancer in which your bone marrow makes too many red blood cells. Polycythemia vera may also result in production of too many of the other types of blood cells — white blood cells and platelets. These excess cells thicken your blood and cause complications, such as such as a risk of blood clots or bleeding. Polycythemia vera isn't common. It usually develops slowly, and you may have it for years without noticing signs or symptoms. Often, polycythemia vera is found during a blood test done for some other reason. Without treatment, polycythemia vera can be life-threatening. However, with proper medical care, many people experience few problems related to this disease. Over time, there's a risk of progressing to more-serious blood cancers, such as myelofibrosis or acute leukemia.
Bronchiectasis is an abnormal dilation of the proximal and medium-sized bronchi (>2 mm in diameter) caused by weakening or destruction of the muscular and elastic components of the bronchial walls. Affected areas may show a variety of changes, including transmural inflammation, edema, scarring, and ulceration, among other findings. Distal lung parenchyma may also be damaged secondary to persistent microbial infection and frequent postobstructive pneumonia. Bronchiectasis can be congenital but is most often acquired.[9] Congenital bronchiectasis usually affects infants and children. These cases result from developmental arrest of the bronchial tree. Acquired forms occur in adults and older children and require an infectious insult, impairment of drainage, airway obstruction, and/or a defect in host defense. The tissue is also damaged in part by the host response of neutrophilic proteases, inflammatory cytokines, nitric oxide, and oxygen radicals. This results in damage to the muscular and elastic components of the bronchial wall. Additionally, peribronchial alveolar tissue may be damaged, resulting in diffuse peribronchial fibrosis.[12] The result is abnormal bronchial dilatation with bronchial wall destruction and transmural inflammation. The most important functional finding of altered airway anatomy is severely impaired clearance of secretions from the bronchial tree. Impaired clearance of secretions causes colonization and infection with pathogenic organisms, contributing to the purulent expectoration commonly observed in patients with bronchiectasis. The result is further bronchial damage and a vicious cycle of bronchial damage, bronchial dilation, impaired clearance of secretions, recurrent infection, and more bronchial damage
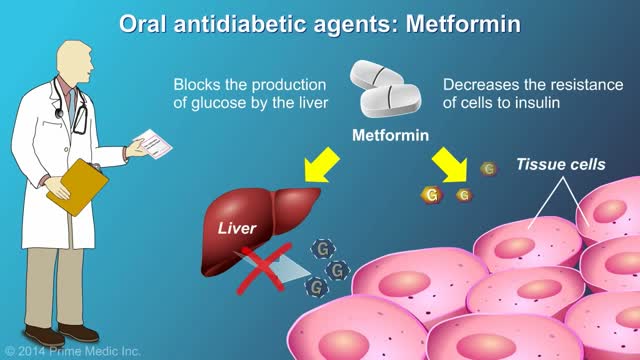
protecting the body from damage caused by hyperglycemia cannot be overstated. In the United States, 57.9% of diabetic patients have one or more diabetes complications, and 14.3% have three or more.1 Strict glycemic control is the primary method of reducing the development and progression of microvascular complications, such as retinopathy, nephropathy, and neuropathy. Aggressive treatment of dyslipidemia and hypertension decreases macrovascular complications.2-4 Glycemic Control There are two primary techniques available for physicians to assess the quality of a patient’s glycemic control: self-monitoring of blood glucose (SMBG) and interval measurement of hemoglobin A1c (HbA1c).

Dieta Alcalina Pdf, Tabla De Alimentos Alcalinos, Beneficios Del Agua Alcalina, Frutas Para Adelgazar--- http://dieta-alcalina-alimentos.good-info.co --- Eligiendo los alimentos para una Dieta Alcalina Es en verdad fácil adoptar una dieta rica en alimentos alcalinos. La mayoría de las frutas y vegetales son excelentes opciones. La carne roja no es una buena opción, pero puedes añadir abundante proteínas a tus comidas usando los productos a base de soya, deliciosos frijoles, legumbres y tanto nueces como almendras. Deberías eliminar las grasas insalubres de tu dieta, pero puedes consumir las grasas buenas como el aceite de oliva, canola y la semilla de lino. El alto contenido graso de los productos lácteos debe ser evitado, pero puedes beber leche de soya y de cabra. Los quesos hechos de leche de soya y cabra también serían buenas opciones. Remplaza las calorías vacías de la soda con delicioso té frío de hierbas, té verde y agua con limón. El café debe ser evitado, pero puedes tomar bebidas calientes a base de té o té verde. Remplaza la pasta con cereales integrales como arroz integral (salvaje), mijo y quinoa. Cuando endulces tus comidas, usa productos naturales como stevia y miel. Como puedes ver, tendrás muchas opciones nutritivas, todas deliciosas y altas en propiedades alcalinizantes. Descubre como la dieta alcalina funciona & por qué los alimentos alcalinos son altamente recomendados para tu salud. Haz clic aquí http://dieta-alcalina-alimentos.good-info.co
When your arteries cannot supply enough blood to your heart, your doctor may recommend coronary artery bypass graft (CABG) surgery. One of the most common heart surgeries in the United States, CABG surgery restores blood flow to your heart. Approximately every 10 minutes, someone has beating heart or "off-pump" bypass surgery1. Beating heart bypass surgery is — in simple terms — bypass surgery that is performed on your heart while it is beating. Your heart will not be stopped during surgery. You will not need a heart-lung machine. Your heart and lungs will continue to perform during your surgery. Surgeons use a tissue stabilization system to immobilize the area of the heart where they need to work. Beating heart bypass surgery is also called Off Pump Coronary Artery Bypass Surgery (OPCAB). Both OPCAB and conventional on-pump surgery restore blood flow to the heart. However, off-pump bypass surgery has proven to reduce side effects in certain types of patients.

Human immunodeficiency virus infection / acquired immunodeficiency syndrome (HIV/AIDS) is a disease of the human immune system caused by the human immunodeficiency virus (HIV).[1] During the initial infection a person may experience a brief period of influenza-like illness. This is typically followed by a prolonged period without symptoms. As the illness progresses it interferes more and more with the immune system, making people much more likely to get infections, including opportunistic infections, and tumors that do not usually affect people with working immune systems.
HIV is transmitted primarily via unprotected sexual intercourse (including anal and even oral sex), contaminated blood transfusions and hypodermic needles, and from mother to child during pregnancy, delivery, or breastfeeding.[2] Some bodily fluids, such as saliva and tears, do not transmit HIV.[3] Prevention of HIV infection, primarily through safe sex and needle-exchange programs, is a key strategy to control the spread of the disease. There is no cure or vaccine; however, antiretroviral treatment can slow the course of the disease and may lead to a near-normal life expectancy. While antiretroviral treatment reduces the risk of death and complications from the disease, these medications are expensive and may be associated with side effects.
Genetic research indicates that HIV originated in West-central Africa during the early twentieth century.[4] AIDS was first recognized by the Centers for Disease Control and Prevention (CDC) in 1981 and its cause—HIV infection—was identified in the early part of the decade.[5] Since its discovery, AIDS has caused nearly 30 million deaths (as of 2009).[6] As of 2010, approximately 34 million people have contracted HIV globally.[7] AIDS is considered a pandemic—a disease outbreak which is present over a large area and is actively spreading.[8]
HIV/AIDS has had a great impact on society, both as an illness and as a source of discrimination. The disease also has significant economic impacts. There are many misconceptions about HIV/AIDS such as the belief that it can be transmitted by casual non-sexual contact. The disease has also become subject to many controversies involving religion.