Top videos

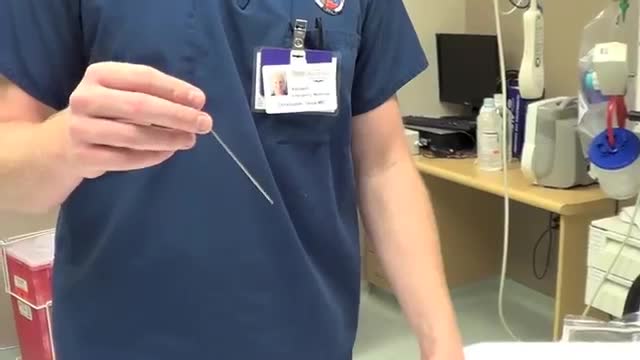
A simple test of fingernail clippings could replace a blood draw as a way to diagnose and monitor type 2 diabetes mellitus (T2DM), with huge implications for tracking the disease in the developing world. Research on this method by a team of Belgian researchers was reported July 28, 2015, at the 2015 American Association for Clinical Chemistry (AACC) Annual Meeting and Clinical Lab Expo in Atlanta. The team, led by Joris R. Delanghe, MD, PhD, of the Department of Global Chemistry, Microbiology and Immunology at Ghent University, collected nail clippings from 25 people with T2DM and 25 without the disease. The clippings were ground into a powder and tested with an inexpensive FT-IR photometer to measure how much the protein in the nails had bonded with sugar molecules, a process known as glycation. “We found a striking difference in the measurements between the control group and the patients with diabetes,” Delanghe said. In an interview with Evidence-Based Diabetes Management, he said replacing the standard blood test to measure glycated hemoglobin is a huge advantage. In many cultures, he said, “Taking blood is something that cannot be tolerated.” - See more at: http://www.ajmc.com/journals/evidence-based-diabetes-management/2015/september-2015/fingernail-tests-may-offer-cheap-simple-way-to-diagnose-diabetes#sthash.XQxnBcNO.dpuf
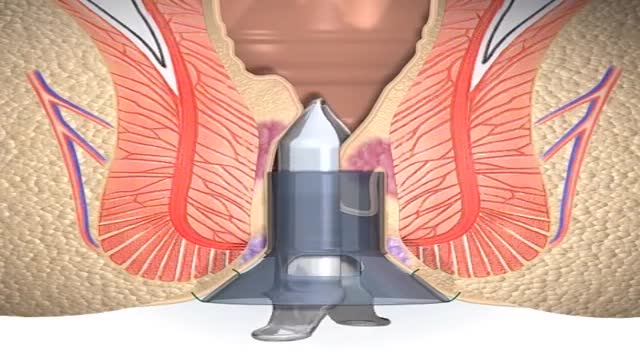
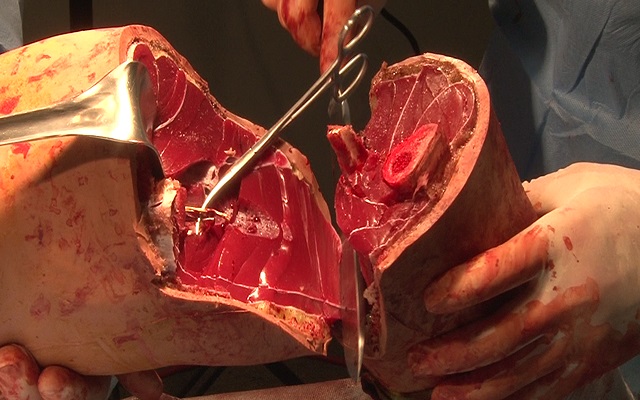
A stapled haemorrhoidopexy is an operation to return the haemorrhoids to a normal. position inside the rectum (back passage). A circular shaped stapling device is gently. inserted in the back passage. The surgeon is then able to use the device to remove.

A man's age matters. As men get older, the chances of conceiving and having a healthy child decline. Male fertility starts to decline after 40 when sperm quality decreases. This means it takes longer for their partners to conceive and when they do, there's an increased risk of miscarriage.
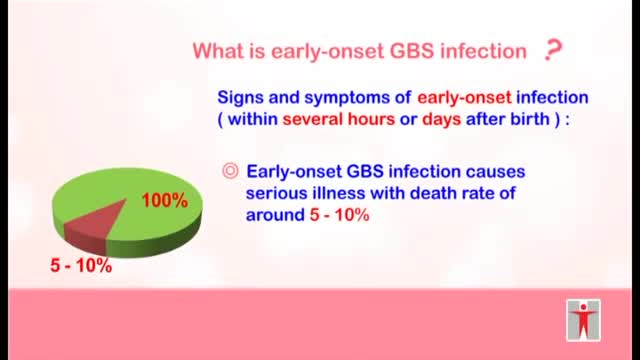
-Intrapartum antibiotic prophylaxis for mothers colonized with group B Streptococcus can prevent early-onset neonatal disease. Adequate prophylaxis consists of ampicillin, penicillin, or cefazolin for ;::4 hours before delivery. Regardless of intrapartum treatment, all high-risk infants must be observed for ;::49 hours. A complete blood count with differential and blood culture are indicated if the infant is preterm <37 weeks or was exposed to prolonged rupture of membranes.>18 hrs.
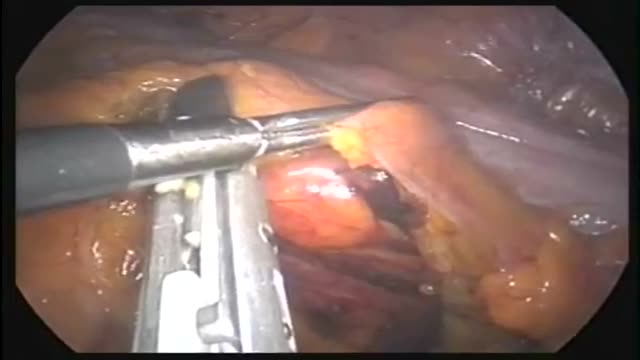
This operation can be performed as an open or laparoscopic (keyhole procedure). During the operation the sigmoid colon is removed. This involves taking away the blood vessels and lymph nodes to that part of the bowel. The surgeon then re-makes the join (anastomosis) between the remaining left side of the colon and the top of the rectum. The surgeon may use either sutures or special staples to make this join.

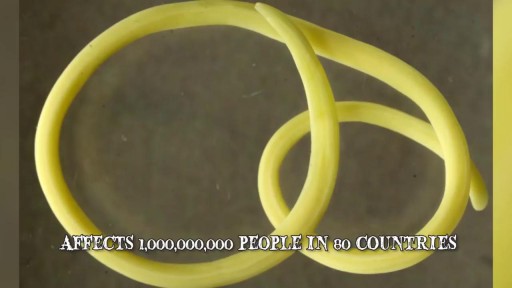
Cells may have slender extensions of the cell membrane to form cilia or the smaller extensions called microvilli. The microscopic microvilli effectively increase the surface area of the cell and are useful for absorption and secretion functions. A dramatic example is the human small intestine. The tissue has small fingerlike extensions called villi which are collections of cells, and those cells have many microvilli to even further increase the available surface area for the digestion process. According to Audesirk & Audesirk, this can give an effective surface area of about 250 square meters for absorption.
This short course reviews the main features of EKG tracings. A method for analyzing EKGs is also presented. This method includes assessment of rhythm, calculating heart rate, observing P-wave forms, measurement of EKG intervals and segments and the evaluation of other relevant waves.
Transvenous cardiac pace maker, also called endocardial pacing, is a potentially life saving intervention used primarily to correct profound bradycardia. It can be used to treat symptomatic bradycardias that do not respond to transcutaneous pacing or to drug therapy.

From our beginnings in 1990 in primary healthcare, Healthway Medical has grown to become a respected medical group in Singapore. With over 100 clinics and medical centres, Healthway Medical has a wide network of medical centres and clinics in Singapore.
We offer comprehensive services including GP & family medicine clinics, health screening, adult specialists, baby & child specialists, dental services and allied healthcare services.

Obesity is one of the most pervasive, chronic diseases in need of new strategies for medical treatment and prevention. As a leading cause of United States mortality, morbidity, disability, healthcare utilization and healthcare costs, the high prevalence of obesity continues to strain the United States healthcare system. Obesity is defined as excess adipose tissue. There are several different methods for determining excess adipose (fat) tissue; the most common being the Body Mass Index (BMI) (see below). A fat cell is an endocrine cell and adipose tissue is an endocrine organ. As such, adipose tissue secretes a number of products, including metabolites, cytokines, lipids, and coagulation factors among others. Significantly, excess adiposity or obesity causes increased levels of circulating fatty acids and inflammation. This can lead to insulin resistance, which in turn can lead to type 2 diabetes.

Electrical cardioversion is a procedure in which an electric current is used to reset the heart's rhythm back to its regular pattern (normal sinus rhythm). The low-voltage electric current enters the body through metal paddles or patches applied to the chest wall.
A C-reactive protein (CRP) test is a blood test that measures the amount of a protein called C-reactive protein in your blood. C-reactive protein measures general levels of inflammation in your body. High levels of CRP are caused by infections and many long-term diseases.
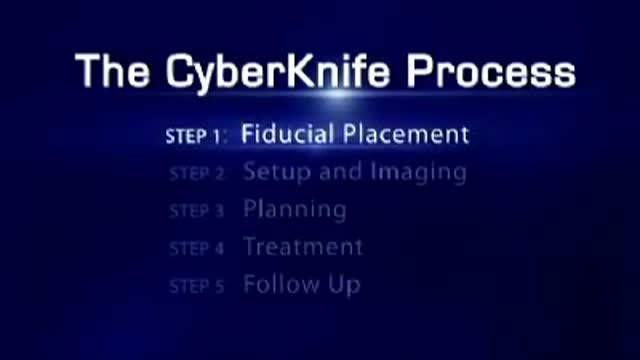
Radiosurgery: Radiosurgery devices, such as the CyberKnife Robotic Radiosurgery System, offer patients a new option for the treatment of lung cancer. The CyberKnife® System is used to treat lung cancer patients who cannot tolerate surgery, have an inoperable tumor, or are seeking an alternative to surgery.
The essential components of the human cardiovascular system are the heart, blood and blood vessels. It includes the pulmonary circulation, a "loop" through the lungs where blood is oxygenated; and the systemic circulation, a "loop" through the rest of the body to provide oxygenated blood.