Top videos

Surgery to treat men with prostate cancer is often followed by months of difficulty controlling urine flow, a condition known as urinary incontinence. But new research suggests that this problem may go away more quickly if the men perform certain exercises to strengthen their pelvic floor muscles.
Researchers from the Kaiser Permanente Medical Center in Los Angeles, California, found that men who were taught how to perform pelvic floor exercises before and after surgery were more likely to have regained continence three months later.
Men Doing Pelvic Exercises Recover Earlier
In the current study, the researchers randomly assigned 38 men scheduled for radical prostatectomy to either a treatment group or a control group. The men in the treatment group were referred to a physical therapist. They were instructed how to do Pelvic Floor Exercises both before and after surgery, using biofeedback to ensure they were using the proper muscles. The control group did not receive any formal instruction. All of the men completed questionnaires regarding bladder function at regular intervals over the next year.
Overall, 82% of the patients had regained continence (defined as not needing to use any absorbent pads) by the end of the year, including about equal numbers in both groups. But on average the men who had been educated about Pelvic exercises regained continence about one month earlier than those in the control group (at 12 weeks vs. 16 weeks).
Most of the men who did not regain continence within a year were still using at least three absorbent pads a day, indicating continued severe incontinence. The study authors explained that these men probably had extensive damage to the bladder sphincter or severe dysfunction of the bladder after surgery, and the exercises alone were unable to compensate for this.
But the exercises seemed to be effective. Pelvic floor exercise and education initiated prior to surgery is an effective noninvasive intervention useful for improving early return of urinary continence, the authors concluded. It would certainly have a positive impact on our patients undergoing radical prostatectomy in an effort to improve quality of life after major urological surgery.
The results of the study were published in the Journal of Urology (Vol. 170, No. 1: 130-133)

This video - produced by students at Oxford University Medical School - demonstrates how to perform an examination of the respiratory system. It also indicates common pathologies encountered. It is part of a series of videos covering basic clinical examinations and is linked to Oxford Medical Education (www.oxfordmedicaleducation.com).

Candida Albicans is more than just yeast- for most people, it's already mutated into a more aggressive fungal form that eats holes through the intestinal tract causing many of todays health problems like food allergies, autoimmune disorders, Crohn's disease, IBS, low energy and many more aggressive diseases. People need to know what it is and what to do about it.
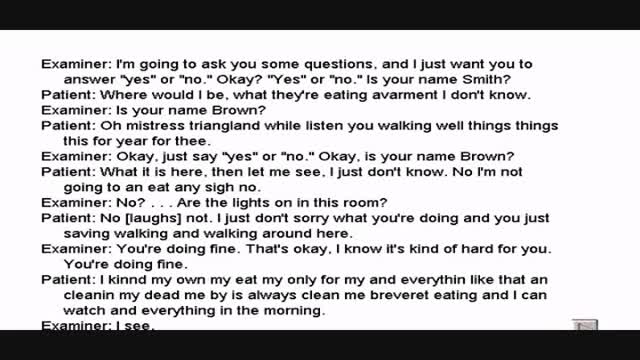
Wernicke's aphasia is a neurological disorder typically caused by stroke. It affects the Wernicke's region in the brain's left hemisphere which is reasoned to be responsible for processing of meaning, especially as it relates to verbal communication, hence the problems with speech witnessed in these patients

There are lots of fallacies about the missionary position being the best position for getting pregnant. With the woman on her back and her partner on top, it is thought that gravity will assist the sperm to swim upwards towards the egg.

Thoracentesis is a procedure used to obtain a sample of fluid from the space around the lungs. Normally, only a thin layer of fluid is present in the area between the lungs and chest wall. However, some conditions can cause a large amount of fluid to accumulate. This collection of fluid is called a pleural effusion.

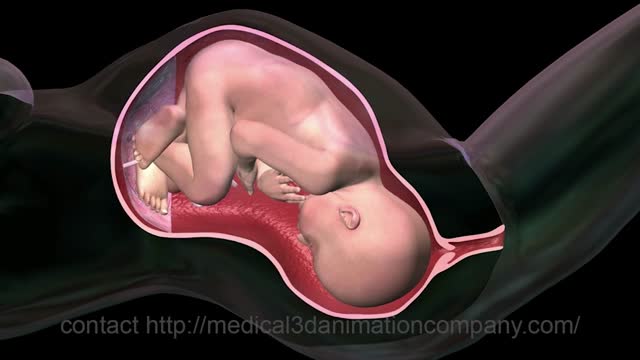
A breech birth occurs when a baby is born bottom first instead of head first. Around 3-5% of pregnant women at term (37–40 weeks pregnant) will have a breech baby. Most babies in the breech position are born by a caesarean section because it is seen as safer than being born vaginally.

Function and Anatomy: The hip is a ball and socket type joint, formed by the articulation of the head of the femur with the pelvis. Normal range of motion includes: abduction 45 degrees, adduction 20-30 degrees, flexion 135 degrees, extension 30 degrees, internal and external rotation. Hip pathology can cause symptoms anywhere around the joint, though frequently pain is anterior and radiates to the groin region. Additionally, pathology outside of the hip can be referred to this region. History and exam obviously help in making these distinctions.

A growing number of patients having total knee replacement surgery are 55 or younger. Surgeons at Sunnybrook's Holland Centre perform more than 1,000 total knee replacements each year. Read more: http://sunnyview.sunnybrook.ca..../2011/11/snap-crackl