Top videos

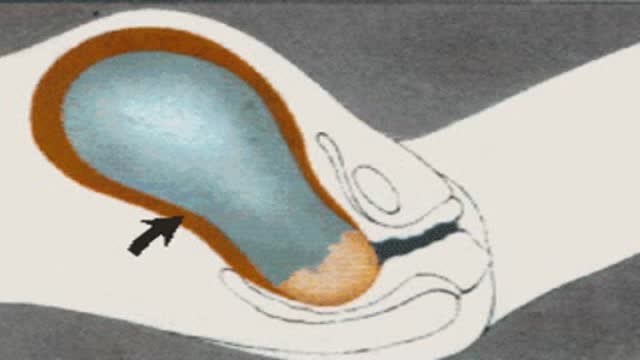
Podalic version is an obstetric procedure wherein the fetus is turned within the womb such that one or both feet present through the cervix during childbirth. It is used most often in cases where the fetus lies transversely or in another abnormal position in the womb.
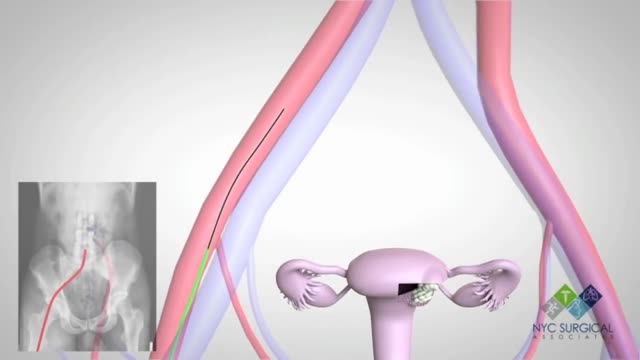
There's no single best approach to uterine fibroid treatment — many treatment options exist. If you have symptoms, talk with your doctor about options for symptom relief. Watchful waiting Many women with uterine fibroids experience no signs or symptoms, or only mildly annoying signs and symptoms that they can live with. If that's the case for you, watchful waiting could be the best option. Fibroids aren't cancerous. They rarely interfere with pregnancy. They usually grow slowly — or not at all — and tend to shrink after menopause, when levels of reproductive hormones drop. Medications Medications for uterine fibroids target hormones that regulate your menstrual cycle, treating symptoms such as heavy menstrual bleeding and pelvic pressure. They don't eliminate fibroids, but may shrink them. Medications include: Gonadotropin-releasing hormone (Gn-RH) agonists. Medications called Gn-RH agonists (Lupron, Synarel, others) treat fibroids by blocking the production of estrogen and progesterone, putting you into a temporary postmenopausal state. As a result, menstruation stops, fibroids shrink and anemia often improves. Your doctor may prescribe a Gn-RH agonist to shrink the size of your fibroids before a planned surgery. Many women have significant hot flashes while using Gn-RH agonists. Gn-RH agonists typically are used for no more than three to six months because symptoms return when the medication is stopped and long-term use can cause loss of bone. Progestin-releasing intrauterine device (IUD). A progestin-releasing IUD can relieve heavy bleeding caused by fibroids. A progestin-releasing IUD provides symptom relief only and doesn't shrink fibroids or make them disappear. It also prevents pregnancy. Tranexamic acid (Lysteda). This nonhormonal medication is taken to ease heavy menstrual periods. It's taken only on heavy bleeding days. Other medications. Your doctor might recommend other medications. For example, oral contraceptives or progestins can help control menstrual bleeding, but they don't reduce fibroid size. Nonsteroidal anti-inflammatory drugs (NSAIDs), which are not hormonal medications, may be effective in relieving pain related to fibroids, but they don't reduce bleeding caused by fibroids. Your doctor may also suggest that you take vitamins and iron if you have heavy menstrual bleeding and anemia

A vaginoplasty is a surgical procedure that tightens the vagina. This is done by removing excess vaginal lining and tightening the surrounding soft tissues and muscles. During delivery of a baby the vagina and surrounding tissues and muscles become stretched. After delivery the vagina may return to a more “normal” size, but it often fails to return to its’ pre pregnancy diameter. Generally, the more vaginal deliveries, the worse the condition gets. Many women will complain of decreased sensation and sexual satisfaction during intercourse. Commonly this is due to a lack of friction. Often their partner may notice a change although he may say nothing. Kegel exercises are often recommended but rarely succeed in restoring vaginal tightness.
Childbirth (also called labour, birth, partus or parturition) is the culmination of a human pregnancy or gestation period with birth of one or more newborn infants from a woman’s uterus. The process of normal human childbirth is categorized in three stages of labour: the shortening and dilation of the cervix, descent and birth of the infant, and birth of the placenta. In some cases, childbirth is achieved through caesarean section, the removal of the neonate through a surgical incision in the abdomen, rather than through vaginal birth
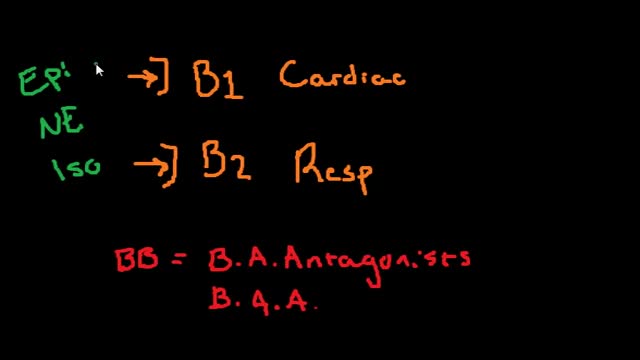
Beta blockers, also known as beta-adrenergic blocking agents, are medications that reduce your blood pressure. Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. When you take beta blockers, your heart beats more slowly and with less force, thereby reducing blood pressure. Beta blockers also help blood vessels open up to improve blood flow. Examples of beta blockers Some beta blockers mainly affect your heart, while others affect both your heart and your blood vessels. Which one is best for you depends on your health and the condition being treated. Examples of oral beta blockers include: Acebutolol (Sectral) Atenolol (Tenormin) Bisoprolol (Zebeta) Metoprolol (Lopressor, Toprol-XL) Nadolol (Corgard) Nebivolol (Bystolic) Propranolol (Inderal LA, InnoPran XL)
At one time, women who had delivered by cesarean section in the past would usually have another cesarean section for any future pregnancies. The rationale was that if allowed to labor, many of these women with a scar in their uterus would rupture the uterus along the weakness of the old scar. Over time, a number of observations have become apparent: Most women with a previous cesarean section can labor and deliver vaginally without rupturing their uterus. Some women who try this will, in fact, rupture their uterus. When the uterus ruptures, the rupture may have consequences ranging from near trivial to disastrous. It can be very difficult to diagnose a uterine rupture prior to observing fetal effects (eg, bradycardia). Once fetal effects are demonstrated, even a very fast reaction and nearly immediate delivery may not lead to a good outcome. The more cesarean sections the patient has, the greater the risk of subsequent rupture during labor. The greatest risk occurs following a “classical” cesarean section (in which the uterine incision extends up into the fundus.) The least risk of rupture is among women who had a low cervical transverse incision. Low vertical incisions probably increase the risk of rupture some, but usually not as much as a classical incision. Many studies have found the use of oxytocin to be associated with an increased risk of rupture, either because of the oxytocin itself, or perhaps because of the clinical circumstances under which it would be contemplated. Pain medication, including epidural anesthetic, has not resulted greater adverse outcome because of the theoretical risk of decreasing the attendant’s ability to detect rupture early. The greatest risk of rupture occurs during labor, but some of the ruptures occur prior to the onset of labor. This is particularly true of the classical incisions. Overall successful vaginal delivery rates following previous cesarean section are in the neighborhood of 70 This means that about 30of women undergoing a vaginal trial of labor will end up requiring a cesarean section. Those who undergo cesarean section (failed VBAC) after a lengthy labor will frequently have a longer recovery and greater risk of infection than had they undergone a scheduled cesarean section without labor. Women whose first cesarean was for failure to progress in labor are only somewhat less likely to be succesful in their quest for a VBAC than those with presumably non-recurring reasons for cesarean section. For these reasons, women with a prior cesarean section are counseled about their options for delivery with a subsequent pregnancy: Repeat Cesarean Section, or Vaginal Trial of Labor. They are usually advised of the approximate 70successful VBAC rate (modified for individual risk factors). They are counseled about the risk of uterine rupture (approximately 1in most series), and that while the majority of those ruptures do not lead to bad outcome, some of them do, including fetal brain damage and death, and maternal loss of future childbearing. They are advised of the usual surgical risks of infection, bleeding, anesthesia complications and surgical injury to adjacent structures. After counseling, many obstetricians leave the decision for a repeat cesarean or VBAC to the patient. Both approaches have risks and benefits, but they are different risks and different benefits. Fortunately, most repeat cesarean sections and most vaginal trials of labor go well, without any serious complications. For those choosing a trial of labor, close monitoring of mother and baby, with early detection of labor abnormalities and preparation for

http://penilepapules.plus101.com/ ----- White Spots On Shaft, Pearly Penile Papules Treatment Cream, Single Red Bump On Shaft, Ppp Surgery. Common Home Made Remedies for Pearly Penile Papules. When it comes to treating pearly penile papules many people find it very difficult to reach one of the medical treatments. This is mainly because they are highly expensive and not many people can afford spending large amounts of money on surgery and recovery. In addition to that, these procedures have been reported as being quite risky, which make the men suffering from pearly penile papules think twice before going for one of the available surgeries. This is why, along the time, many homemade, natural treatments have been experienced, so that a cheaper and less risky way of curing pearly penile papules would be found. Some of the methods which have been tried proved to be very less effective, while some did not have any effect at all. Yet, there have also been methods which not only proved to be effective, but they were also considered to be much better than the medical treatment. Most of those who have tried the tea tree oil treatment reported significant diminish of the number of the papules from their penises. In addition to the clearing of the skin, they have also noticed that there were no side effects and the skin remained soft after the papules were removed. As the method was quite simple to put in practice (it requires the application of tea tree oil on the affected area with a cotton swab for three or four times per day), many men decided this was indeed a great solution to their problem.

Watch this clinical examination video to learn how to diagnose inguinal related groin pain.
This video clip is part of the FIFA Diploma in Football Medicine and the FIFA Medical Network. To enrol or to find our more click on the following link http://www.fifamedicalnetwork.com
The Diploma is a free online course designed to help clinicians learn how to diagnose and manage common football-related injuries and illnesses. There are a total of 42 modules created by football medicine experts. Visit a single page, complete individual modules or finish the entire course.
The network provides the opportunity for clinicians around the world to meet and share ideas relating to football medicine. Ask about an interesting case, debate current practice and discuss treatment strategies. Create a profile and log on to interact with other health professionals from around the globe.
This is not medical advice. The content is intended as educational content for health care professionals and students. If you are a patient, seek care of a health care professional.

Brachytherapy or localized radiation treatment can be used in certain patients with breast cancer. Depending on tumor size and other factor, physicians may use APBI or accelerated partial breast irradiation. Dr. Elizabeth Tapen, a radiation oncologist, reviews brachytherapy for breast cancer.

In this video, we show a sports hernia self treatment we give many of our clients. It is not the only part of treatment. Grabbing the skin around the region of the groin strain can reduce pain and stiffness with turning and twisting. Sports hernias are often misdiagnosed with hip labrum tears, hip impingement, adductor tendonitis and abdominal strains.
Want more information? We have a more detailed free webinar on our page here. https://bit.ly/37thtNF
Want some treatment or suggestions of exercises or stretches? Contact us! We have in-person and virtual sessions.
Costa Mesa CA 715-502-4243 www.p2sportscare.com
Sports Hernia Diagnosis
What Is A Sports Hernia?
A sports hernia is tearing of the transversalis fascia of the lower abdominal or groin region. A common misconception is that a sports hernia is the same as a traditional hernia. The mechanism of injury is rapid twisting and change of direction within sports, such as football, basketball, soccer and hockey.
The term “sports hernia” is becoming mainstream with more professional athletes being diagnosed. The following are just to name a few:
Torii Hunter
Tom Brady
Ryan Getzlaf
Julio Jones
Jeremy Shockey
If you follow any of these professional athletes, they all seem to have the same thing in common: Lingering groin pain. If you play fantasy sports, this is a major headache since it seems so minor, but it can land a player on Injury Reserve on a moments notice. In real life, it is a very frustrating condition to say the least. It is hard to pin point, goes away with rest and comes back after activity, but is hardly painful enough to make you want to stop. It lingers and is always on your mind. And if you’re looking for my step-by-step sports hernia rehab video course here it is.
One the best definitions of Sport hernias is the following by Harmon:
The phenomena of chronic activity–related groin pain that it is unresponsive to conservative therapy and significantly improves with surgical repair.”
This is truly how sports hernias behave in a clinical setting. It is not uncommon for a sports hernia to be unrecognized for months and even years. Unlike your typical sports injury, most sports medicine offices have only seen a handful of cases. It’s just not on most doctors’ radar. The purpose of this article is not only to bring awareness about sports hernias, but also to educate.
Will you find quick fixes in this article for sports hernia rehab?
Nope. There is no quick fix for this condition, and if someone is trying to sell you one, they are blowing smoke up your you-know-what.
Is there a way to decrease the pain related to sports hernias?
Yes. Proper rehab and avoidance of activity for a certain period of time will assist greatly, but this will not always stop it from coming back. Pain is the first thing to go and last thing to come. Do not be fooled when you become pain-free by resting it. Pain is only one measure of improvement in your rehab. Strength, change of direction, balance and power (just to name a few) are important, since you obviously desire to play your sport again. If you wanted to be a couch potato, you would be feeling better in no time. Watching Sports Center doesn’t require any movement.
Why is this article so long?
There is a lot of information on sports hernias available to you on the web. However, much of the information is spread out all over the internet and hard for athletes to digest due to complicated terminology. This article lays out the foundational terminology you will need to understand what options you have with your injury. We will go over anatomy, biomechanics, rehab, surgery, and even the fun facts. The information I am using is from the last ten years of medical research, up until 2016. We will be making updates overtime when something new is found as well. So link to this page and share with friends. This is the best source for information on sports hernias you will find.
Common Names (or Aliases?) for Sports Hernias
Sportsman’s Hernia
Athletic Pubalgia
Gilmore’s Groin
How Do You Know If You Have A Sports Hernia?
Typical athlete characteristics:
Male, age mid-20s
Common sports: soccer, hockey, tennis, football, field hockey
Motions involved: cutting, pivoting, kicking and sharp turns
Gradual onset
How A Sports Hernia Develops
Chronic groin pain typically happens over time, which is why with sports hernias, we do not hear many stories of feeling a “pop” or a specific moment of injury. It is the result of “overuse” mechanics stemming from a combination of inadequate strength and endurance, lack of dynamic control, movement pattern abnormalities, and discoordination of motion in the groin area.
#sportsherniadiagnosisselftreatment #sportshernia #california

Best and 100% Successful Hymen Repair Surgery in Delhi with Latest Ultrafine Hymen repair Technology. 100% successful , Secure and Private. for more information visit: http://www.olmeccosmeticsurgery.com/best-hymenoplasty-surgery-india-delhi/