Top videos
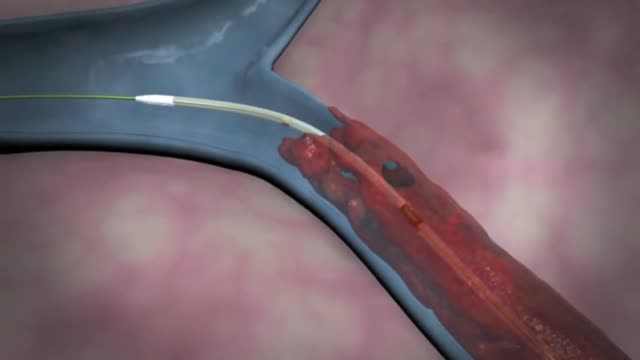
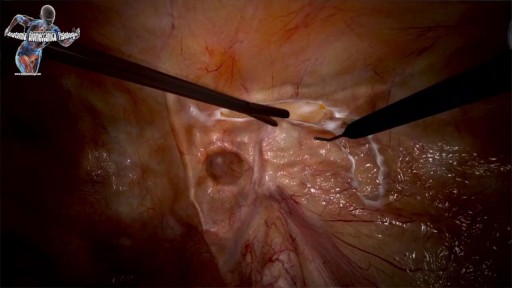
Although individual surgeons and centers employ different methods to insert a left ventricular assist device (LVAD), the fundamental concepts remain true for all. That is, most devices use the apex of the left ventricle (LV) as the inflow site to the pump, which subsequently gives off an outflow graft to the aorta, thus bypassing the ailing LV. Currently available devices do not differ significantly with regard to general implantation technique. The sequence of implantation can vary also from patient to patient, depending on the particular situation. In some cases, concomitant procedures may be performed in conjunction with LVAD implantation without adversely affecting outcome.

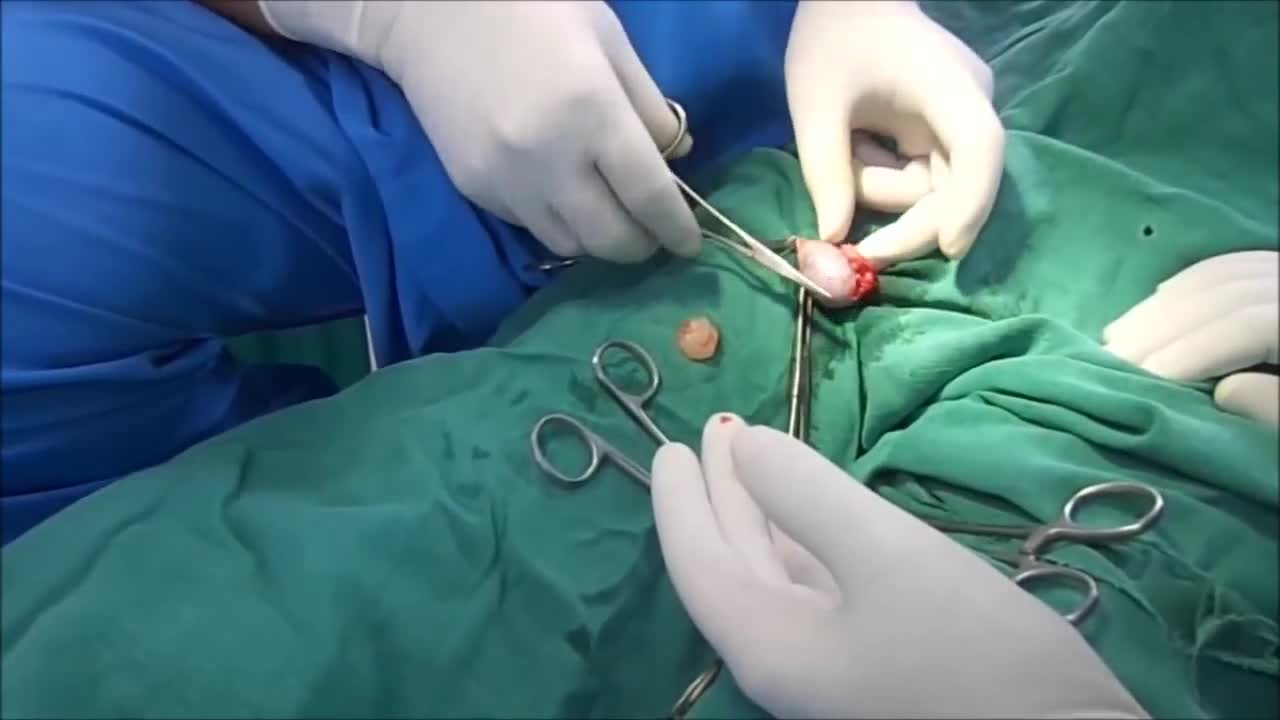
Hardware removals are among the most commonly performed surgical procedures worldwide. Current literature offers little data concerning postoperative patient satisfaction. The purpose of our study was to evaluate the patients’ point of view on implant removal. watch to learn more.

The gastric balloon procedure (endoscopic intragastric balloon) leaves an inflated silicon balloon in the stomach for 6 months, making less room for food. As a result, patients: Feel full sooner while eating and therefore eat less. Lose about 30% of their excess weight in 6 months.

An abscess is a tender mass generally surrounded by a colored area from pink to deep red. Abscesses are often easy to feel by touching. The middle of an abscess is full of pus and debris. Painful and warm to touch, abscesses can show up any place on your body. The most common sites are in your armpits (axillae), areas around your anus and vagina(Bartholin gland abscess), the base of your spine (pilonidal abscess), around a tooth (dental abscess), and in your groin. Inflammation around a hair follicle can also lead to the formation of an abscess, which is called a boil (furuncle).
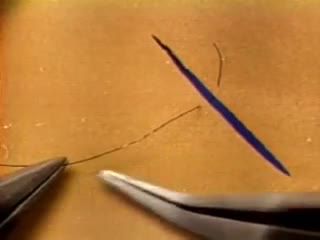
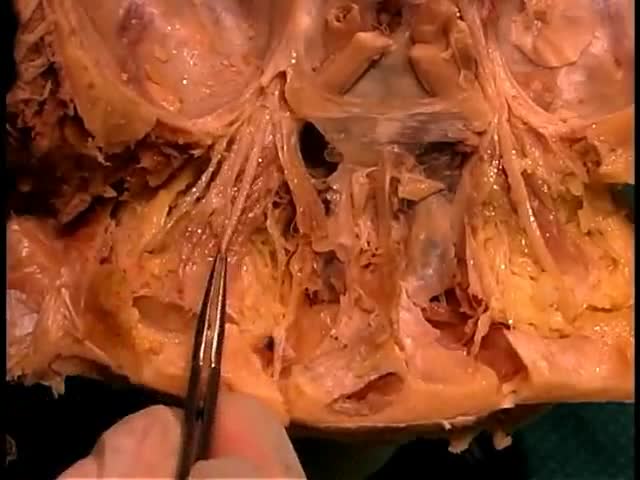
The needle should pass through the tissue at a perpendiculaPlace the tips of the left-hand forceps on the underside of the tissue at the point where the needle will enter, and gently push the edge upward. With the right hand, bring the needle into contact with the tissue, and press downward. These movements create eversion. Pass the needle through. Do not grab the tissue with your left hand forceps since it will damage the intima. If needed, you can pick up adventitia or a nearby suture to help with exposure and eversion. r.The needle must pass through the other side at a perpendicular, too. Bring the tip of the needle to the place where you intend to bring it out on the other side. Put the tip of your left-hand forceps on the upper surface of the tissue at the intended exit point. Press down with the left-hand forceps and push up with the needle to give you the correct eversion. The width of the bite should be about three times the thickness of the needle. The bites on both sides must be equal, and the needle should cross exactly in a straight line (not diagonally). Pull the needle through the tissue following the curve of the needle
The future of Medicine - Il futuro della medicina - Die Zukunft der Medizin: High Tech, Robots, VR ⚡️Anatomia Biomeccanica Fisiologia by Ticinosthetics: tutto gira attorno alla palestra ©️2017 - www.ticinostheticsgs.com

How to use a Hepatitis B rapid test kit for self-diagnosis of Hepatitis B (fingerstick blood). Convenient, Easy to Use, and over 98% Accurate. Certified GMP and ISO13485. Test yourself at home with Complete Privacy. Buy online today at: http://www.stdrapidtest.com
Like any syndrome, fetal alcohol syndrome (FAS) is a group of signs and symptoms that appear together and indicate a certain condition. In the case of FAS, the signs and symptoms are birth defects that result from a woman's use of alcohol during her pregnancy.