Top videos
A hematoma is a common complication of surgical procedures. A large, expanding hematoma can result in necrosis of the overlying skin (1,2) or adjacent subcutaneous fat, increased incidence of infection, scarring, skin hyperpigmentation, tissue edema and a prolonged convalescence.

The examination room should be quiet, warm and well lit. After you have finished interviewing the patient, provide them with a gown (a.k.a. "Johnny") and leave the room (or draw a separating curtain) while they change. Instruct them to remove all of their clothing (except for briefs) and put on the gown so that the opening is in the rear. Occasionally, patient's will end up using them as ponchos, capes or in other creative ways. While this may make for a more attractive ensemble it will also, unfortunately, interfere with your ability to perform an examination! Prior to measuring vital signs, the patient should have had the opportunity to sit for approximately five minutes so that the values are not affected by the exertion required to walk to the exam room. All measurements are made while the patient is seated. Observation: Before diving in, take a minute or so to look at the patient in their entirety, making your observations, if possible, from an out-of-the way perch. Does the patient seem anxious, in pain, upset? What about their dress and hygiene? Remember, the exam begins as soon as you lay eyes on the patient. Temperature: This is generally obtained using an oral thermometer that provides a digital reading when the sensor is placed under the patient's tongue. As most exam rooms do not have thermometers, it is not necessary to repeat this measurement unless, of course, the recorded value seems discordant with the patient's clinical condition (e.g. they feel hot but reportedly have no fever or vice versa). Depending on the bias of a particular institution, temperature is measured in either Celcius or Farenheit, with a fever defined as greater than 38-38.5 C or 101-101.5 F. Rectal temperatures, which most closely reflect internal or core values, are approximately 1 degree F higher than those obtained orally. Respiratory Rate: Respirations are recorded as breaths per minute. They should be counted for at least 30 seconds as the total number of breaths in a 15 second period is rather small and any miscounting can result in rather large errors when multiplied by 4. Try to do this as surreptitiously as possible so that the patient does not consciously alter their rate of breathing. This can be done by observing the rise and fall of the patient's hospital gown while you appear to be taking their pulse. Normal is between 12 and 20. In general, this measurement offers no relevant information for the routine examination. However, particularly in the setting of cardio-pulmonary illness, it can be a very reliable marker of disease activity. Pulse: This can be measured at any place where there is a large artery (e.g. carotid, femoral, or simply by listening over the heart), though for the sake of convenience it is generally done by palpating the radial impulse. You may find it helpful to feel both radial arteries simultaneously, doubling the sensory input and helping to insure the accuracy of your measurements. Place the tips of your index and middle fingers just proximal to the patients wrist on the thumb side, orienting them so that they are both over the length of the vessel.

The most reliable clinical sign to detect ascites is checking for bilateral flank dullness. If a patient with ascites is lying supine, fluid accumulates in the flank regions, leading to dullness on percussion. At the same time, the air-filled bowel loops are forced upwards by the free fluid due to buoyancy, resulting in tympanitic percussion. To locate specifically where dullness shifts to tympany, or the air-fluid level, percussion should be performed from the sides towards the middle. To confirm that the dullness is caused by ascites, ask the patient to switch to a lateral decubitus position. If ascites is present, the air-filled bowel loops will shift accordingly and remain at the surface of the fluid. As a result, the air-fluid level will shift as well. This is known as shifting dullness.
Subscribe to AMBOSS YouTube for the latest clinical examination videos, medical student interviews, study tips and tricks, and live webinars!
Free 5 Day Trial: https://go.amboss.com/amboss-YT
Instagram: https://www.instagram.com/amboss_med/
Facebook: https://www.facebook.com/AMBOSS.Med/
Twitter: https://twitter.com/ambossmed
Blog: https://blog.amboss.com/us
#AMBOSSMed #ClinicalExamination

I talk about 5 Essential Skills you need as a nurse. These skills are timeless in the fat that you will always need to use them at some level. Of course specific skills are good to have as well but these skills are universal and can help you in other areas of life as well.
NURSING SCHOOL STUDY RESOURCES: https://sellfy.com/nursingschoolstudyNURSING
PHARMACOLOGY: https://sellfy.com/p/fnoy/
INSTAGRAM:https://www.instagram.com/your_mentor_rn/?hl=en
PERSONAL INSTAGRAM: https://www.instagram.com/crosby_steen/
MEDIUM ARTICLES: https://medium.com/@rnacademy1..../7-tips-for-nursing-
AMAZON PRIME STUDENT DISCOUNT: https://amzn.to/2OIleAe
VIDEO GEAR
Camera: G7X Markii - https://amzn.to/2na3OR8
Phone: Galaxy Note 8- https://amzn.to/2nboHM3
Audio: Zoom H4NPro Audio Recorder- https://amzn.to/2vktlf8
Computer: 13 inch Macbook Pro- https://amzn.to/2ndhISw
INSTAGRAM TV https://www.instagram.com/crosby_steen/
Hi Guys! My name is Crosby Steen. I am a Nursing Educator, and ER Travel Nurse. I do videos on daily science based news and travel, with the goal of providing value for you in science based education and travel nursing. Any questions hit me up in the comments or Email below.....
PRIVATE TUTORING OR VIDEO REQUESTS CONTACT:
crosby.steen@gmail.com
MUSIC BY: https://andrewapplepie.com/ and copyrighted by Epidemic Sound
Music by Joakim Karud http://youtube.com/joakimkarud
Music by DJ Quads

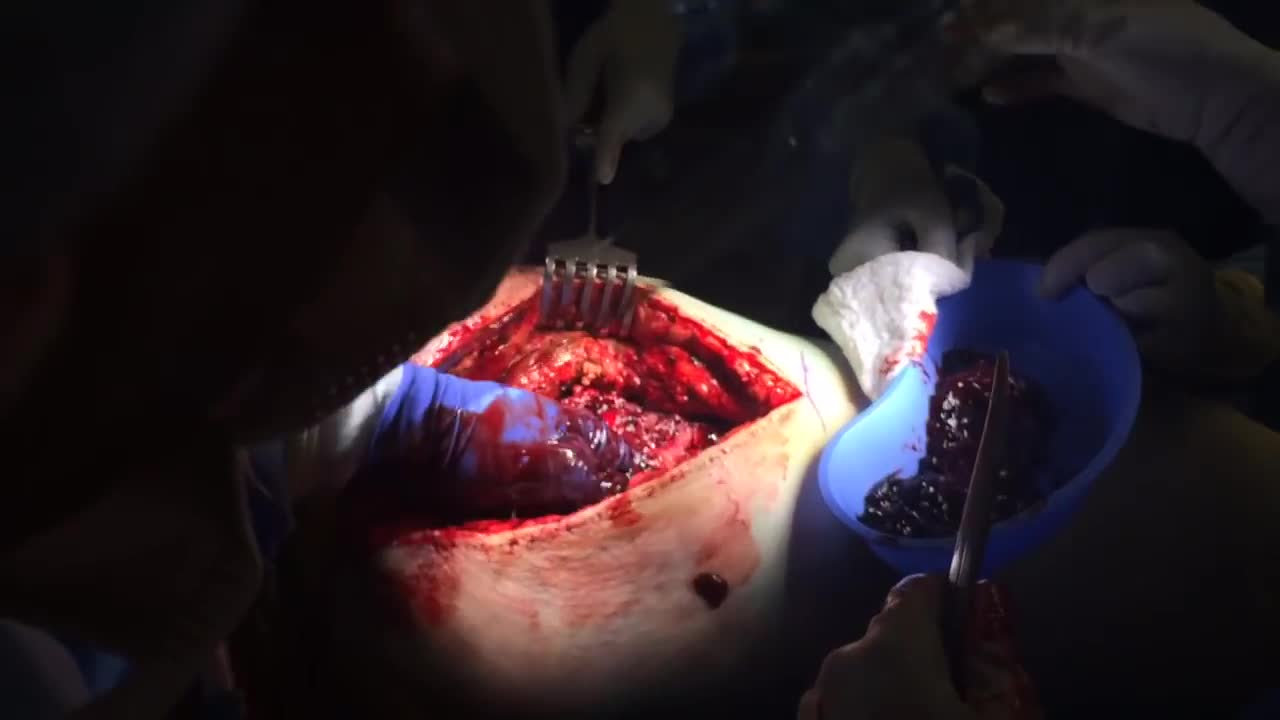
Join Dr. Parsia Vagefi, Chief of Surgical Transplantation and Dr. Steven Hanish, Surgical Director of Liver Transplantation, as they grant unprecedented access to the OR while performing a #Liver #Transplant #Surgery.
To find out more about UT Southwestern's transplant programs visit:
https://www.utswmed.org/transplant

In this video, we show a sports hernia self treatment we give many of our clients. It is not the only part of treatment. Grabbing the skin around the region of the groin strain can reduce pain and stiffness with turning and twisting. Sports hernias are often misdiagnosed with hip labrum tears, hip impingement, adductor tendonitis and abdominal strains.
Want more information? We have a more detailed free webinar on our page here. https://bit.ly/37thtNF
Want some treatment or suggestions of exercises or stretches? Contact us! We have in-person and virtual sessions.
Costa Mesa CA 715-502-4243 www.p2sportscare.com
Sports Hernia Diagnosis
What Is A Sports Hernia?
A sports hernia is tearing of the transversalis fascia of the lower abdominal or groin region. A common misconception is that a sports hernia is the same as a traditional hernia. The mechanism of injury is rapid twisting and change of direction within sports, such as football, basketball, soccer and hockey.
The term “sports hernia” is becoming mainstream with more professional athletes being diagnosed. The following are just to name a few:
Torii Hunter
Tom Brady
Ryan Getzlaf
Julio Jones
Jeremy Shockey
If you follow any of these professional athletes, they all seem to have the same thing in common: Lingering groin pain. If you play fantasy sports, this is a major headache since it seems so minor, but it can land a player on Injury Reserve on a moments notice. In real life, it is a very frustrating condition to say the least. It is hard to pin point, goes away with rest and comes back after activity, but is hardly painful enough to make you want to stop. It lingers and is always on your mind. And if you’re looking for my step-by-step sports hernia rehab video course here it is.
One the best definitions of Sport hernias is the following by Harmon:
The phenomena of chronic activity–related groin pain that it is unresponsive to conservative therapy and significantly improves with surgical repair.”
This is truly how sports hernias behave in a clinical setting. It is not uncommon for a sports hernia to be unrecognized for months and even years. Unlike your typical sports injury, most sports medicine offices have only seen a handful of cases. It’s just not on most doctors’ radar. The purpose of this article is not only to bring awareness about sports hernias, but also to educate.
Will you find quick fixes in this article for sports hernia rehab?
Nope. There is no quick fix for this condition, and if someone is trying to sell you one, they are blowing smoke up your you-know-what.
Is there a way to decrease the pain related to sports hernias?
Yes. Proper rehab and avoidance of activity for a certain period of time will assist greatly, but this will not always stop it from coming back. Pain is the first thing to go and last thing to come. Do not be fooled when you become pain-free by resting it. Pain is only one measure of improvement in your rehab. Strength, change of direction, balance and power (just to name a few) are important, since you obviously desire to play your sport again. If you wanted to be a couch potato, you would be feeling better in no time. Watching Sports Center doesn’t require any movement.
Why is this article so long?
There is a lot of information on sports hernias available to you on the web. However, much of the information is spread out all over the internet and hard for athletes to digest due to complicated terminology. This article lays out the foundational terminology you will need to understand what options you have with your injury. We will go over anatomy, biomechanics, rehab, surgery, and even the fun facts. The information I am using is from the last ten years of medical research, up until 2016. We will be making updates overtime when something new is found as well. So link to this page and share with friends. This is the best source for information on sports hernias you will find.
Common Names (or Aliases?) for Sports Hernias
Sportsman’s Hernia
Athletic Pubalgia
Gilmore’s Groin
How Do You Know If You Have A Sports Hernia?
Typical athlete characteristics:
Male, age mid-20s
Common sports: soccer, hockey, tennis, football, field hockey
Motions involved: cutting, pivoting, kicking and sharp turns
Gradual onset
How A Sports Hernia Develops
Chronic groin pain typically happens over time, which is why with sports hernias, we do not hear many stories of feeling a “pop” or a specific moment of injury. It is the result of “overuse” mechanics stemming from a combination of inadequate strength and endurance, lack of dynamic control, movement pattern abnormalities, and discoordination of motion in the groin area.
#sportsherniadiagnosisselftreatment #sportshernia #california

Identify the anatomy and explain the physiology of the scrotum on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the scrotum.
Identify and describe sonographic images of congenital abnormalities of the scrotum.
Identify and describe sonographic images of pathologies of the scrotum.
Identify and describe sonographic images of extratesticular disease processes.
Identify the anatomy and explain the physiology of the prostate on diagrams and sonograms.
Describe and demonstrate the protocol for transabdominal and endorectal sonographic scanning of the prostate.
Identify and describe sonographic images of benign and malignant pathologies of the prostate, including benign hyperplasia, prostatitis, carcinoma, and calculi.
Explain the technique for prostate biopsy.
Define the criteria for an ultrasound appearance of prostate tumor staging.
Explain the technique for radiation seed implantation.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).
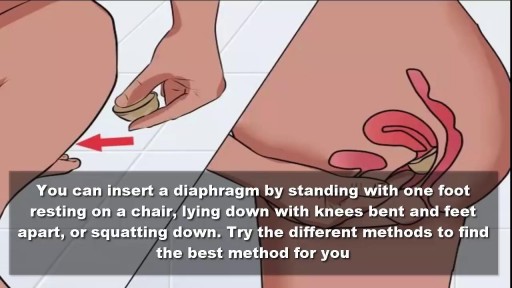
To use the diaphragm, first cover the inside of it with spermicide. Then insert it into your vagina so that it covers your cervix. You can insert the diaphragm up to 6 hours before sex. You should leave it in for at least 6 hours after the last time you have sex.