Top videos

Ewing's sarcoma typically occurs in children and young adults. It often begins in the legs, bones of the pelvis, and arms. Bone pain, localized swelling, and tenderness are symptoms. In rare cases bone fractures may also be found. Treatments include chemotherapy, surgery, and radiation.

Cobalamin (vitamin B12) deficiency is particularly common in the elderly (>65 years of age), but is often unrecognized because of its subtle clinical manifestations; although they can be potentially serious, particularly from a neuropsychiatric and hematological perspective.
Multiple myeloma is a cancer formed by malignant plasma cells. Normal plasma cells are found in the bone marrow and are an important part of the immune system. The immune system is made up of several types of cells that work together to fight infections and other diseases. Lymphocytes (lymph cells) are the main cell type of the immune system. The major types of lymphocytes are T cells and B cells.

Pyogenic granuloma (lobular capillary hemangioma[1] ) is a relatively common benign vascular lesion of the skin and mucosa whose exact cause is unknown. Also see the Medscape Reference article Oral Pyogenic Granuloma. Pyogenic granulomas are misnamed; they are neither infectious nor granulomatous. The lesion usually occurs in children and young adults as a solitary, glistening red papule or nodule that is prone to bleeding and ulceration. Pyogenic granulomas typically evolve rapidly over a period of a few weeks, most often on the head, neck, extremities, and upper trunk. Pyogenic granuloma often arises in pregnancy (or rarely with oral contraceptive usage), particularly on the gingiva or elsewhere in the oral mucosa, and then is termed the "pregnancy tumor." Other pyogenic granuloma variants that have been well documented include the disseminated, subcutaneous, intravenous, and medication-induced (for example, retinoid, antiretroviral, and oncologic agent) subtypes. Removal of pyogenic granuloma is indicated to alleviate any bleeding, discomfort, cosmetic distress, and diagnostic uncertainty. A number of malignant tumors may clinically mimic pyogenic granuloma, making histopathologic confirmation important if the presentation is atypical. Aside from cutaneous and oral lesions, pyogenic granuloma has been reported throughout the gastrointestinal tract and upper airway, at various ocular locations, the central nervous system, the bladder, and the internal vasculature. This article discusses only cutaneous and oral involvement.
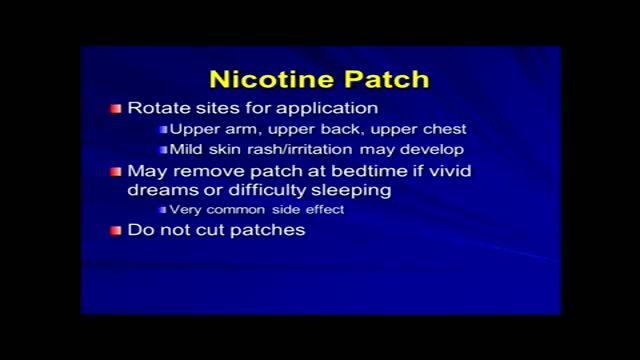
Tobacco use is the most common preventable cause of death. About half of the people who don't quit smoking will die of smoking-related problems. Quitting smoking is important for your health. Soon after you quit, your circulation begins to improve, and your blood pressure starts to return to normal. Your sense of smell and taste return, and it's easier for you to breathe. In the long term, giving up tobacco can help you live longer. Your risk of getting cancer decreases with each year you stay smoke-free. Quitting is not easy. You may have short-term affects such as weight gain, irritability, and anxiety. Some people try several times before they succeed. There are many ways to quit smoking. Some people stop "cold turkey." Others benefit from step-by-step manuals, counseling, or medicines or products that help reduce nicotine addiction. Some people think that switching to e-cigarettes can help you quit smoking, but that has not been proven. Your health care provider can help you find the best way for you to quit.
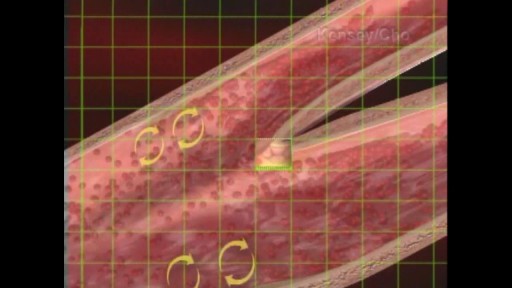
When the hematocrit rises to 60 or 70%, which it often does in polycythemia, the blood viscosity can become as great as 10 times that of water, and its flow through blood vessels is greatly retarded because of increased resistance to flow. This will lead to decreased oxygen delivery.

Skin grafting is a type of medical grafting involving the transplantation of skin. The transplanted tissue is called a skin graft. Skin grafting is often used to treat: Extensive wounding or trauma Burns Areas of extensive skin loss due to infection such as necrotizing fasciitis or purpura fulminans Specific surgeries that may require skin grafts for healing to occur – most commonly removal of skin cancers. Skin grafts are often employed after serious injuries when some of the body’s skin is damaged. Surgical removal (excision or debridement) of the damaged skin is followed by skin grafting. The grafting serves two purposes: it can reduce the course of treatment needed (and time in the hospital), and it can improve the function and appearance of the area of the body which receives the skin graft. There are two types of skin grafts, the more common type is where a thin layer is removed from a healthy part of the body (the donor section), like peeling a potato, or a full thickness skin graft, which involves pitching and cutting skin away from the donor section. A full thickness skin graft is more risky, in terms of the body accepting the skin, yet it leaves only a scar line on the donor section, similar to a Cesarean section scar. For full thickness skin grafts, the donor section will often heal much more quickly than the injury and is less painful than a partial thickness skin graft.

A simple test of fingernail clippings could replace a blood draw as a way to diagnose and monitor type 2 diabetes mellitus (T2DM), with huge implications for tracking the disease in the developing world. Research on this method by a team of Belgian researchers was reported July 28, 2015, at the 2015 American Association for Clinical Chemistry (AACC) Annual Meeting and Clinical Lab Expo in Atlanta. The team, led by Joris R. Delanghe, MD, PhD, of the Department of Global Chemistry, Microbiology and Immunology at Ghent University, collected nail clippings from 25 people with T2DM and 25 without the disease. The clippings were ground into a powder and tested with an inexpensive FT-IR photometer to measure how much the protein in the nails had bonded with sugar molecules, a process known as glycation. “We found a striking difference in the measurements between the control group and the patients with diabetes,” Delanghe said. In an interview with Evidence-Based Diabetes Management, he said replacing the standard blood test to measure glycated hemoglobin is a huge advantage. In many cultures, he said, “Taking blood is something that cannot be tolerated.” - See more at: http://www.ajmc.com/journals/evidence-based-diabetes-management/2015/september-2015/fingernail-tests-may-offer-cheap-simple-way-to-diagnose-diabetes#sthash.XQxnBcNO.dpuf

A man's age matters. As men get older, the chances of conceiving and having a healthy child decline. Male fertility starts to decline after 40 when sperm quality decreases. This means it takes longer for their partners to conceive and when they do, there's an increased risk of miscarriage.

Hysteroscopy is a procedure that allows your doctor to look inside your uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
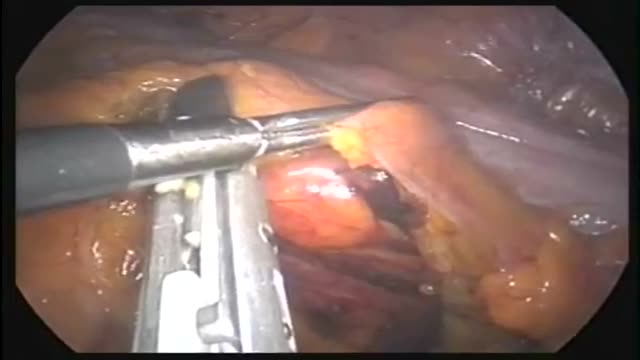
This operation can be performed as an open or laparoscopic (keyhole procedure). During the operation the sigmoid colon is removed. This involves taking away the blood vessels and lymph nodes to that part of the bowel. The surgeon then re-makes the join (anastomosis) between the remaining left side of the colon and the top of the rectum. The surgeon may use either sutures or special staples to make this join.
This short course reviews the main features of EKG tracings. A method for analyzing EKGs is also presented. This method includes assessment of rhythm, calculating heart rate, observing P-wave forms, measurement of EKG intervals and segments and the evaluation of other relevant waves.
Transvenous cardiac pace maker, also called endocardial pacing, is a potentially life saving intervention used primarily to correct profound bradycardia. It can be used to treat symptomatic bradycardias that do not respond to transcutaneous pacing or to drug therapy.

Get a 60-day free trial at https://shipstation.com/doctormike. Thanks to ShipStation for sponsoring the show!
I’ll teach you how to become to media’s go-to expert in your field. Enroll in The Professional’s Media Academy now: https://www.professionalsmediaacademy.com/
Listen to my podcast, @DoctorMikeCheckup, here:
Spotify: https://go.doctormikemedia.com..../spotify/CheckUpSpot
Apple Podcasts: https://go.doctormikemedia.com..../applepodcast/AppleP
Body Bizarre is a TLC show with a name I'm not too wild about, but with stories that are nonetheless fascinating. Today we look at separating conjoined twins, a girl with ants crawling out of her ears, a man who nearly lost his hand in a factory accident, a family that all has 6 fingers, and more.
Help us continue the fight against medical misinformation and change the world through charity by becoming a Doctor Mike Resident on Patreon where every month I donate 100% of the proceeds to the charity, organization, or cause of your choice! Residents get access to bonus content, an exclusive discord community, and many other perks for just $10 a month. Become a Resident today:
https://www.patreon.com/doctormike
Let’s connect:
IG: https://go.doctormikemedia.com..../instagram/DMinstagr
Twitter: https://go.doctormikemedia.com/twitter/DMTwitter
FB: https://go.doctormikemedia.com/facebook/DMFacebook
TikTok: https://go.doctormikemedia.com/tiktok/DMTikTok
Reddit: https://go.doctormikemedia.com/reddit/DMReddit
Contact Email: DoctorMikeMedia@Gmail.com
Executive Producer: Doctor Mike
Production Director and Editor: Dan Owens
Managing Editor and Producer: Sam Bowers
Editor and Designer: Caroline Weigum
Editor: Juan Carlos Zuniga
* Select photos/videos provided by Getty Images *
** The information in this video is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional **

To learn more about licensing this video for content marketing or patient education purposes, visit: http://www.nucleushealth.com/?utm_source=youtube&utm_medium=video-description&utm_campaign=stroke-071411
This video, created by Nucleus Medical Media, gives a thorough explanation of stroke, covering anatomy and physiology, different types of stroke, and treatment.
ANH11048

Electrical cardioversion is a procedure in which an electric current is used to reset the heart's rhythm back to its regular pattern (normal sinus rhythm). The low-voltage electric current enters the body through metal paddles or patches applied to the chest wall.





