Top videos

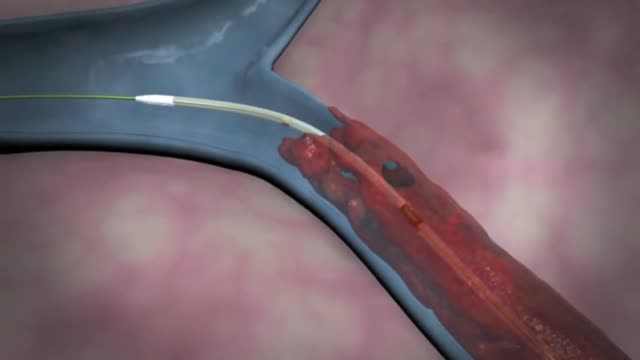
The removal of a clot is called an embolectomy. An embolectomy might be done during a surgery. Or it might be done with a minimally invasive procedure that uses a catheter (a thin tube that is guided through a blood vessel). This type of treatment for pulmonary embolism is used only in rare cases.
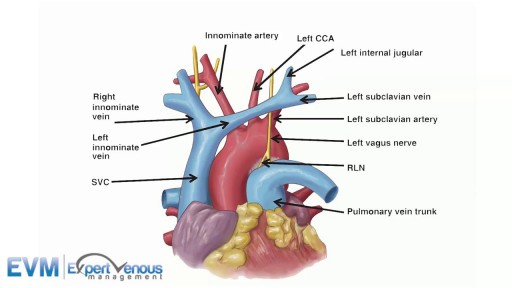
Although individual surgeons and centers employ different methods to insert a left ventricular assist device (LVAD), the fundamental concepts remain true for all. That is, most devices use the apex of the left ventricle (LV) as the inflow site to the pump, which subsequently gives off an outflow graft to the aorta, thus bypassing the ailing LV. Currently available devices do not differ significantly with regard to general implantation technique. The sequence of implantation can vary also from patient to patient, depending on the particular situation. In some cases, concomitant procedures may be performed in conjunction with LVAD implantation without adversely affecting outcome.

Bacterial meningitis is very serious and can be deadly. Death can occur in as little as a few hours. While most people with meningitis recover, permanent disabilities such as brain damage, hearing loss, and learning disabilities can result from the infection. There are several types of bacteria that can cause meningitis. Some of the leading causes of bacterial meningitis in the United States include Streptococcus pneumoniae, group B Streptococcus, Neisseria meningitidis, Haemophilus influenzae, and Listeria monocytogenes.

Hardware removals are among the most commonly performed surgical procedures worldwide. Current literature offers little data concerning postoperative patient satisfaction. The purpose of our study was to evaluate the patients’ point of view on implant removal. watch to learn more.

🔥 Multivitamins for Men: https://lynxshort.com/Multivitamins-for-Men
✨ Multivitamins for Women: https://lynxshort.com/Multivitamins-for-Women
⭐ Multivitamins for Kids: https://lynxshort.com/Multivitamins-for-Kids
📙 Book of the Day 📚 https://lynxshort.com/Book-of-the-Day
This is one of the most interesting medical topics to discuss. What are the responsibilities of a doctor? What are the basic skills a doctor needs to have? and what are the responsibilities of a doctor?
**** CONNECT ****
- " Medical Videos " Android application on Google Play store:
https://play.google.com/store/....apps/details?id=com.
https://healthusher.com
https://www.facebook.com/MedicalVideosAnimated
https://www.instagram.com/medical_videos1
👉 Support Us to Help Us Continue Making Videos.. Thanks in Advance :)
- Via PayPal: https://www.paypal.me/medicalvideos
- Via Patreon: https://www.patreon.com/medicalvideosanimated
- The creator:
Pharmacist. Alaa Nasr
#MedicalVideosAnimated
Affiliate Disclaimer: This video and description contains affiliate links, which means that if you click on one of the product links, I'll receive a small commission. This is at no extra cost to you and in many cases include exclusive discounts where applicable. This helps support the channel and allows me to continue to make free videos like this. Thank you for the support!

Among the many health benefits of sex are: Improved Immunity. People who have sex frequently (one or two times a week) have significantly higher levels of immunoglobulin A (IgA). ... Heart Health. ... Lower Blood Pressure. ... It's a Form of Exercise. ... Pain Relief. ... May Help Reduce Risk of Prostate Cancer. ... Improve Sleep. ... Stress Relief.

Epley maneuver: Step 1 You will sit on the doctor's exam table with your legs extended in front of you. The doctor will turn your head so that it is halfway between looking straight ahead and looking directly to the side that causes the worst vertigo. Without changing your head position, the doctor will guide you back quickly so that your shoulders are on the table but your head is hanging over the edge of the table. In this position, the side of your head that is causing the worst vertigo is facing the floor. The doctor will hold you in this position for 30 seconds or until your vertigo stops. Epley maneuver: Step 2 Then, without lifting up your head, the doctor will turn your head to look at the same angle to the opposite side, so that the other side of your head is now facing the floor. The doctor will hold you in this position for 30 seconds or until your vertigo stops. Epley maneuver: Step 3 The doctor will help you roll in the same direction you are facing so that you are now lying on your side. (For example, if you are looking to your right, you will roll onto your right side.) The side that causes the worst vertigo should be facing up. The doctor will hold you in this position for another 30 seconds or until your vertigo stops. Epley maneuver: Step 4 The doctor will then help you to sit back up with your legs hanging off the table on the same side that you were facing. This maneuver is done with the assistance of a doctor or physical therapist. A single 10- to 15-minute session usually is all that is needed. When your head is firmly moved into different positions, the crystal debris (canaliths) causing vertigo will move freely and no longer cause symptoms.

Ear Examination ENT is often a challenging examination, crossing over with the cranial nerve examination of the vestibular cochlear exam as well at other neurological assessments of balance
Here we will review the ear examination, looking both at the use of the otoscope, but also the Dix-Hallpike Manoeuvre, along with HINTS assessment. the Webers and Rinne's test is also included to determine types of hearing loss.
Often these ear examination techniques are performed separately, depending on the patients presenting complaint
#EARExamination #DrGill #ClinicalSkills
The future of Medicine - Il futuro della medicina - Die Zukunft der Medizin: High Tech, Robots, VR ⚡️Anatomia Biomeccanica Fisiologia by Ticinosthetics: tutto gira attorno alla palestra ©️2017 - www.ticinostheticsgs.com
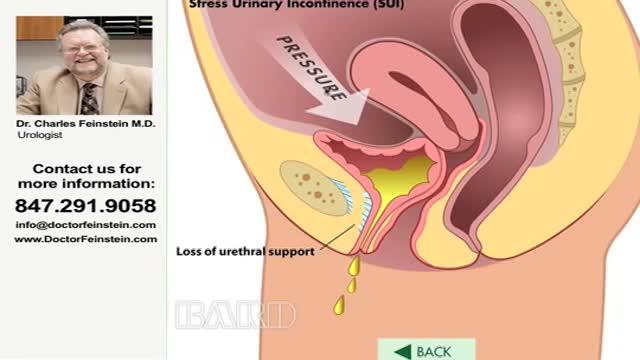
Urinary incontinence — the loss of bladder control — is a common and often embarrassing problem. The severity ranges from occasionally leaking urine when you cough or sneeze to having an urge to urinate that's so sudden and strong you don't get to a toilet in time. If urinary incontinence affects your daily activities, don't hesitate to see your doctor. For most people, simple lifestyle changes or medical treatment can ease discomfort or stop urinary incontinence

A cervical rib in humans is an extra rib which arises from the seventh cervical vertebra. Sometimes known as "neck ribs", their presence is a congenital abnormality located above the normal first rib. A cervical rib is estimated to occur in 0.2% (1 in 500 people) to 0.5% of the population.
Thoracic outlet syndrome is a group of disorders that occur when blood vessels or nerves in the space between your collarbone and your first rib (thoracic outlet) are compressed. This can cause pain in your shoulders and neck and numbness in your fingers. Common causes of thoracic outlet syndrome include physical trauma from a car accident, repetitive injuries from job- or sports-related activities, certain anatomical defects (such as having an extra rib), and pregnancy. Sometimes doctors can't determine the cause of thoracic outlet syndrome. Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures. Most people improve with these approaches. In some cases, however, your doctor may recommend surgery.

Possible causes are a blocked milk duct or bacteria entering the breast. It usually occurs within the first three months of breast-feeding. Symptoms include breast pain, swelling, warmth, fever, and chills. Antibiotics are required. Mild pain relievers can help with discomfort.