Top videos

A simple test of fingernail clippings could replace a blood draw as a way to diagnose and monitor type 2 diabetes mellitus (T2DM), with huge implications for tracking the disease in the developing world. Research on this method by a team of Belgian researchers was reported July 28, 2015, at the 2015 American Association for Clinical Chemistry (AACC) Annual Meeting and Clinical Lab Expo in Atlanta. The team, led by Joris R. Delanghe, MD, PhD, of the Department of Global Chemistry, Microbiology and Immunology at Ghent University, collected nail clippings from 25 people with T2DM and 25 without the disease. The clippings were ground into a powder and tested with an inexpensive FT-IR photometer to measure how much the protein in the nails had bonded with sugar molecules, a process known as glycation. “We found a striking difference in the measurements between the control group and the patients with diabetes,” Delanghe said. In an interview with Evidence-Based Diabetes Management, he said replacing the standard blood test to measure glycated hemoglobin is a huge advantage. In many cultures, he said, “Taking blood is something that cannot be tolerated.” - See more at: http://www.ajmc.com/journals/evidence-based-diabetes-management/2015/september-2015/fingernail-tests-may-offer-cheap-simple-way-to-diagnose-diabetes#sthash.XQxnBcNO.dpuf
Thyroid nodules are solid or fluid-filled lumps that form within your thyroid, a small gland located at the base of your neck, just above your breastbone. The great majority of thyroid nodules aren't serious and don't cause symptoms. Thyroid cancer accounts for only a small percentage of thyroid nodules. You often won't know you have a thyroid nodule until your doctor discovers it during a routine medical exam. Some thyroid nodules, however, may become large enough to be visible or make it difficult to swallow or breathe.

In the Dialysis Unit you have an opportunity to provide Dialysis care for a variety of patients, including those with End-Stage Chronic Kidney disease and acutely ill patients requiring dialysis and plasmapheresis.
The Chronic Dialysis Nurse focuses on patients receiving Hemodialysis, Peritoneal Dialysis, or Home Hemodialysis. Our patients range in age from newborns to young adults. The Hemodialysis patient receives their dialysis treatment in the clinic 3-5 times a week. The Peritoneal Dialysis and Home Hemodialysis treatments are provided in the patient’s home once the parent/caregiver is trained to operate the machine. They are followed monthly in clinic. The patient receiving Chronic Dialysis is supported by a multidisciplinary team that consists of a physician, nurses, social worker, nutritionist, pharmacist, child-life therapist, teacher, and counselor. The group works together to meet the medical and emotional needs of the patient and caregiver. Care is specialized to meet the needs of each individual patient.
The Acute Dialysis Nurse focuses on acute dialysis related therapies such as: Continuous Renal Replacement Therapy (CRRT); therapeutic plasmapheresis; or acute peritoneal dialysis. The acute dialysis team works with the multi-disciplinary inpatient nephrology team to provide acute dialysis services to the critically ill ICU patients. The work environment is highly technical and fast-paced.
The Dialysis Unit operates on 12hr shifts 7a – 7p; 7 days a week. Night call is required and shared by the nurses. We provide a detailed orientation plan to the nurse to become proficient in providing hemodialysis, peritoneal dialysis, continuous renal replacement therapy and plasmapheresis. Previous experience in dialysis or pediatrics is not required.
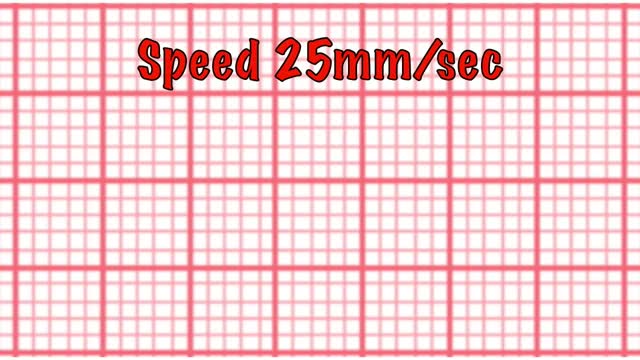
This short course reviews the main features of EKG tracings. A method for analyzing EKGs is also presented. This method includes assessment of rhythm, calculating heart rate, observing P-wave forms, measurement of EKG intervals and segments and the evaluation of other relevant waves.

Stomach acid is natural, a valuable chemical contributor to orderly digestion. But in excess or in the wrong place, it's a menace, inflaming and irritating the esophagus, typically causing heartburn and sometimes contributing to the development of ulcers in the stomach and the duodenum, the first part of the small intestine.

We are looking for 5 patients with knee pain who want to get significantly better in the next 30 days. Click this link to let me know you're interested and learn more.
https://www.drdavidgeier.com/work-with-me/contact/
If you suffer a knee injury, what do you do about it? Should you be concerned? On one hand, you could give it a few days to see if it gets better on its own. How can you know if you risk making the problem worse? In this Ask Dr. Geier video, I offer four signs you have a serious knee injury that could require surgery.
Please note: I don't respond to questions and requests for specific medical advice left in the comments to my videos. I receive too many to keep up (several hundred per week), and legally I can't offer specific medical advice to people who aren't my patients (see below). If you want to ask a question about a specific injury you have, leave it in the comments below, and I might answer it in an upcoming Ask Dr. Geier video. If you need more detailed information on your injury, go to my Resources page: https://www.drdavidgeier.com/resources/
The content of this YouTube Channel, https://www.youtube.com/user/drdavidgeier (“Channel”) is for INFORMATIONAL PURPOSES ONLY. The Channel may offer health, fitness, nutritional and other such information, but such information is intended for educational and informational purposes only. This content should not be used to self-diagnose or self-treat any health, medical, or physical condition. The content does not and is not intended to convey medical advice and does not constitute the practice of medicine. YOU SHOULD NOT RELY ON THIS INFORMATION AS A SUBSTITUTE FOR, NOR DOES IT REPLACE, PROFESSIONAL MEDICAL ADVICE, DIAGNOSIS, OR TREATMENT. You should consult with your healthcare professional before doing anything contained on this Channel. You agree that Dr. Geier is not responsible for any actions or inaction on your part based on the information that is presented on the Channel. Dr. David Geier Enterprises, LLC makes no representations about the accuracy or suitability of the content. USE OF THE CONTENT IS AT YOUR OWN RISK.
SWELLING
If you have a knee that is much more swollen than the opposite knee, especially if the swelling developed soon after you got hurt, then it could be a sign of structural damage. While a small amount of swelling could be normal or a sign of inflammation in the knee, a knee that is really swollen and much larger than the other knee could represent a fracture, torn ACL or other ligament or some other damaged structure.
INABILITY TO FULLY STRAIGHTEN YOUR KNEE
Pain can make it difficult for you to straighten your knee. But being unable to get your knee completely flat can be a sign of an injury like an ACL tear or meniscus tear.
LOCKING OF THE KNEE
Locking is a term orthopedic surgeons use to describe a knee that gets stuck in a certain position. Maybe you can straighten it to a certain point, but it gets stuck around 30 degrees short of fully straight. Or you can’t bend it past a certain point because something inside the knee is blocking it. Catching is a milder form of the same problem, where you can get to the point that the motion stops, but you can twist or rotate your knee past that point.
BUCKLING OR GIVING WAY
Having the tibia (shin bone) shift out from under the femur (thigh bone) usually represents an ACL injury. If your knee buckled during the traumatic injury and keeps happening in the days after the injury, you risk doing more damage to the other structures inside the knee.
This list is not comprehensive, so if you are concerned about your knee injury or knee pain, it never hurts to see your doctor or an orthopedic surgeon.
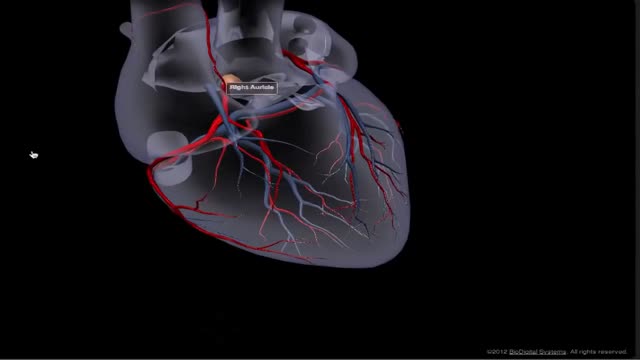
The heart receives its own supply of blood from the coronary arteries. Two major coronary arteries branch off from the aorta near the point where the aorta and the left ventricle meet. These arteries and their branches supply all parts of the heart muscle with blood.
A C-reactive protein (CRP) test is a blood test that measures the amount of a protein called C-reactive protein in your blood. C-reactive protein measures general levels of inflammation in your body. High levels of CRP are caused by infections and many long-term diseases.

In this video, I will be sharing simple tests and exercises which will diagnose your knee pain.
These tests will help with the knee pain diagnosis.
In addition, I will share the most effective therapy and exercises with you which you can do from the comfort of your own home.
Time Stamp:
00:00 Introduction
00:59 Anatomy Inside of the Knee
02:19 Test for Pain on Inside of knee (MCL)
03:12 HARM Protocol
03:30 POLICE Protocol
04:44 Home Therapy MCL Sprain
06:06 Home Exercises MCL Sprain
09:21 Test for Pain on Outside of Knee (LCL)
11:11 Renne's Test (ITB Band)
13:39 Symptoms of Meniscus Tear
13:59 Thessaly Test for Meniscus Tear
14:49 Ege's Test for Meniscus Tear
Our Clinics:
Milton Chiropractic Clinic
2 Ely Road
Milton, Cambridge
CB24 6DD
United Kingdom
Tel: +44 (0) 1223 864444
https://www.miltonchiropractic.co.uk
Fornham Chiropractic Clinic
Unit 10
Fornham Business Court
Hall Farm
Fornham St Martin
Bury St Edmunds
IP31 1SL
United Kingdom
Tel: +44 (0) 1284 220202
https://www.fornhamchiropractic.co.uk
atrial septal defect (ASD) is a hole in the wall between the two upper chambers of your heart (atria). The condition is present from birth (congenital). Small atrial septal defects may close on their own during infancy or early childhood. Large and long-standing atrial septal defects can damage your heart and lungs. Small defects may never cause a problem and may be found incidentally. An adult who has had an undetected atrial septal defect for decades may have a shortened life span from heart failure or high blood pressure that affects the arteries in the lungs (pulmonary hypertension). Surgery may be necessary to repair atrial septal defects to prevent complications
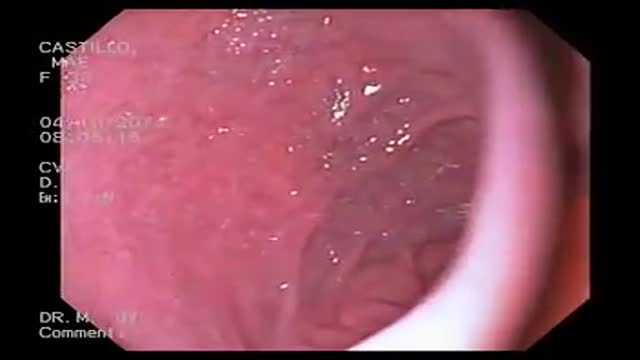
A gastroscopy is a procedure where a thin, flexible tube called an endoscope is used to look inside the oesophagus (gullet), stomach and first part of the small intestine (duodenum). It's also sometimes referred to as an upper gastrointestinal endoscopy. The endoscope has a light and a camera at one end.
Anaphylaxis is a severe, potentially life-threatening allergic reaction. It can occur within seconds or minutes of exposure to something you're allergic to, such as a peanut or the venom from a bee sting. The flood of chemicals released by your immune system during anaphylaxis can cause you to go into shock; your blood pressure drops suddenly and your airways narrow, blocking normal breathing. Signs and symptoms of anaphylaxis include a rapid, weak pulse, a skin rash, and nausea and vomiting. Common triggers of anaphylaxis include certain foods, some medications, insect venom and latex. Anaphylaxis requires an immediate trip to the emergency department and an injection of epinephrine. If anaphylaxis isn't treated right away, it can lead to unconsciousness or even death.

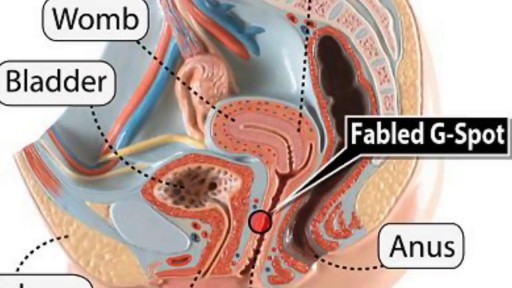
Endometrial cancer is a type of cancer that begins in the uterus. The uterus is the hollow, pear-shaped pelvic organ in women where fetal development occurs. Endometrial cancer begins in the layer of cells that form the lining (endometrium) of the uterus. Endometrial cancer is sometimes called uterine cancer. Other types of cancer can form in the uterus, including uterine sarcoma, but they are much less common than endometrial cancer. Endometrial cancer is often detected at an early stage because it frequently produces abnormal vaginal bleeding, which prompts women to see their doctors. If endometrial cancer is discovered early, removing the uterus surgically often cures endometrial cancer.
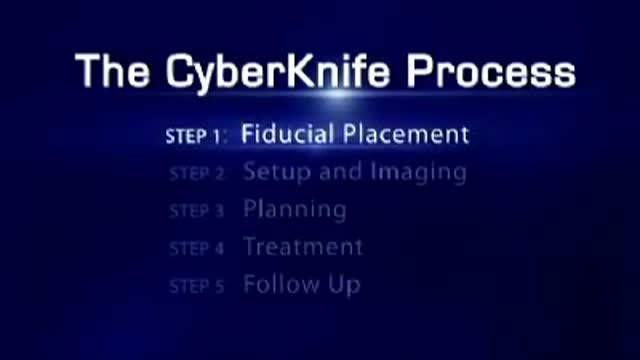
Radiosurgery: Radiosurgery devices, such as the CyberKnife Robotic Radiosurgery System, offer patients a new option for the treatment of lung cancer. The CyberKnife® System is used to treat lung cancer patients who cannot tolerate surgery, have an inoperable tumor, or are seeking an alternative to surgery.

Cells may have slender extensions of the cell membrane to form cilia or the smaller extensions called microvilli. The microscopic microvilli effectively increase the surface area of the cell and are useful for absorption and secretion functions. A dramatic example is the human small intestine. The tissue has small fingerlike extensions called villi which are collections of cells, and those cells have many microvilli to even further increase the available surface area for the digestion process. According to Audesirk & Audesirk, this can give an effective surface area of about 250 square meters for absorption.