Top videos

The easy experimental answer to this question is 264 hours (about 11 days). In 1965, Randy Gardner, a 17-year-old high school student, set this apparent world-record for a science fair. Several other normal research subjects have remained awake for eight to 10 days in carefully monitored experiments. None of these individuals experienced serious medical, neurological, physiological or psychiatric problems. On the other hand, all of them showed progressive and significant deficits in concentration, motivation, perception and other higher mental processes as the duration of sleep deprivation increased. Nevertheless, all experimental subjects recovered to relative normality within one or two nights of recovery sleep. Other anecdotal reports describe soldiers staying awake for four days in battle, or unmedicated patients with mania going without sleep for three to four days.

Instead, try these natural solutions and lifestyle changes, which may help you stop snoring. Change Your Sleep Position. ... Lose Weight. ... Avoid Alcohol. ... Practice Good Sleep Hygiene. ... Open Nasal Passages. ... Change Your Pillows. ... Stay Well Hydrated.

Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. You may have sleep apnea if you snore loudly, and you feel tired even after a full night's sleep. The main types of sleep apnea are: Obstructive sleep apnea, the more common form that occurs when throat muscles relax. Central sleep apnea, which occurs when your brain doesn't send proper signals to the muscles that control breathing. Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea. If you think you might have any form of sleep apnea, see your doctor. Treatment can ease your symptoms and may help prevent heart problems and other complications.

The Ortolani method is an examination method that identifies a dislocated hip that can be reduced into the socket (acetabulum). Ortolani described the feeling of reduction as a “Hip Click” but the translation from Italian was interpreted a sound instead of a sensation of the hip moving over the edge of the socket when it re-located. After the age of six weeks, this sensation is rarely detectable and should not be confused with snapping that is common and can occur in stable hips when ligaments in and around the hip create clicking noises. When the Ortolani test is positive because the hip is dislocated, treatment is recommended to keep the hip in the socket until stability has been established
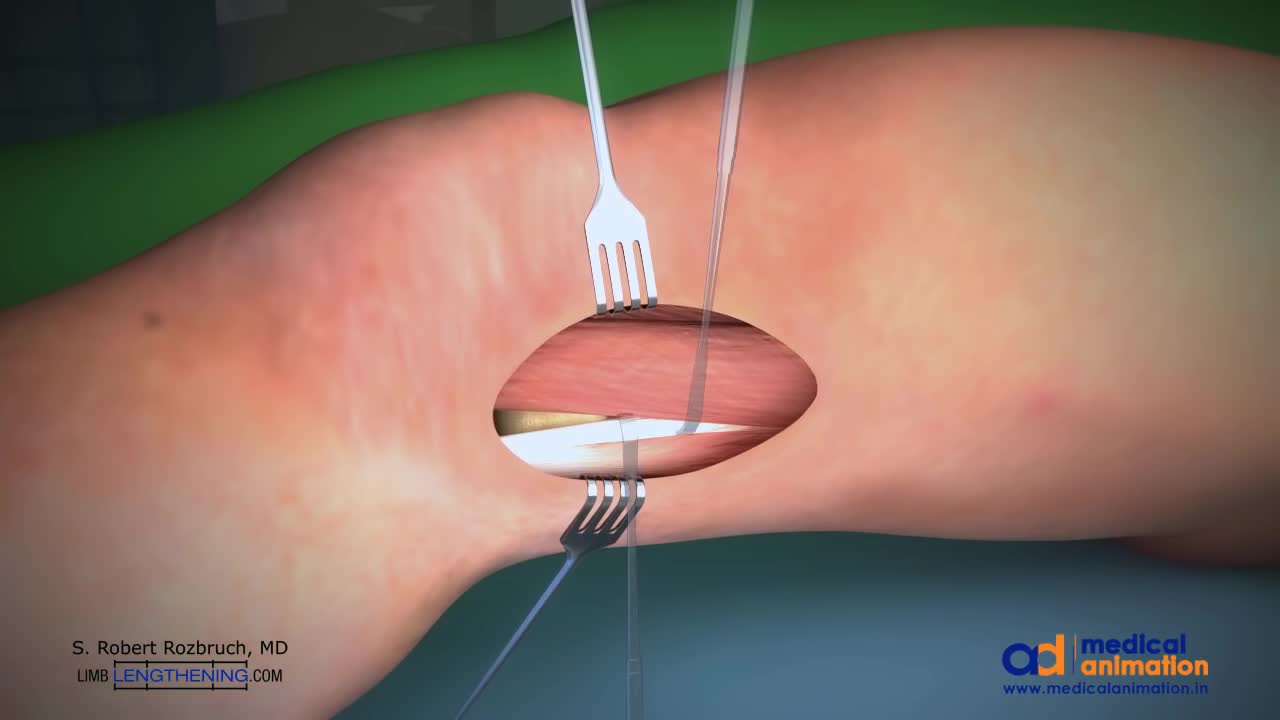
The Distal Femoral Osteotomy System utilizes the same principles of design featured in the Tibial Osteotomy System. Specifically designed femoral osteotomy plates take into account the anatomical differences between the distal femur and proximal tibia.

Jennifer Lawton, M.D., is professor and chief of the Johns Hopkins Division of Cardiac Surgery, as well as director of the Cardiac Surgery Research Laboratory and program director of the cardiothoracic fellowship training program at Johns Hopkins. Her areas of expertise include valve surgery, including minimally invasive surgery, coronary artery bypass grafting on- and off-pump, all arterial revascularization, as well as surgery for aortic dissection and ascending aneurysm. For more information about Dr. Lawton visit http://www.hopkinsmedicine.org..../heart_vascular_inst

Peritoneal dialysis (per-ih-toe-NEE-ul die-AL-uh-sis) is a way to remove waste products from your blood when your kidneys can no longer do the job adequately. A cleansing fluid flows through a tube (catheter) into part of your abdomen and filters waste products from your blood. After a prescribed period of time, the fluid with filtered waste products flows out of your abdomen and is discarded. Peritoneal dialysis differs from hemodialysis, a more commonly used blood-filtering procedure. With peritoneal dialysis, you can give yourself treatments at home, at work or while traveling. Peritoneal dialysis isn't an option for everyone wit

Know About Cardiothoracic Surgery in 60 Seconds About what cardiothoracic surgery is, why it is done and what is the result of such surgery. A Major Session on #cardiothoracic #surgery at #Congress #2018HCC 2018 Healthcare and Cardiology Conference #BANGKOK http://cosmicseries.org/cardiology-conferences/