Top videos
A hematoma is a common complication of surgical procedures. A large, expanding hematoma can result in necrosis of the overlying skin (1,2) or adjacent subcutaneous fat, increased incidence of infection, scarring, skin hyperpigmentation, tissue edema and a prolonged convalescence.

Overview
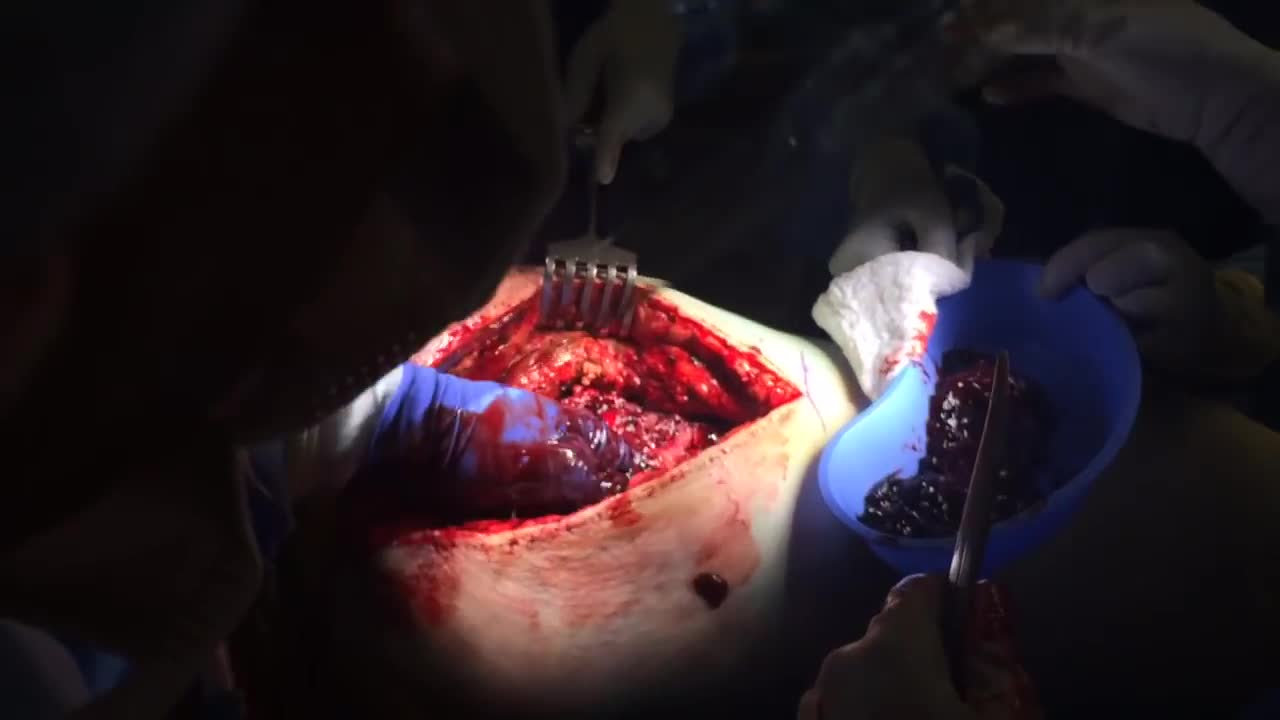
Heart bypass surgery creates a new route, called a bypass, for blood and oxygen to reach the heart.
Heart bypass surgery begins with an incision in the chest, and the breastbone is cut exposing the heart. Next, a portion of the saphenous vein, which is very large, is harvested from the inside of the leg. Pieces of this large vein are used to bypass the blocked coronary arteries, which are arteries that supply blood to the heart. The venous graft is sewn to the aorta, the main artery of the body, and to the affected coronary artery, to bypass the blocked site.
The internal mammary artery from the chest may also be used to bypass a clogged artery.
Several arteries may be bypassed depending on the condition of the heart. After the graft is created, the breastbone and chest are closed.

This video - produced by students at Oxford University Medical School - demonstrates how to perform an examination of the respiratory system. It also indicates common pathologies encountered. It is part of a series of videos covering basic clinical examinations and is linked to Oxford Medical Education (www.oxfordmedicaleducation.com).

A VCUG (Voiding Cystourethrogram) is a test that looks at how well your child's kidneys, ureters and bladder are working. Your child's kidneys make urine. The urine flows from the kidneys through thin tubes (called ureters) into your child's bladder.

Function and Anatomy: The hip is a ball and socket type joint, formed by the articulation of the head of the femur with the pelvis. Normal range of motion includes: abduction 45 degrees, adduction 20-30 degrees, flexion 135 degrees, extension 30 degrees, internal and external rotation. Hip pathology can cause symptoms anywhere around the joint, though frequently pain is anterior and radiates to the groin region. Additionally, pathology outside of the hip can be referred to this region. History and exam obviously help in making these distinctions.

Thoracentesis is a procedure used to obtain a sample of fluid from the space around the lungs. Normally, only a thin layer of fluid is present in the area between the lungs and chest wall. However, some conditions can cause a large amount of fluid to accumulate. This collection of fluid is called a pleural effusion.

Surgery to treat men with prostate cancer is often followed by months of difficulty controlling urine flow, a condition known as urinary incontinence. But new research suggests that this problem may go away more quickly if the men perform certain exercises to strengthen their pelvic floor muscles.
Researchers from the Kaiser Permanente Medical Center in Los Angeles, California, found that men who were taught how to perform pelvic floor exercises before and after surgery were more likely to have regained continence three months later.
Men Doing Pelvic Exercises Recover Earlier
In the current study, the researchers randomly assigned 38 men scheduled for radical prostatectomy to either a treatment group or a control group. The men in the treatment group were referred to a physical therapist. They were instructed how to do Pelvic Floor Exercises both before and after surgery, using biofeedback to ensure they were using the proper muscles. The control group did not receive any formal instruction. All of the men completed questionnaires regarding bladder function at regular intervals over the next year.
Overall, 82% of the patients had regained continence (defined as not needing to use any absorbent pads) by the end of the year, including about equal numbers in both groups. But on average the men who had been educated about Pelvic exercises regained continence about one month earlier than those in the control group (at 12 weeks vs. 16 weeks).
Most of the men who did not regain continence within a year were still using at least three absorbent pads a day, indicating continued severe incontinence. The study authors explained that these men probably had extensive damage to the bladder sphincter or severe dysfunction of the bladder after surgery, and the exercises alone were unable to compensate for this.
But the exercises seemed to be effective. Pelvic floor exercise and education initiated prior to surgery is an effective noninvasive intervention useful for improving early return of urinary continence, the authors concluded. It would certainly have a positive impact on our patients undergoing radical prostatectomy in an effort to improve quality of life after major urological surgery.
The results of the study were published in the Journal of Urology (Vol. 170, No. 1: 130-133)

Candida Albicans is more than just yeast- for most people, it's already mutated into a more aggressive fungal form that eats holes through the intestinal tract causing many of todays health problems like food allergies, autoimmune disorders, Crohn's disease, IBS, low energy and many more aggressive diseases. People need to know what it is and what to do about it.

Get a 60-day free trial at https://shipstation.com/doctormike. Thanks to ShipStation for sponsoring the show!
I’ll teach you how to become to media’s go-to expert in your field. Enroll in The Professional’s Media Academy now: https://www.professionalsmediaacademy.com/
Listen to my podcast, @DoctorMikeCheckup, here:
Spotify: https://go.doctormikemedia.com..../spotify/CheckUpSpot
Apple Podcasts: https://go.doctormikemedia.com..../applepodcast/AppleP
Body Bizarre is a TLC show with a name I'm not too wild about, but with stories that are nonetheless fascinating. Today we look at separating conjoined twins, a girl with ants crawling out of her ears, a man who nearly lost his hand in a factory accident, a family that all has 6 fingers, and more.
Help us continue the fight against medical misinformation and change the world through charity by becoming a Doctor Mike Resident on Patreon where every month I donate 100% of the proceeds to the charity, organization, or cause of your choice! Residents get access to bonus content, an exclusive discord community, and many other perks for just $10 a month. Become a Resident today:
https://www.patreon.com/doctormike
Let’s connect:
IG: https://go.doctormikemedia.com..../instagram/DMinstagr
Twitter: https://go.doctormikemedia.com/twitter/DMTwitter
FB: https://go.doctormikemedia.com/facebook/DMFacebook
TikTok: https://go.doctormikemedia.com/tiktok/DMTikTok
Reddit: https://go.doctormikemedia.com/reddit/DMReddit
Contact Email: DoctorMikeMedia@Gmail.com
Executive Producer: Doctor Mike
Production Director and Editor: Dan Owens
Managing Editor and Producer: Sam Bowers
Editor and Designer: Caroline Weigum
Editor: Juan Carlos Zuniga
* Select photos/videos provided by Getty Images *
** The information in this video is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional **
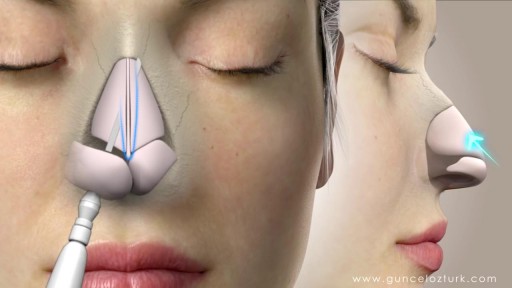
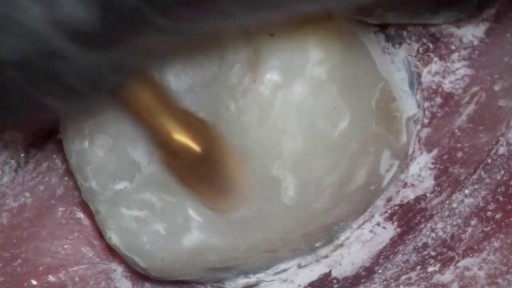
Rhinoplasty, sometimes referred to as a "nose job" or "nose reshaping" by patients, enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. What surgical rhinoplasty can treat Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone's face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion. Rhinoplasty to correct a deviated septum Nose surgery that's done to improve an obstructed airway requires careful evaluation of the nasal structure as it relates to airflow and breathing. Correction of a deviated septum, one of the most common causes of breathing impairment, is achieved by adjusting the nasal structure to produce better alignment.
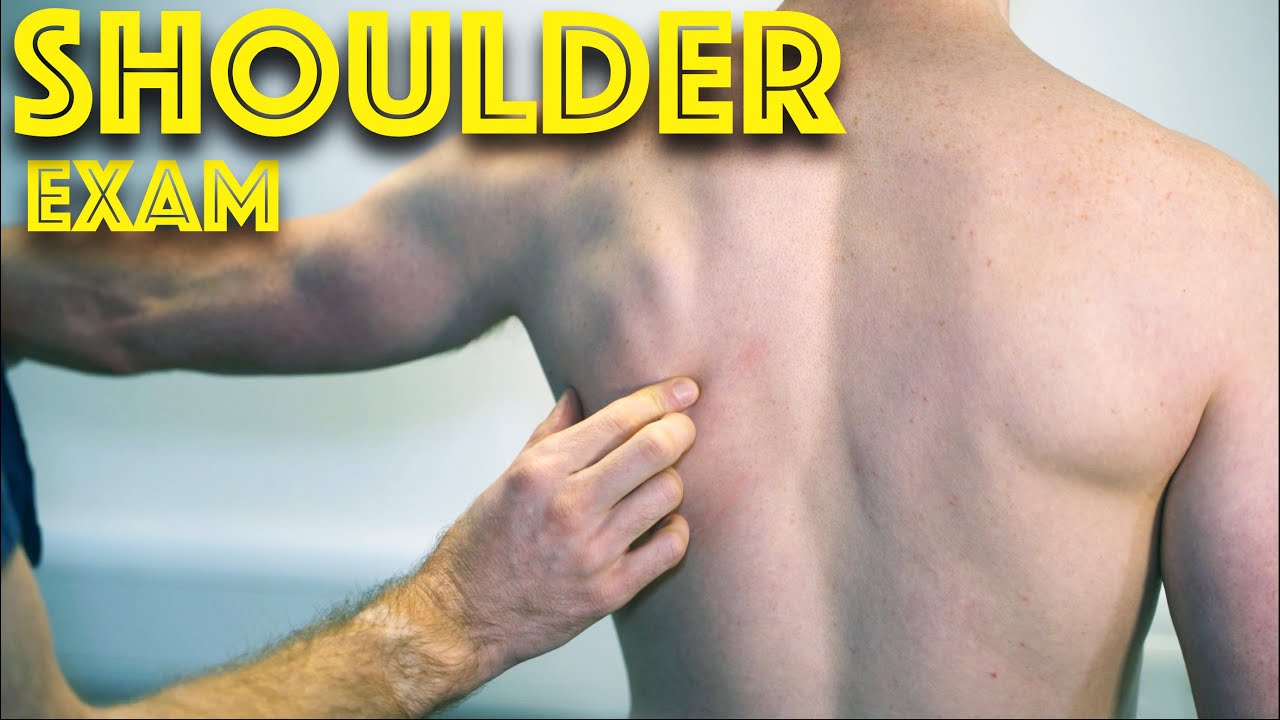
Shoulder Clinical Examination - Medical School Clinical Skills - Dr Gill
Personally, I find the shoulder examination the most complex examination possibly as there are so many variations and special tests. Some of which overlap and some will relate specifically to a patients presentation.
Often in a medical school syllabus, only select special tests will be used. In this shoulder exam demonstration, we include the Hawkins-Kennedy Test looking for impingement. This is dovetailed with examination for bicipital tendonitis as this is another possible cause of impingement type symptoms.
This shoulder upper limb exam follows the standard "Look, Feel, Move" orthopaedic exam approach, and overall order as set out in MacLeods Clinical Examination
Watch further orthopaedic examinations for your OSCE revision:
The Spine Examination:
https://youtu.be/pJxMHa6SCgU
Knee Examination
https://youtu.be/oyKH4EYfJDM
Hip Joint Clinical Examination
https://youtu.be/JC9GKq5nSdQ
________
Please note that there is no ABSOLUTE way to perform a clinical examination. Different institutions and even clinicians will have differing degrees of variations - the aim is the effectively identify medically relevant signs.
However during OSCE assessments. Different medical schools, nursing colleges, and other health professional courses will have their own preferred approach to a clinical assessment - you should concentrate on THEIR marks schemes for your assessments.
The examination demonstrated here is derived from Macleods Clinical Examination - a recognized standard textbook for clinical skills.
#ShoulderExamination #ClinicalSkills #DrGill

There are lots of fallacies about the missionary position being the best position for getting pregnant. With the woman on her back and her partner on top, it is thought that gravity will assist the sperm to swim upwards towards the egg.