Top videos

Identify the anatomy and explain the physiology of the breast on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the breast, including the clock and quadrant methods, and targeted examinations based on mammographic findings.
Describe the various diagnostic pathways that may lead to a sonographic breast examination, and explain how the ultrasound findings are correlated with other imaging modalities.
Identify and describe sonographic images of benign and malignant features and common breast pathologies.
Explain biopsy techniques for breast tumors.
Define and use related medical terminology.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference

Identify the anatomy and explain the physiology of the scrotum on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the scrotum.
Identify and describe sonographic images of congenital abnormalities of the scrotum.
Identify and describe sonographic images of pathologies of the scrotum.
Identify and describe sonographic images of extratesticular disease processes.
Identify the anatomy and explain the physiology of the prostate on diagrams and sonograms.
Describe and demonstrate the protocol for transabdominal and endorectal sonographic scanning of the prostate.
Identify and describe sonographic images of benign and malignant pathologies of the prostate, including benign hyperplasia, prostatitis, carcinoma, and calculi.
Explain the technique for prostate biopsy.
Define the criteria for an ultrasound appearance of prostate tumor staging.
Explain the technique for radiation seed implantation.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).

Subscribe and 🔔 to the BBC 👉 https://bit.ly/BBCYouTubeSub
Watch the BBC first on iPlayer 👉 https://bbc.in/iPlayer-Home http://www.bbc.co.uk/human Richard Edwards undergoes a double hand transplant in which his hands are amputated and replaced with hands from a donor. This is the first time this has been done. Three months later the new hands are already changing his life.
#bbc
All our TV channels and S4C are available to watch live through BBC iPlayer, although some programmes may not be available to stream online due to rights. If you would like to read more on what types of programmes are available to watch live, check the 'Are all programmes that are broadcast available on BBC iPlayer?' FAQ 👉 https://bbc.in/2m8ks6v.

Children are special patients, and their medical needs are unique, including their surgical needs. At UNC Hospitals, an expert and experienced team of physicians treat children in a kid-friendly and family-centered environment. UNC Pediatric Surgeon Dr. Timothy Weiner explains
Dr. David Sneed of Aesthetica Med Spa in Austin discusses the latest liposuction technique known as Body Jet Water Liposuction - which is quickly gaining popularity due to the procedure being less invasive than traditional liposuction techniques, therefore minimizing recovery time and pain.

Childbirth (also called labour, birth, partus or parturition) is the culmination of a human pregnancy or gestation period with the birth of one or more newborn infants from a woman's uterus. The process of normal human childbirth is categorized in three stages of labour: the shortening and dilation of the cervix, descent and birth of the infant, and birth of the placenta. In many cases, with increasing frequency, childbirth is achieved through caesarean section, the removal of the neonate through a surgical incision in the abdomen, rather than through vaginal birth. In the U.S. and Canada it represents nearly 1 in 3 (31.8%) and 1 in 4 (22.5%) of all childbirths, respectively.

For a full Surgical Airway Techniques resource: https://bit.ly/2rb9Nud
Video courtesy of Gauri Mankekar, MBBS, MS, PhD

We will show you what a sports hernia examination (aka athletic pubalgia, gilmore's groin, lower abdominal pain) and rule out a diagnosis of hip impingement. Rehab exercises are suggested based on the results.
If you're experiencing any of these symptoms, don't hesitate to schedule a sports hernia examination. I can help you determine the best treatment plan to promote your recovery and avoid future injury. Subscribe to my channel to stay updated on the latest medical news and tips!
If you would like to know more about sports hernias and other diagnoses for front of hip, groin, adductor and lower abdominal strain, watch our detailed webinar here: https://bit.ly/37thtNF
For treatment, come visit us or schedule a virtual session. www.p2sportscare.com
Costa Mesa CA 715-502-4243
#sportshernia #abdominal #hippain
Sports Hernia Diagnosis
What Is A Sports Hernia?
A sports hernia is tearing of the transversalis fascia of the lower abdominal or groin region. A common misconception is that a sports hernia is the same as a traditional hernia. The mechanism of injury is rapid twisting and change of direction within sports, such as football, basketball, soccer and hockey.
The term “sports hernia” is becoming mainstream with more professional athletes being diagnosed. The following are just to name a few:
Torii Hunter
Tom Brady
Ryan Getzlaf
Julio Jones
Jeremy Shockey
If you follow any of these professional athletes, they all seem to have the same thing in common: Lingering groin pain. If you play fantasy sports, this is a major headache since it seems so minor, but it can land a player on Injury Reserve on a moments notice. In real life, it is a very frustrating condition to say the least. It is hard to pin point, goes away with rest and comes back after activity, but is hardly painful enough to make you want to stop. It lingers and is always on your mind. And if you’re looking for my step-by-step sports hernia rehab video course here it is.
One the best definitions of Sport hernias is the following by Harmon:
The phenomena of chronic activity–related groin pain that it is unresponsive to conservative therapy and significantly improves with surgical repair.”
This is truly how sports hernias behave in a clinical setting. It is not uncommon for a sports hernia to be unrecognized for months and even years. Unlike your typical sports injury, most sports medicine offices have only seen a handful of cases. It’s just not on most doctors’ radar. The purpose of this article is not only to bring awareness about sports hernias, but also to educate.
Will you find quick fixes in this article for sports hernia rehab?
Nope. There is no quick fix for this condition, and if someone is trying to sell you one, they are blowing smoke up your you-know-what.
Is there a way to decrease the pain related to sports hernias?
Yes. Proper rehab and avoidance of activity for a certain period of time will assist greatly, but this will not always stop it from coming back. Pain is the first thing to go and last thing to come. Do not be fooled when you become pain-free by resting it. Pain is only one measure of improvement in your rehab. Strength, change of direction, balance and power (just to name a few) are important, since you obviously desire to play your sport again. If you wanted to be a couch potato, you would be feeling better in no time. Watching Sports Center doesn’t require any movement.
Why is this article so long?
There is a lot of information on sports hernias available to you on the web. However, much of the information is spread out all over the internet and hard for athletes to digest due to complicated terminology. This article lays out the foundational terminology you will need to understand what options you have with your injury. We will go over anatomy, biomechanics, rehab, surgery, and even the fun facts. The information I am using is from the last ten years of medical research, up until 2016. We will be making updates overtime when something new is found as well. So link to this page and share with friends. This is the best source for information on sports hernias you will find.
Common Names (or Aliases?) for Sports Hernias
Sportsman’s Hernia
Athletic Pubalgia
Gilmore’s Groin
How Do You Know If You Have A Sports Hernia?
Typical athlete characteristics:
Male, age mid-20s
Common sports: soccer, hockey, tennis, football, field hockey
Motions involved: cutting, pivoting, kicking and sharp turns
Gradual onset
How A Sports Hernia Develops
Chronic groin pain typically happens over time, which is why with sports hernias, we do not hear many stories of feeling a “pop” or a specific moment of injury. It is the result of “overuse” mechanics stemming from a combination of inadequate strength and endurance, lack of dynamic control, movement pattern abnormalities, and discoordination of motion in the groin area.
#SPORTSHERNIAEXAM #california
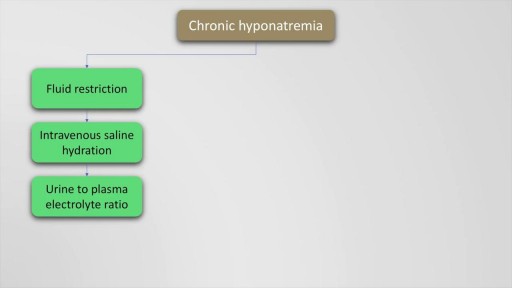
Hyponatremia is defined as a serum sodium of less than 135 Meq per litre and occurs in upto 22 % of hospitalised patients. The causes of hyponatremia may be understood based on the pre-existing volume status of the patient which may either be hypovolemic, euvolemic or hypervolemic hyponatremia. This presentation discusses in detail, the causes of these underlying conditions. Also mentioned are the clinical features and management options and therapeutic sodium targets in patients with hyponatremia. Drugs such as demeclocycline and vaptans (Tolvaptan, Conivaptan) are also mentioned as management options which may be used on a case to case basis. Finally, the all important targets of sodium correction over 24 hours are also mentioned, along with a practical formula for calculation of sodium deficit which is explained with an example.
Hepatitis B is a serious disease caused by a virus that attacks the liver. The virus, which is called hepatitis B virus (HBV), can cause lifelong infection, cirrhosis (scarring) of the liver, liver cancer, liver failure, and death. Hepatitis B vaccine is available for all age groups to prevent HBV infection.
Uterine fibroids are noncancerous growths of the uterus that often appear during childbearing years. Also called leiomyomas (lie-o-my-O-muhs) or myomas, uterine fibroids aren't associated with an increased risk of uterine cancer and almost never develop into cancer. Fibroids range in size from seedlings, undetectable by the human eye, to bulky masses that can distort and enlarge the uterus. You can have a single fibroid or multiple ones. In extreme cases, multiple fibroids can expand the uterus so much that it reaches the rib cage. Many women have uterine fibroids sometime during their lives. But most women don't know they have uterine fibroids because they often cause no symptoms. Your doctor may discover fibroids incidentally during a pelvic exam or prenatal ultrasound.
If it is not removed, tooth decay will begin. The acids in plaque damage the enamel covering your teeth. It also creates holes in the tooth called cavities. Cavities usually do not hurt, unless they grow very large and affect nerves or cause a tooth fracture.
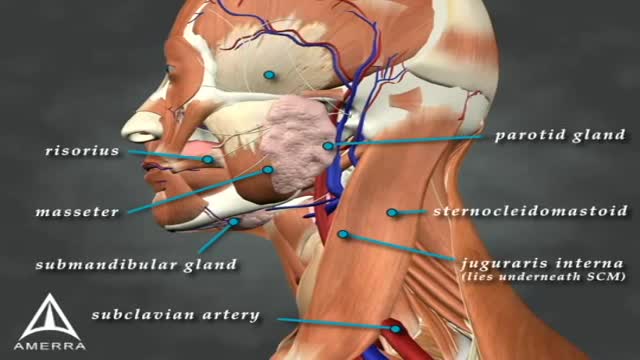
Sialorrhea or excessive drooling is a major issue in children with cerebral palsy and adults with neurodegenerative disorders. In this review, we describe the clinical features, anatomy and physiology of sialorrhea, as well as a review of the world literature on medical treatment using Yale University’s search engine; including but not limited to Medline and Erasmus. Level of drug efficacy is defined according to the guidelines of American Academy of Neurology. Current medical management is unsatisfactory. Topical agents (scopolamine and tropicamide) and oral agents (glyccopyrolate) combined render a level B evidence (probably effective); however, this treatment is associated with troublesome side effects. Double-blind and placebo-controlled studies of botulinum toxin (BoNT) provide a level A evidence for type B (two class I studies; effective and established) and both overall and individual B level of evidence for OnabotulinumtoxinA (A/Ona) and AbobotulinumtoxinA (A/Abo); these are probably effective. For IncobotulinumtoxinA (A/Inco), the level of evidence is U (insufficient) due to lack of blinded studies. Side effects are uncommon; transient and comparable between the two types of toxin. A clinical note at the end of this review comments on fine clinical points. Administration of BoNTs into salivary glands is currently the most effective way of treating sialorrhea.