Top videos

Superior vena cava syndrome (SVCS) is obstruction of blood flow through the superior vena cava (SVC). It is a medical emergency and most often manifests in patients with a malignant disease process within the thorax. A patient with SVCS requires immediate diagnostic evaluation and therapy.
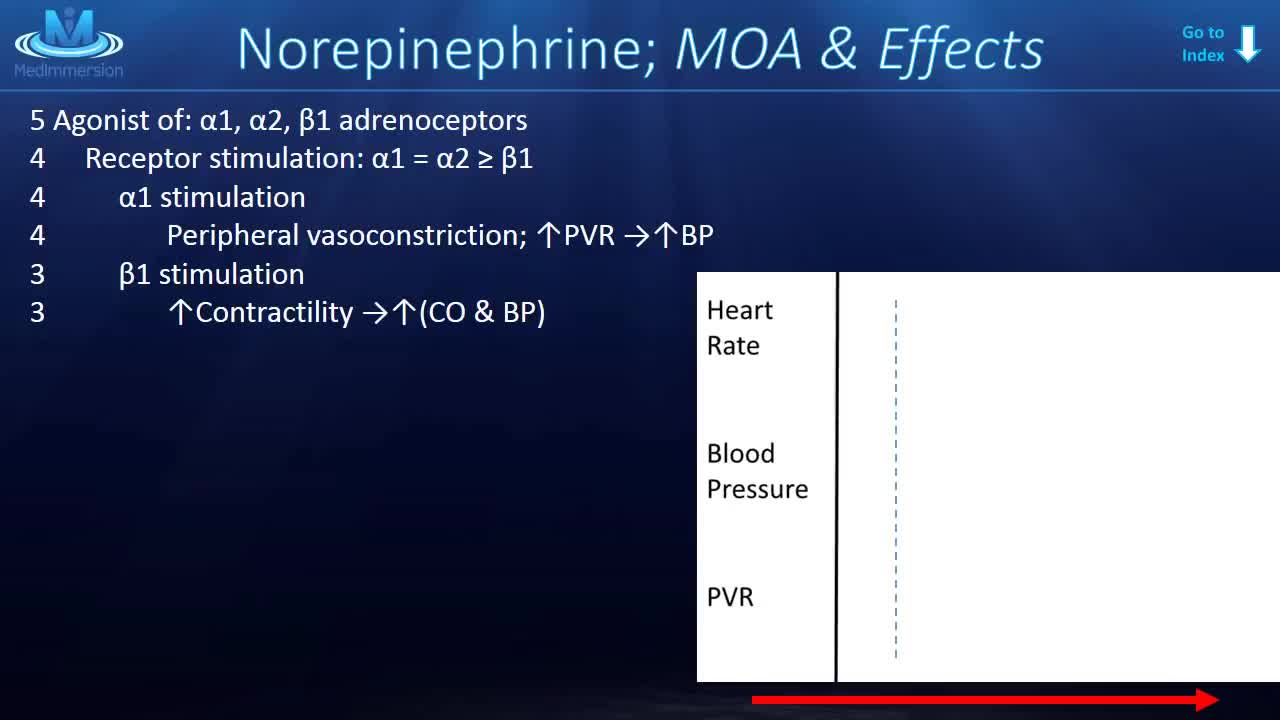
Norepinephrine is synthesized from dopamine by dopamine β-hydroxylase.[7] It is released from the adrenal medulla into the blood as a hormone, and is also a neurotransmitter in the central nervous system and sympathetic nervous system where it is released from noradrenergic neurons.
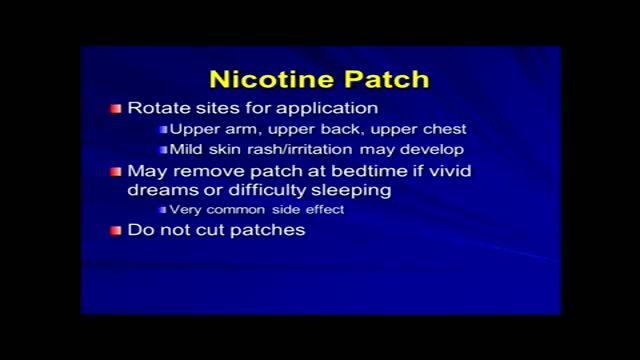
Tobacco use is the most common preventable cause of death. About half of the people who don't quit smoking will die of smoking-related problems. Quitting smoking is important for your health. Soon after you quit, your circulation begins to improve, and your blood pressure starts to return to normal. Your sense of smell and taste return, and it's easier for you to breathe. In the long term, giving up tobacco can help you live longer. Your risk of getting cancer decreases with each year you stay smoke-free. Quitting is not easy. You may have short-term affects such as weight gain, irritability, and anxiety. Some people try several times before they succeed. There are many ways to quit smoking. Some people stop "cold turkey." Others benefit from step-by-step manuals, counseling, or medicines or products that help reduce nicotine addiction. Some people think that switching to e-cigarettes can help you quit smoking, but that has not been proven. Your health care provider can help you find the best way for you to quit.

Knee replacement surgery advances are improving patients' experiences and outcomes. Knee surgery -- or even partial knee replacement -- is often the solution for advanced knee arthritis. Today you can regain significant mobility and flexibility after knee replacement thanks to advances in orthopedic surgery technology, materials and techniques. Knee replacement recovery times also have improved. This knee replacement surgery video covers what you can expect out of these knee joint replacement advances. Knee replacement surgery has been around for more than 30 years and is an incredibly successful operation. In the past the past, when a person had bad arthritis of the knee, they were pretty much out of luck other than taking aspirin. They'd be debilitated and limited in their activities. So, when a person has pain, stiffness, and their life is becoming restricted by that, that's when it's time to consider knee replacement. We always do non-surgical treatment first. When that doesn't work anymore, then it's time to consider knee replacement. About 500,000 a year are done, and most patients who have gone through this basically say that they wish they had done it sooner.

During root canal treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterwards, the tooth is restored with a crown or filling for protection.
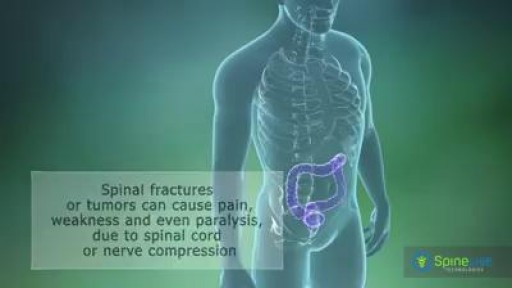
A spinal tumor is a growth that develops within your spinal canal or within the bones of your spine. It may be cancerous or noncancerous. Tumors that affect the bones of the spine (vertebrae) are known as vertebral tumors. Tumors that begin within the spinal cord itself are called spinal cord tumors. There are two main types of tumors that may affect the spinal cord: Intramedullary tumors begin in the cells within the spinal cord itself, such as astrocytomas or ependymomas. Extramedullary tumors develop within the supporting network of cells around the spinal cord. Although they don't begin within the spinal cord itself, these types of tumors may affect spinal cord function by causing spinal cord compression and other problems. Examples of extramedullary tumors that can affect the spinal cord include schwannomas, meningiomas and neurofibromas.

Take your left leg and place your ankle against the knee. Hold the position for a moment before changing legs. This helps stretch the tiny piriformis muscle, which sometimes becomes inflamed and presses against the sciatic nerve causing pain. Repeat by switching sides and doing the same exercise with the other leg.

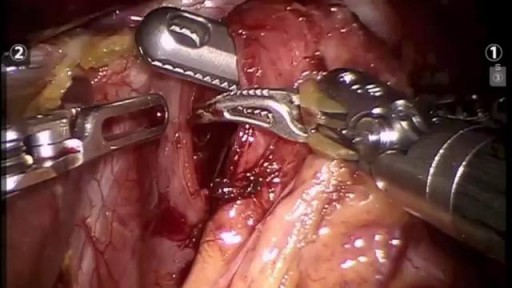
Indications for endovascular repair of the iliac artery are: Stenosis or (short-segment) occlusion of iliac artery (TASC type A and B, TASC C lesions are controversial) with ipsilateral lower extremity ischemia (lifestyle-limiting, progressive claudication, rest pain, gangrene). Patients with asymptomatic aneurysm greater than 4 cm in diameter. An iliac aneurysm which has also increased in size by 0.5 cm in last six months. Symptomatic iliac artery aneurysms mandate endovascular (or open) repair regardless of size. Patients with long occluded lesions/poor run-off/acute limb ischemia are poor endovascular candidates.

Dr. Kathryn Baerman is a Board Certified General Surgeon specializing in Women's Health and Breast Care. She shares with us that in women, hernias present differently than in men. If you are experiencing groin pain, it may be a hernia.
To visit Dr. Baerman in Apex, Chapel Hill, or Durham, North Carolina, call 919-281-1699 to schedule an appointment with her at EmergeOrtho.

Lipomas are slow-growing soft tissue tumours that rarely reach a size larger than 2 cm. Lesions larger than 5 cm, so-called giant lipomas, can occur anywhere in the body but are seldom found in the upper extremities. The authors present their experiences with eight patients having giant lipomas of the upper extremity. In addition, a review of the literature, and a discussion of the appropriate evaluation and management are included.
This video: The veins around your anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from an increase in pressure in the lower rectum. Factors that might cause increased pressure include: Straining during bowel movements.

Try our MULTIPLE CHOICE QUESTIONS and WATCH MORE VIDEOS at www.boxmedicine.com!
Inguinal and femoral hernias need not be confusing. In this tutorial you will be presented with colourful diagrams and animations to cover important areas, such as the anatomy of what goes on in these two conditions, the examination of groin hernias and a simple explanation of the difference between incarceration, strangulation and obstruction, in and amongst a systematic look at the clinical topic. More tutorials at www.boxmedicine.com.
Comment Avoir Un Ventre Plat, Rajeuni, Rajeunir De 10 Ans En 3 Mois, Bruleur De Graisse Musculation --- http://rajeunir-de-10-ans.info-pro.co --- 5 Raisons pourquoi le Cardio Long-Lent n’est PAS bon. En passant à travers les e-mails de clients au cours des derniers jours, j'ai remarqué que beaucoup de gens font encore du cardio longue durée, à faible intensité, beurk! Voici l'affaire: si vous cherchez à obtenir un bénéfice maximal du temps que vous mettez dans vos séances d'entraînement, le cardio de longue durée à faible intensité n'est pas la voie à suivre, et pour de nombreuses raisons. Voici mon top 5: 1. Les calories brûlées minimales: 45 minutes sur le tapis roulant peuvent brûler un énorme 300 calories si vous êtes chanceux, l'équivalent de 50 grammes de graisse. En vous exerçant dix heures par semaine et vous pourriez perdre un demi-kilo! Ce qui m'amène à mon prochain point: 2. Beaucoup trop de temps consacré: Je ne sais pas pour vous, mais je n'ai pas des heures et des heures de mon temps à mettre dans l’entraînement chaque semaine. En fait, je n’ai le temps pour faire que quelques heures d'exercice par semaine, et vous savez quoi? C'est tout ce dont vous avez besoin. En fait, la recherche a montré que plus de 90 minutes par semaine peuvent être nuisibles! (Plus d'infos ici) http://rajeunir-de-10-ans.info-pro.co Au-delà de cela, le cardio à longue durée et faible intensité est: 3. Ennuyeux que diable: Assis sur un vélo d'exercice à regarder le mur en face de moi pendant 45-60 minutes? Non merci. Mais peut-être pire encore est le fait que le cardio de longue durée et à faible intensité ne fournit: Ces 5 étapes Révèlent Les Choses Que Vous Devez ABSOLUMENT ÉVITER Si Vous Voulez Ralentir Le Processus De Vieillissement, Récupérer Votre Santé Et Atteindre Un Corps Idéal. Cliquez Ici: http://rajeunir-de-10-ans.info-pro.co