Top videos
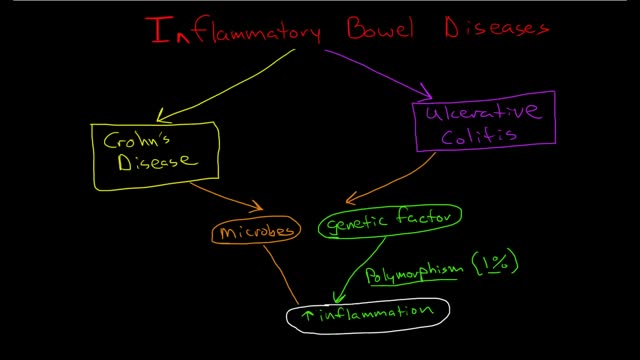
Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of your digestive tract. IBD primarily includes ulcerative colitis and Crohn's disease. Both usually involve severe diarrhea, pain, fatigue and weight loss. IBD can be debilitating and sometimes leads to life-threatening complications. Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease that causes long-lasting inflammation and sores (ulcers) in the innermost lining of your large intestine (colon) and rectum. Crohn's disease is an IBD that cause inflammation of the lining of your digestive tract. In Crohn's disease, inflammation often spreads deep into affected tissues. The inflammation can involve different areas of the digestive tract — the large intestine, small intestine or both. Collagenous (kuh-LAJ-uh-nus) colitis and lymphocytic colitis also are considered inflammatory bowel diseases but are usually regarded separately from classic inflammatory bowel disease.
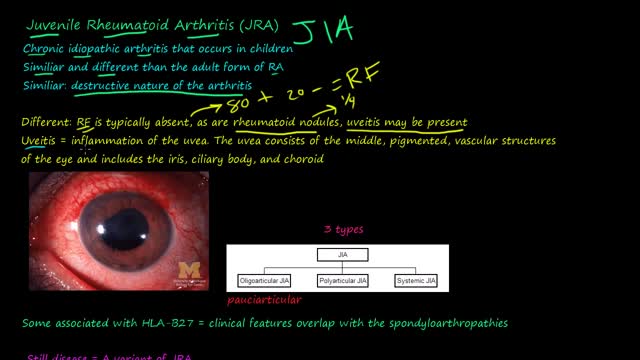
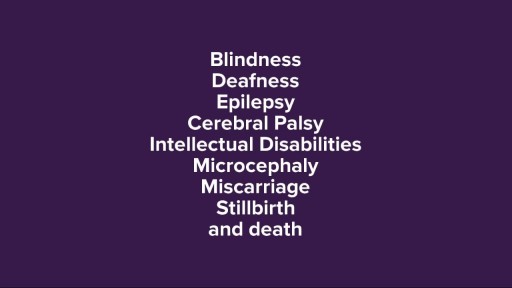
Juvenile rheumatoid arthritis, also known as juvenile idiopathic arthritis, is the most common type of arthritis in children under the age of 17. Juvenile rheumatoid arthritis causes persistent joint pain, swelling and stiffness. Some children may experience symptoms for only a few months, while others have symptoms for the rest of their lives. Some types of juvenile rheumatoid arthritis can cause serious complications, such as growth problems and eye inflammation. Treatment of juvenile rheumatoid arthritis focuses on controlling pain, improving function and preventing joint damage.

Colorectal cancer (also known as colon cancer, rectal cancer or bowel cancer) is the development of cancer in the colon or rectum (parts of the large intestine). It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body. People with HNPCC tend to develop colon cancer before age 50. Familial adenomatous polyposis (FAP). FAP is a rare disorder that causes you to develop thousands of polyps in the lining of your colon and rectum. People with untreated FAP have a greatly increased risk of developing colon cancer before age 40.
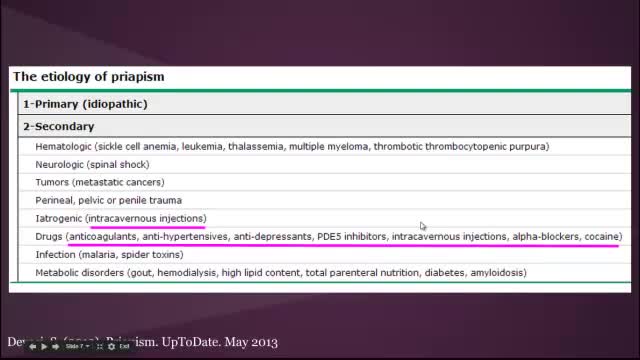
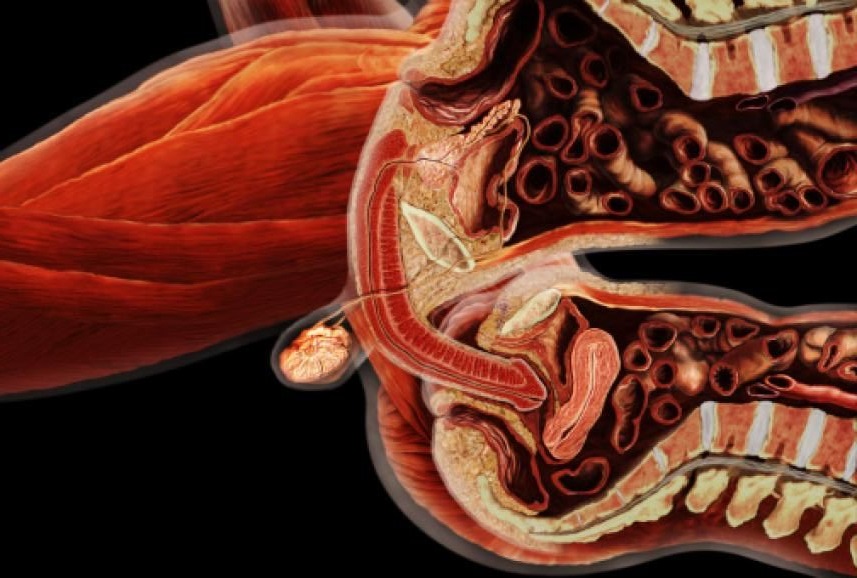
Priapism is a prolonged erection of the penis. The persistent erection continues hours beyond or isn't caused by sexual stimulation. Priapism is usually painful. Although priapism is an uncommon condition overall, it occurs commonly in certain groups, such as people who have sickle cell anemia. Prompt treatment for priapism is usually needed to prevent tissue damage that could result in the inability to get or maintain an erection (erectile dysfunction). Priapism is most common in men in their 30s.
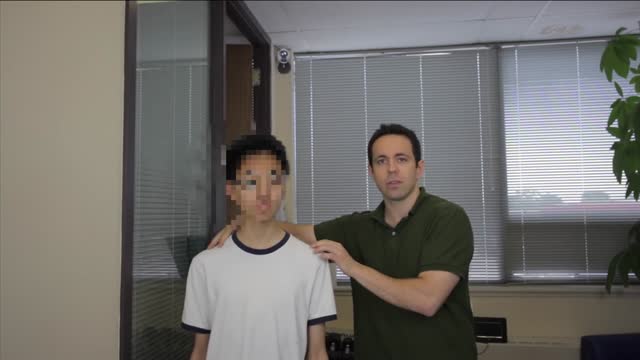
Scoliosis is a sideways curvature of the spine that occurs most often during the growth spurt just before puberty. While scoliosis can be caused by conditions such as cerebral palsy and muscular dystrophy, the cause of most scoliosis is unknown.
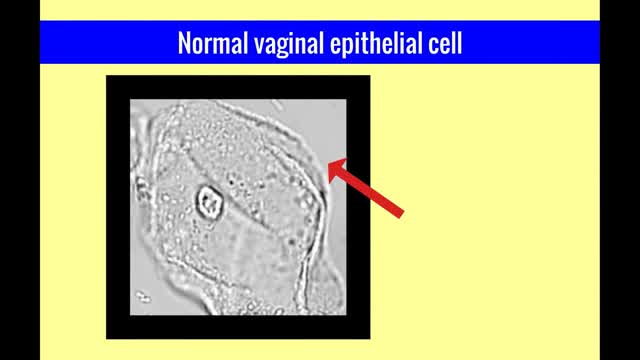
The vulvar vaginal diseases service sees referrals to help women with short--and long--term problems of the outer genital area (vulva), vagina and pelvic floor muscles including: Vulvar vaginal burning, itching, irritation and pain Vulvar Vestibulitis Pain with intercourse Discharge Yeast infections Bacterial vaginosis Pelvic floor muscle dysfunction A patient must be referred by her local health care provider. Services include: Skin care education Examinations-Your healthcare provider will examine you and talk with you about recommendations for treatment and/or management of your symptoms. Some vulvar diseases require a biopsy to diagnose the condition. Referrals-Your healthcare team may refer you to other specialists, including physical therapists or health psychologists. Separate insurance authorization is necessary for these services. The clinic staff provides general education and support to help women cope with these very personal health problems. Following a clinic visit, a letter is promptly sent to your local health care provider. The letter provides the results of your exam and the plan of care.
Patent ductus arteriosus (PDA), in which there is a persistent communication between the descending thoracic aorta and the pulmonary artery that results from failure of normal physiologic closure of the fetal ductus (see image below), is one of the more common congenital heart defects.

Euthyroid sick syndrome (ESS), sick euthyroid syndrome (SES), thyroid allostasis in critical illness, tumours, uremia and starvation (TACITUS), non-thyroidal illness syndrome (NTIS) or low T3 low T4 syndrome is a state of adaptation or dysregulation of thyrotropic feedback control where the levels of T3 and/or T4 are ...

Interventional Nephrology is a new and emerging subspecialty of Nephrology that mainly deals with ultrasonography of kidneys and ultrasound-guided renal biopsy, insertion of peritoneal dialysis catheters, tunneled dialysis catheters as a vascular access for patients undergoing hemodialysis as well as percutaneous ...

A bilateral complete cleft lip, which has been previously treated with nasoalvoelar molding, is repaired with the Millard-Mulliken technique, which employs reconstruction of the orbicularis oris muscle by advancing bilateral muscular segments. This tutorial for medical professionals was developed to supplement learning of a common surgical technique and is not intended to replace formal surgical training. This slideshow is primarily intended for use on tablets or larger screens. Some detail might be lost on mobile screens.

This is a 60 year man having large swelling of size 7cm x 5 cm behind neck for one year. Patient complained pain and tenderness over local area for 7 days and came to us.On examination punctum found in the centre of swelling and fluctuation positive.Infected sebaceous cyst diagnosis made. Incision and drainage surgery done under local anesthesia.all infected pultaceous material evacuated.Pus culture sent and antibiotics given as per sensitivity report. Patient improved with daily dressing.

Gallstone ileus is an important, though infrequent, cause of mechanical bowel obstruction, affecting older adult patients who often have other significant medical conditions. It is caused by impaction of a gallstone in the ileum after being passed through a biliary-enteric fistula. The diagnosis is often delayed since symptoms may be intermittent and investigations fail to identify the cause of the obstruction. The mainstay of treatment is removal of the obstructing stone after resuscitating the patient. Gallstone ileus continues to be associated with relatively high rates of morbidity and mortality.

Peritoneal dialysis (per-ih-toe-NEE-ul die-AL-uh-sis) is a way to remove waste products from your blood when your kidneys can no longer do the job adequately. A cleansing fluid flows through a tube (catheter) into part of your abdomen and filters waste products from your blood. After a prescribed period of time, the fluid with filtered waste products flows out of your abdomen and is discarded. Peritoneal dialysis differs from hemodialysis, a more commonly used blood-filtering procedure. With peritoneal dialysis, you can give yourself treatments at home, at work or while traveling. Peritoneal dialysis isn't an option for everyone wit
Uterine fibroids are noncancerous growths of the uterus that often appear during childbearing years. Also called leiomyomas (lie-o-my-O-muhs) or myomas, uterine fibroids aren't associated with an increased risk of uterine cancer and almost never develop into cancer. Fibroids range in size from seedlings, undetectable by the human eye, to bulky masses that can distort and enlarge the uterus. You can have a single fibroid or multiple ones. In extreme cases, multiple fibroids can expand the uterus so much that it reaches the rib cage. Many women have uterine fibroids sometime during their lives. But most women don't know they have uterine fibroids because they often cause no symptoms. Your doctor may discover fibroids incidentally during a pelvic exam or prenatal ultrasound.