Top videos

• Define and use related medical terminology.
• Describe and demonstrate techniques for imaging the thyroid gland.
• Discuss functional abnormalities of the thyroid gland.
• Correlate laboratory data relevant to the thyroid and parathyroid glands.
• Describe, and recognize on images, pathologies of the thyroid gland.
• Identify the anatomy of the parathyroid glands on diagrams and sonograms.
• Describe and demonstrate techniques for imaging the parathyroid glands.
• Describe, and recognize on images, pathologies of the parathyroid glands.
• List and describe other neck masses.
• Follow relevant protocols when scanning.
• Differentiate the sonographic appearances of the female reproductive organs in relation to the menstrual cycle, the use of contraceptives and hormone replacement, and following chemotherapy.
• Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).

The Combitube is a twin lumen device designed for use in emergency situations and difficult airways. It can be inserted without the need for visualization into the oropharynx, and usually enters the esophagus. It has a low volume inflatable distal cuff and a much larger proximal cuff designed to occlude the oro- and nasopharynx.
If the tube has entered the trachea, ventilation is achieved through the distal lumen as with a standard ETT. More commonly the device enters the esophagus and ventilation is achieved through multiple proximal apertures situated above the distal cuff. In the latter case the proximal and distal cuffs have to be inflated to prevent air from escaping through the esophagus or back out of the oro- and nasopharynx.
For patients looking to slim down their neck and achieve a more contoured and sculpted jaw line, then Tampa chin liposuction at the Artistic Lipo Sculpting Center is the answer! This one procedure can literally make patients look 10 years younger and 20 lbs lighter. Dr. Thomas Su is specialized in performing Liposuction procedures and consistently achieves stunning results for his Tampa patients. To find out more about Tampa neck lipo, visit http://www.artlipo.com/liposuction/liposuction-body-areas/lipo-chin---neck.html
Key facts
Hepatitis B is a viral infection that attacks the liver and can cause both acute and chronic disease.
The virus is transmitted through contact with the blood or other body fluids of an infected person - not through casual contact.
About 2 billion people worldwide have been infected with the virus and about 350 million live with chronic infection. An estimated 600 000 persons die each year due to the acute or chronic consequences of hepatitis B.
About 25% of adults who become chronically infected during childhood later die from liver cancer or cirrhosis (scarring of the liver) caused by the chronic infection.
The hepatitis B virus is 50 to 100 times more infectious than HIV.
Hepatitis B virus is an important occupational hazard for health workers.
Hepatitis B is preventable with a safe and effective vaccine.
-----------------------------------
Hepatitis B is a potentially life-threatening liver infection caused by the hepatitis B virus. It is a major global health problem and the most serious type of viral hepatitis. It can cause chronic liver disease and puts people at high risk of death from cirrhosis of the liver and liver cancer.
Worldwide, an estimated two billion people have been infected with the hepatitis B virus (HBV), and more than 350 million have chronic (long-term) liver infections.
A vaccine against hepatitis B has been available since 1982. Hepatitis B vaccine is 95% effective in preventing HBV infection and its chronic consequences, and is the first vaccine against a major human cancer.
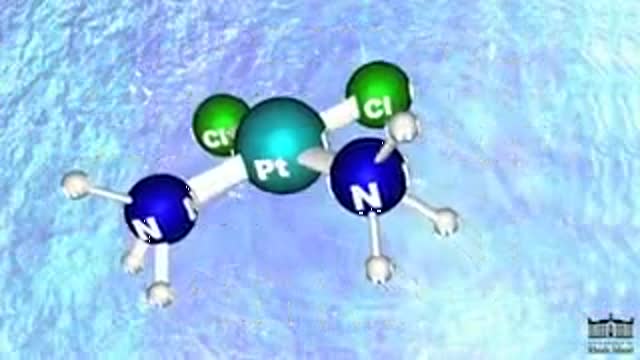
Cisplatin is in a class of drugs known as platinum-containing compounds used to treat various types of cancers including metastatic testicular and ovarian tumors. The molecule was first discovered in 1845, but did not receive FDA approval until 1978. Today it is known as the "penicillin of cancer drugs," because it is so effective for many different cancers. There are three key players involved in Cisplatin's mechanism: (1) Cisplatin, (2) DNA (3) and an HMG Protein. Most Cisplatin enters the body through active transport, but some molecules are passively defused through the cell membrane. Once in the nucleus, Cisplatin can form an adduct with two consecutive guanine bases within a strand of DNA. The molecule loses its chlorine atoms in exchange for the nitrogen atoms of the target guanines. Cisplatin can bond more tightly with nitrogen because nitrogen balances the platinum charge more effectively than chlorine. It is this adduct-induced DNA bend that allows binding of proteins which contain the high mobility group, HMG domain. Once the protein is bound to the DNA, it inserts a wedge-like phenyl group of phenylalanine 37 into the widened minor groove created by the bend. The tightly bound HMG protein causes destacking of the nucleotide bases, resulting in the DNA helix becoming kinked. In this way, Cisplatin can be thought of as a monkey wrench in the DNA repair system. With the HMG protein bound to the DNA, the modified strand is not repaired properly and so the cell dies. The success of Cisplatin depends on its ratio of efficacy between cancerous and healthy cells.
Tampa body sculpting is the specialty of Dr. Thomas Su of the Artistic Lipo Sculpting Center. Dr. Su’s dedication to body contouring has allowed him to finely hone his craft over the years, making him the most trusted Tampa lipo surgeon. To learn more about Tampa fat removal procedures, visit http://www.artlipo.com/liposuction/liposuction-body-areas/lipo-abdomen.html.

http://www.mediplus.co.uk A new and safer method of inserting a Foley catheter suprapubically. The technique allows the insertion to be carried out in an Outpatient setting, thus saving time, cost and effort. By using the Seldinger technique, the product reduces the chances of bowel or bladder perforation and resultant morbidity.
The product has been chosen by The NHS National Technology Adoption Centre to help facilitate adoption of the product.