Top videos

Comment Maigrir, Perdre Des Cuisses, Perdre Du Ventre Rapidement, Perdre 3 Kilos, Mincir Vite --- http://perte-poids-rapide.info-pro.co --- Comment maigrir uniquement du ventre ? Avoir un ventre gonflé et des bourrelets est le cauchemar des hommes comme des femmes. On n’est pas à l’aise dans son corps, on a du mal à s’habiller et dès que l’on fait un repas copieux, il faut déboutonner son pantalon. Alors quelles sont les solutions pour maigrir du ventre ? Changez vos habitudes alimentaires Maigrir uniquement du ventre est compliqué comme pour toutes les autres parties du corps. On ne peut pas maigrir qu’au niveau du ventre ou qu’au niveau des cuisses ou des fesses d’ailleurs. Si vous pensez qu’il est suffisant de faire des heures d’abdos pour retrouver un ventre plat, c’est une erreur. Il faut d’abord perdre la graisse avant d’attaquer le sport. Et pour cela, il va falloir passer par la case régime. Inutile de vous ruer sur le dernier régime à la mode qui vous promet de perdre 5 kilos dès que vous mangerez normalement. Pour perdre du poids au niveau de la ceinture abdominale sur du long terme, choisissez plutôt une méthode où vous apprendrez les bonnes habitudes alimentaires avec une alimentation saine et équilibrée. Pour cela, il va falloir : Stopper les grignotages Ne pas sauter de repas Mâcher lentement les aliments Supprimer l’alcool et les jus de fruit achetés en magasin Faire une croix sur les fast-foods et les plats industriels Tirer un trait sur les gâteaux, les viennoiseries, les fritures et les sauces Consommer des fruits et des légumes Mangez de la viande blanche, des œufs et du poisson Préférer le pain complet à la baguette traditionnelle Inclure des féculents à chaque repas Boire 1,5 litre d’eau par jour Découvrez Comment Mincir Durablement Sans Peser Les Aliments Ni Compter Les Calories... Cliquez ici: http://perte-poids-rapide.info-pro.co
Genetic surfactant dysfunction disorders are caused by mutations in genes encoding proteins critical for the production and function of pulmonary surfactant. These rare disorders may produce familial or sporadic lung disease, with clinical presentations ranging from neonatal respiratory failure to childhood- or adult-onset interstitial lung disease. An overview of these disorders is presented in the table.. Interstitial lung diseases in children until recently were categorized by their histologic appearance in a manner similar to that used for adult forms of interstitial lung disease (ILD). In children, the lung histopathology findings associated with desquamative interstitial pneumonitis (DIP) are now known to often result from genetic mechanisms that disrupt normal surfactant production and metabolism. By contrast, DIP in adults is considered to represent a distinct type of ILD, which is strongly associated with cigarette smoking and carries a relatively favorable prognosis [1]. These genetic disorders also result in histopathologic patterns other than DIP, including findings of pulmonary alveolar proteinosis and chronic pneumonitis of infancy. An understanding of the pathogenesis of these disorders permits a mechanistic classification as genetic surfactant dysfunction disorders instead of their previous classification based upon histologic appearance.
Verrugas Genitales, Verrugas Del Papiloma Humano, Verrugas En El Cuerpo, Como Eliminar Lunares -- http://sinverrugasylunares.plus101.com --- El Nitrógeno Liquido Es Seguro Para Eliminas Tus Verrugas? Dentro de los tratamientos para las verrugas que la medicina convencional ofrece existe la crioterapia el cual se utiliza nitrógeno líquido. Este tratamiento es de los más comunes que se utilizan para remover las verrugas, este tratamiento debe ser administrado por un profesional especializado. Ya que si se hace sin la supervisión adecuada puede provocar severos daños en la piel. El tratamiento se aplica de la forma siguiente: Se aplica sobre la verruga un poco de nitrógeno líquido ya sea en aerosol o con un algodón, teniendo cuidado de no aplicar a áreas sanas de la piel, esto debido a que el nitrógeno líquido puede afectar severamente a la piel sana, es por eso que debe ser aplicado por un profesional. Para eliminar la verruga serán necesarias varias aplicaciones, al cabo de 2 a 3 semanas la verruga se caerá dejando una costra sobre la piel. Las molestias sobre este tratamiento depende mucho del especialista que lo aplique, existen casos en que a sido doloroso porque el médico a rociado nitrógeno líquido en las partes alrededor de la verruga, lo cual produce un severo daño a la piel, eso sin contar la costra que se forma en la parte donde estuvo la verruga después de que esta se cayera. Generalmente el dolor es mínimo pero también se tiene la opción de aplicar anestesia local sobre la parte afectada. Tu sistema inmunológico es un arma poderosa contra todas las infecciones que existen, pero lamentablemente no le damos el debido mantenimiento q ue necesita para poder luchar contra las infecciones virales. Te invito a conocer esta guía aquí: http://sinverrugasylunares.plus101.com
Transvenous cardiac pace maker, also called endocardial pacing, is a potentially life saving intervention used primarily to correct profound bradycardia. It can be used to treat symptomatic bradycardias that do not respond to transcutaneous pacing or to drug therapy.

The gastric balloon procedure (endoscopic intragastric balloon) leaves an inflated silicon balloon in the stomach for 6 months, making less room for food. As a result, patients: Feel full sooner while eating and therefore eat less. Lose about 30% of their excess weight in 6 months.

Your stomach must be empty, so you should not eat or drink anything for approximately 8 hours before the examination. Your physician will be more specific about the time to begin fasting depending on the time of day that your test is scheduled. Your current medications may need to be adjusted or avoided. Most medications can be continued as usual. Medication use such as aspirin, Vitamin E, non-steroidal anti-inflammatories, blood thinners and insulin should be discussed with your physician prior to the examination as well as any other medication you might be taking. It is therefore best to inform your physician of any allergies to medications, iodine, or shellfish. It is essential that you alert your physician if you require antibiotics prior to undergoing dental procedures, since you may also require antibiotics prior to ERCP. Also, if you have any major diseases, such as heart or lung disease that may require special attention during the procedure, discuss this with your physician. To make the examination comfortable, you will be sedated during the procedure, and, therefore, you will need someone to drive you home afterward. Sedatives will affect your judgment and reflexes for the rest of the day, so you should not drive or operate machinery until the next day.

Thoracic outlet syndrome is a group of disorders that occur when blood vessels or nerves in the space between your collarbone and your first rib (thoracic outlet) are compressed. This can cause pain in your shoulders and neck and numbness in your fingers. Common causes of thoracic outlet syndrome include physical trauma from a car accident, repetitive injuries from job- or sports-related activities, certain anatomical defects (such as having an extra rib), and pregnancy. Sometimes doctors can't determine the cause of thoracic outlet syndrome. Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures. Most people improve with these approaches. In some cases, however, your doctor may recommend surgery.
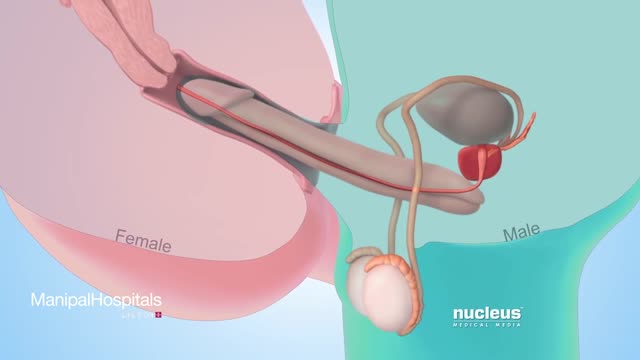
In some cases, the doctor will recommend that the couple seek assisted reproductive technologies (ART), such as IVF (in vitro fertilisation). ART do not cure or treat the cause of infertility but they can help couples achieve a pregnancy, even if the man's sperm count is very low.
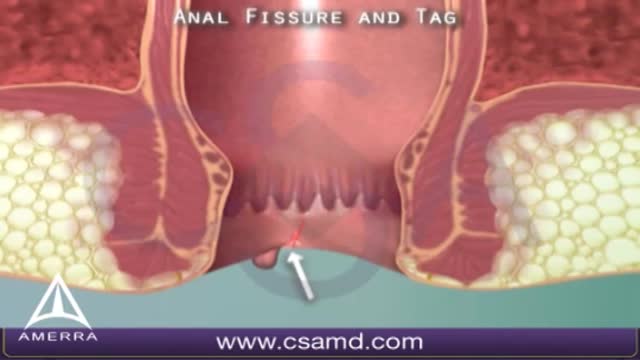
An anal fissure is a small tear in the thin, moist tissue (mucosa) that lines the anus. An anal fissure may occur when you pass hard or large stools during a bowel movement. Anal fissures typically cause pain and bleeding with bowel movements. You also may experience spasms in the ring of muscle at the end of your anus (anal sphincter). Anal fissures are very common in young infants but can affect people of any age. Most anal fissures get better with simple treatments, such as increased fiber intake or sitz baths. Some people with anal fissures may need medication or, occasionally, surgery.
Cholangitis Email this page to a friend Email this page to a friend Facebook Twitter Google+ Cholangitis is an infection of the bile ducts, the tubes that carry bile from the liver to the gallbladder and intestines. Bile is a liquid made by the liver that helps digest food. Causes Cholangitis is most often caused by bacteria. This can occur when the duct is blocked by something, such as a gallstone or tumor. The infection causing this condition may also spread to the liver. Risk factors include a previous history of gallstones, sclerosing cholangitis, HIV, narrowing of the common bile duct, and rarely, travel to countries where you might catch a worm or parasite infection. Symptoms The following symptoms may occur: Pain on the upper right side or upper middle part of the abdomen. It may also be felt in the back or below the right shoulder blade. The pain may come and go and feel sharp, cramp-like, or dull. Fever and chills. Dark urine and clay-colored stools. Nausea and vomiting. Yellowing of the skin (jaundice), which may come and go.

Hysteroscopy is a procedure that allows your doctor to look inside your uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
Before deciding how to treat one episode of high blood glucose, it is important to figure out why the number is high. Some possible causes include eating a heavy meal, not getting enough physical activity, forgetting to take diabetes medication, and dealing with illness and stress. Insulin is the medication that will bring blood glucose down the fastest. Someone who uses mealtime insulin can take correction doses to lower blood glucose. This requires a thorough understanding of when to inject, how often to give correction doses, and how much insulin to use. You will need to work with your doctor or diabetes educator to learn how to do this. Apart from administering insulin, the fastest way to lower your blood glucose is to engage in physical activity. Exercise results in an increased sensitivity to insulin. It causes your muscle cells to take up more glucose, leaving less of it to circulate in your bloodstream during and after the physical activity (which means a lower blood glucose when you test). Frequent, regular exercise is very important to good blood glucose control no matter what type of diabetes you have. Research has shown that it is vital in warding off long-term complications like neuropathy, retinopathy, and heart and kidney diseases. Don't forget to check with a doctor, though, before making any major changes to your exercise routine. And, if you have type 1 diabetes and your glucose is 250 mg/dl or higher, check for urine ketones. You should not exercise if ketones are present.
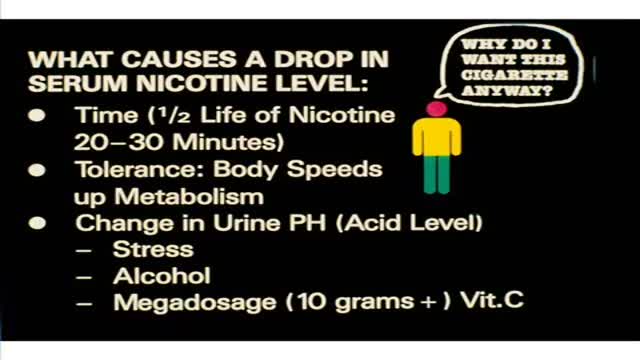
Most people start smoking when they are in their teens and are addicted by the time they reach adulthood. Some have tried to quit but have returned to cigarettes because smoking is such a strong addiction. It is a habit that is very difficult to break. There are many different reasons why people smoke.