Top videos
You may have a lot of questions about epilepsy. We will help you understand the basics, answer the most common questions, and help you find resources and other information you may need. However, information alone won’t help you manage your epilepsy and find a way to cope with the effects on your daily life. You’ll need to learn how to use the information and make it work for you.
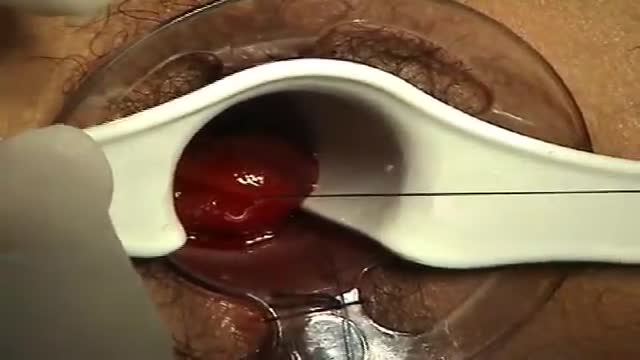
A surgeon begins the PPH stapled hemorrhoidectomy by inserting a circular anal dilator and obturator into the anal canal and then securing the dilator in place with four sutures. The surgeon then inserts a PPH anoscope into the obturator. Next, he places a circumferential purse-string suture of 2-0 Monocryl on a UR-6 needle 4 cm proximal to the dentate line. The surgeon opens a PPH stapler and places its anvil across the purse string. The stapler is then closed and fired; it is held closed for two minutes to improve hemostasis. Prior to firing the stapler in a female patient, the surgeon places a gloved finger in the vagina to ensure the vaginal mucosa and rectal-vaginal septum are not trapped within the jaws of the closed stapler. The surgeon then opens and removes the stapler.
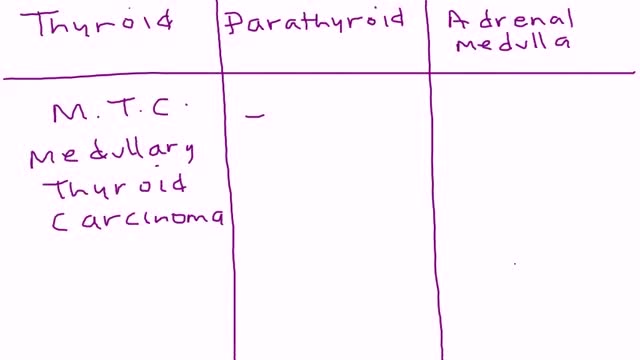
Multiple endocrine neoplasia type 2 (MEN2) (also known as "Pheochromocytoma and amyloid producing medullary thyroid carcinoma", "PTC syndrome," and "Sipple syndrome") is a group of medical disorders associated with tumors of the endocrine system. The tumors may be benign or malignant (cancer).
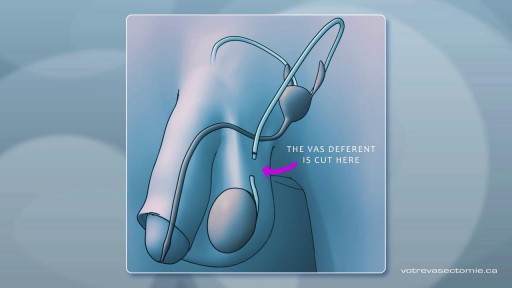
A vasectomy is one of the most effective kinds of birth control out there, and THE most effective method for people with penises and testicles. Vasectomies are almost 100% effective at preventing pregnancy — but not right away. It takes about 3 months for your semen to become sperm-free
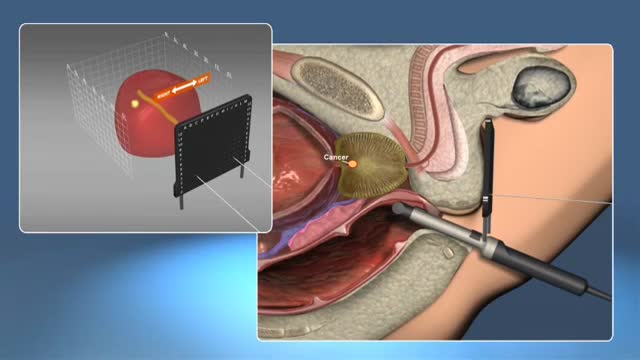
A prostate gland biopsy is a test to remove small samples of prostate tissue to be looked at under a microscope. ... For a prostate biopsy, a thin needle is inserted through the rectum (transrectal biopsy), through the urethra, or through the area between the anus and scrotum (perineum).
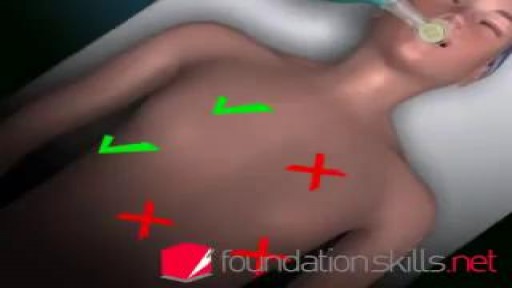
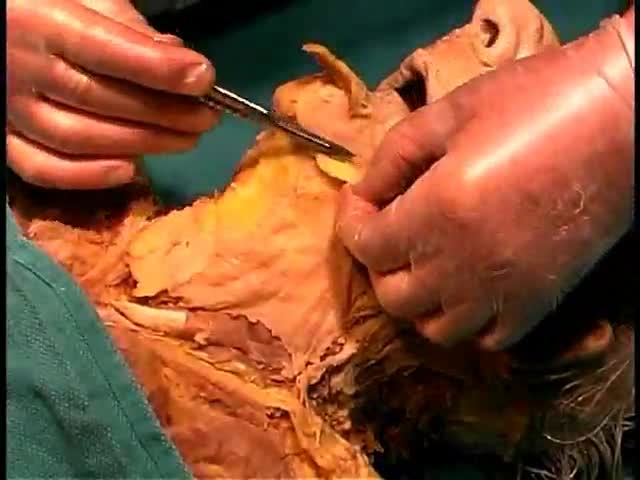
Endotracheal intubation is a medical procedure in which a tube is placed into the windpipe (trachea) through the mouth or nose. In most emergency situations it is placed through the mouth. Whether you are awake (conscious) or not awake (unconscious), you will be given medicine to make it easier to insert the tube. After endotracheal intubation, you will likely be placed on a breathing machine. If you are awake after the procedure, your health care provider may give you medicine to reduce your anxiety or discomfort.
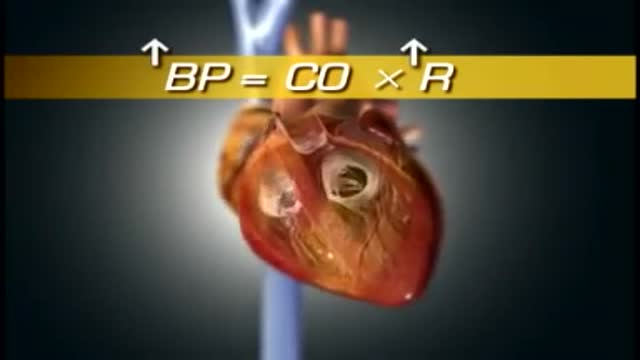
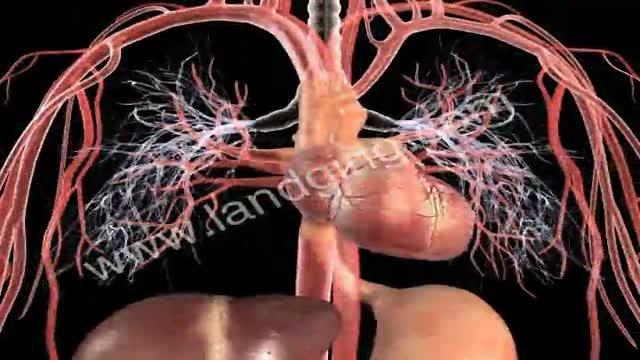
High blood pressure is a common condition in which the long-term force of the blood against your artery walls is high enough that it may eventually cause health problems, such as heart disease. Blood pressure is determined both by the amount of blood your heart pumps and the amount of resistance to blood flow in your arteries. The more blood your heart pumps and the narrower your arteries, the higher your blood pressure. You can have high blood pressure (hypertension) for years without any symptoms. Even without symptoms, damage to blood vessels and your heart continues and can be detected. Uncontrolled high blood pressure increases your risk of serious health problems, including heart attack and stroke. High blood pressure generally develops over many years, and it affects nearly everyone eventually. Fortunately, high blood pressure can be easily detected. And once you know you have high blood pressure, you can work with your doctor to control it.
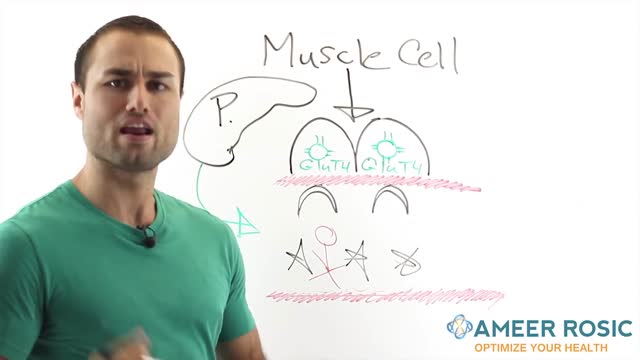
Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy or to store glucose for future use. Insulin helps keeps your blood sugar level from getting too high (hyperglycemia) or too low (hypoglycemia). The cells in your body need sugar for energy. However, sugar cannot go into most of your cells directly. After you eat food and your blood sugar level rises, cells in your pancreas (known as beta cells) are signaled to release insulin into your bloodstream. Insulin then attaches to and signals cells to absorb sugar from the bloodstream. Insulin is often described as a “key,” which unlocks the cell to allow sugar to enter the cell and be used for energy.