Top videos

Ellis Parker MSN, RN-BC, CNE, CHSE covers Incentive Spirometry. The Critical Nursing Skills - Shorts series is intended to help RN and PN nursing students study for nursing school exams, including the ATI, HESI and NCLEX.
#NCLEX #HESI #Kaplan #ATI #NursingSchool #NursingStudent #Nurse #RN #PN #Education #LVN #LPN #clinicalskills #safety
Comments? Suggestions? Please share! Your feedback can help inform our future videos and study resources. 🙂
🤔🤔🤔 DO YOU WANT TO PASS your classes, proctored exams and the NCLEX? 🤔🤔🤔 Our flashcards are the best you can buy. They are built with a single goal: help you pass with no fluff. Everything you need, and nothing you don’t. Don’t take our word for it, though! Check out our hundreds of 5-star reviews from nurses who passed their exams and the NCLEX with Level Up RN.
Our #Clinical Nursing Skills Flashcards are available at
➡️ https://bit.ly/clinicalnursingskills
👇SHOP ALL OUR FLASHCARDS👇
http://bit.ly/allstudycards
🗂️ Our Ultimate Nursing School Survival kit is your number 1 resource to get through nursing school and to pass the NCLEX. Whether you're just starting school or you’re already prepping for the NCLEX, this bundle of flashcards is the best you can buy. It covers all the information you need to know to pass all your exams and it has FREE shipping!
➡️ https://bit.ly/TUNSSK ⬅️
📧 LOOKING FOR FREE RESOURCES TO HELP WITH YOUR EXAMS? Get exclusive tips, latest video releases and more delivered to your email!
➡️ https://www.leveluprn.com/signup ⬅️
Want perks? Join our channel!
➡️ https://www.youtube.com/leveluprn/join ⬅️
👩⚕️ LEVEL UP NURSE SQUAD 👩⚕️
All of the nurses at Level Up RN are here to help! Cathy Parkes started helping her fellow classmates back when she was in nursing school, tutoring so they could pass their exams and graduate. After she got her BSN and started working as an RN at Scripps Encinitas Hospital, she started this YouTube channel to help nursing students around the world. Since then she has built a team of top-notch dedicated nurses and nurse educators who are focused on improving nursing education and supporting career advancement for nurses everywhere. With flashcards, videos, courses, organizational tools and more, we are singularly focused on helping students and nurses Level Up on their exams and nursing careers.
👋 STAY CONNECTED 👋
TikTok: https://tiktok.com/@leveluprn
Instagram: https://www.instagram.com/leveluprn/
Facebook: https://fb.me/LevelUpRN
Pinterest: https://www.pinterest.com/leveluprn/

Curettage, electrosurgery, and laser surgery are more likely than cryotherapy to leave scars, so they are usually reserved for hard-to-remove or recurring warts. If you have a large area of warts, curettage may not be an effective treatment. Some surgical treatments may be too painful for some children.

Cosmetic facial plastic surgery is surgery performed to enhance visual appearance of the facial structures and features. Common procedures include facelifts, eye lifts, rhinoplasty, chin and cheek implants, liposuction, and procedures to correct facial wrinkles.

The gastric balloon procedure (endoscopic intragastric balloon) leaves an inflated silicon balloon in the stomach for 6 months, making less room for food. As a result, patients: Feel full sooner while eating and therefore eat less. Lose about 30% of their excess weight in 6 months.
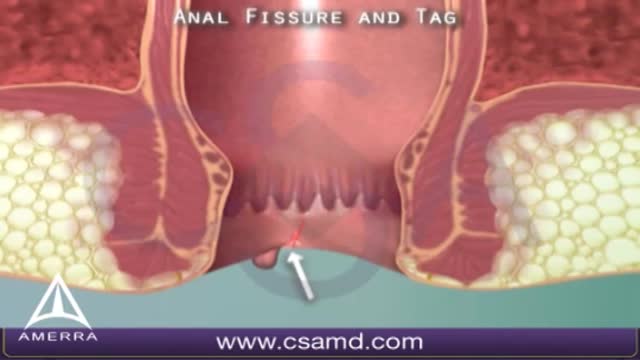
An anal fissure is a small tear in the thin, moist tissue (mucosa) that lines the anus. An anal fissure may occur when you pass hard or large stools during a bowel movement. Anal fissures typically cause pain and bleeding with bowel movements. You also may experience spasms in the ring of muscle at the end of your anus (anal sphincter). Anal fissures are very common in young infants but can affect people of any age. Most anal fissures get better with simple treatments, such as increased fiber intake or sitz baths. Some people with anal fissures may need medication or, occasionally, surgery.
Femoroacetabular impingement (FAI) is a condition in which extra bone grows along one or both of the bones that form the hip joint — giving the bones an irregular shape. Because they do not fit together perfectly, the bones rub against each other during movement. Over time this friction can damage the joint, causing pain and limiting activity.
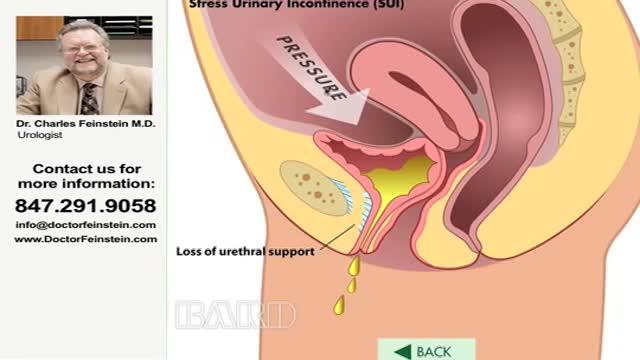
Urinary incontinence — the loss of bladder control — is a common and often embarrassing problem. The severity ranges from occasionally leaking urine when you cough or sneeze to having an urge to urinate that's so sudden and strong you don't get to a toilet in time. If urinary incontinence affects your daily activities, don't hesitate to see your doctor. For most people, simple lifestyle changes or medical treatment can ease discomfort or stop urinary incontinence

How to Use a Menstrual Cup Fold and hold. Always start by washing your hands. ... Insert and ensure. As with tampons, gently insert the folded cup into your vagina, tilting it back to the base of your spine. ... Use it up to twelve hours. ... Remove and empty. ... Re-insert.

This video: Pancreatic cancer begins in the tissues of your pancreas — an organ in your abdomen that lies horizontally behind the lower part of your stomach. Your pancreas secretes enzymes that aid digestion and hormones that help regulate the metabolism of sugars. Pancreatic cancer often has a poor prognosis, even when diagnosed early. Pancreatic cancer typically spreads rapidly and is seldom detected in its early stages, which is a major reason why it's a leading cause of cancer death. Signs and symptoms may not appear until pancreatic cancer is quite advanced and complete surgical removal isn't possible.
Thoracic outlet syndrome is a group of disorders that occur when blood vessels or nerves in the space between your collarbone and your first rib (thoracic outlet) are compressed. This can cause pain in your shoulders and neck and numbness in your fingers. Common causes of thoracic outlet syndrome include physical trauma from a car accident, repetitive injuries from job- or sports-related activities, certain anatomical defects (such as having an extra rib), and pregnancy. Sometimes doctors can't determine the cause of thoracic outlet syndrome. Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures. Most people improve with these approaches. In some cases, however, your doctor may recommend surgery.

Bariatric surgical procedures cause weight loss by restricting the amount of food the stomach can hold, causing malabsorption of nutrients, or by a combination of both gastric restriction and malabsorption. Bariatric procedures also often cause hormonal changes. Most weight loss surgeries today are performed using minimally invasive techniques (laparoscopic surgery). The most common bariatric surgery procedures are gastric bypass, sleeve gastrectomy, adjustable gastric band, and biliopancreatic diversion with duodenal switch. Each surgery has its own advantages and disadvantages.