Top videos

Lipomas are slow-growing soft tissue tumours that rarely reach a size larger than 2 cm. Lesions larger than 5 cm, so-called giant lipomas, can occur anywhere in the body but are seldom found in the upper extremities. The authors present their experiences with eight patients having giant lipomas of the upper extremity. In addition, a review of the literature, and a discussion of the appropriate evaluation and management are included.
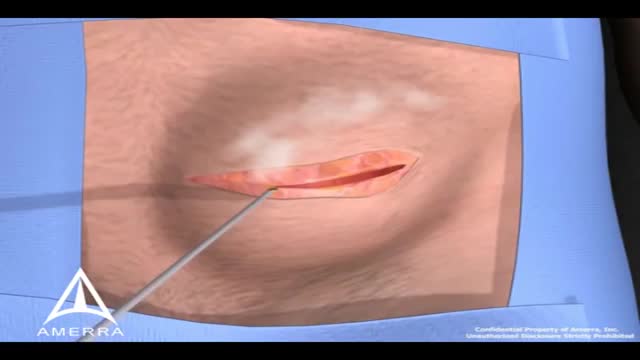
During surgery to repair the hernia, the bulging tissue is pushed back in. Your abdominal wall is strengthened and supported with sutures (stitches), and sometimes mesh. This repair can be done with open or laparoscopic surgery. You and your surgeon can discuss which type of surgery is right for you.

What is hemodiafiltration? Hemodiafiltration, or HDF, is a renal replacement modality that combines diffusion and convection to improve removal of molecules in the middle molecular weight range versus hemodialysis.
Find our full video library only on Osmosis Prime: http://osms.it/more.
Join over 3 million current & future clinicians who learn by Osmosis, and over 130 universities around the world who partner with us to make medical and health education more engaging and efficient. We have unparalleled tools and materials to prepare you to succeed in school, on board exams, and as a future clinician. Sign up for a free trial at http://osms.it/more. If you're interested in exploring an institutional partnership, visit osmosis.org/educators to request a personalized demo.
Follow us on social:
Facebook: http://osms.it/facebook
Twitter: http://osms.it/twitter
Instagram for med: http://osms.it/instagram
Instagram for nursing: https://osms.it/ignursing
Linkedin: https://osms.it/linkedin
Our Vision: Everyone who cares for someone will learn by Osmosis.
Our Mission: To empower the world’s clinicians and caregivers with the best learning experience possible. Learn more here: http://osms.it/mission
Medical disclaimer: Knowledge Diffusion Inc (DBA Osmosis) does not provide medical advice. Osmosis and the content available on Osmosis's properties (Osmosis.org, YouTube, and other channels) do not provide a diagnosis or other recommendation for treatment and are not a substitute for the professional judgment of a healthcare professional in diagnosis and treatment of any person or animal. The determination of the need for medical services and the types of healthcare to be provided to a patient are decisions that should be made only by a physician or other licensed health care provider. Always seek the advice of a physician or other qualified healthcare provider with any questions you have regarding a medical condition. © 2023 Elsevier. All rights reserved.
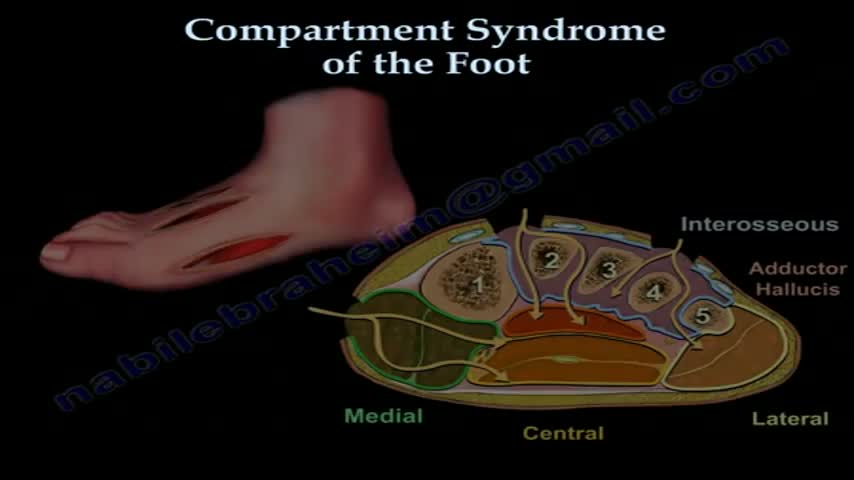
Compartment syndrome can develop in the foot following crush injury or closed fracture. Following some critical threshold of bleeding and/or swelling into the fixed space compartments, arterial pulse pressure is insufficient to overcome the osmotic tissue pressure gradient, leading to cell death. The complicating factor is related to the magnitude of the force of the crush injury. The amount of swelling or bleeding has to be sufficient to impair arterial inflow, while not being of sufficient magnitude to produce an open injury, which decompresses the pressure within the affected compartments. When the injury is open, we then attribute the late disability primarily to the crushing injury to the involved muscles.
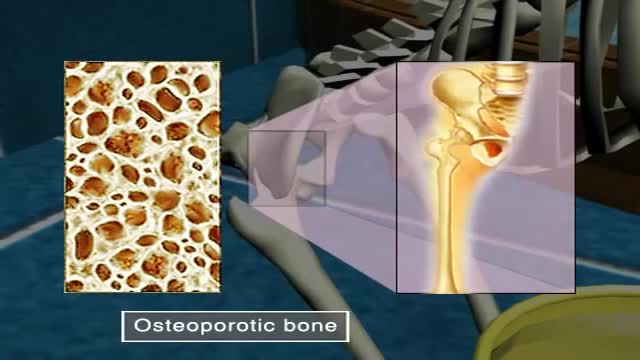
Osteoporosis, which literally means porous bone, is a disease in which the density and quality of bone are reduced. As bones become more porous and fragile, the risk of fracture is greatly increased. The loss of bone occurs silently and progressively. Often there are no symptoms until the first fracture occurs.
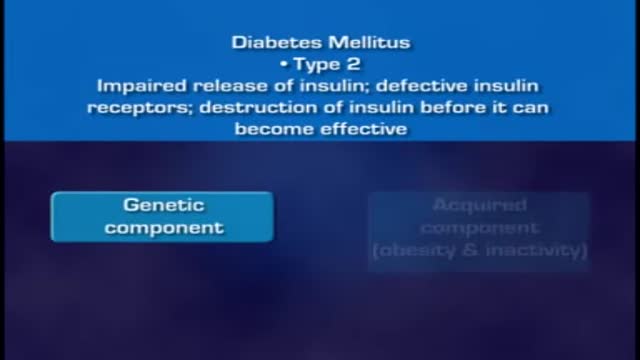
When food is taken, it is broken down into smaller components. Sugars and carbohydrates are thus broken down into glucose for the body to utilize them as an energy source. The liver is also able to manufacture glucose. In normal persons the hormone insulin, which is made by the beta cells of the pancreas, regulates how much glucose is in the blood. When there is excess of glucose in blood, insulin stimulates cells to absorb enough glucose from the blood for the energy that they need. Insulin also stimulates the liver to absorb and store any excess glucose that is in the blood. Insulin release is triggered after a meal when there is a rise in blood glucose. When blood glucose levels fall, during exercise for example, insulin levels fall too. High insulin will promote glucose uptake, glycolysis (break down of glucose), and glycogenesis (formation of storage form of glucose called glycogen), as well as uptake and synthesis of amino acids, proteins, and fat. Low insulin will promote gluconeogenesis (breakdown of various substrates to release glucose), glycogenolysis (breakdown of glycogen to release gluose), lipolysis (breakdown of lipids to release glucose), and proteolysis (breakdown of proteins to release glucose). Insulin acts via insulin receptors.

The CSICU rounds are an opportunity for residents to come together with attendings and review all the patients in the ICU.
Cedars-Sinai is committed to educating exceptional cardiothoracic surgeons through outstanding personal mentorship, operative training and research leadership. Residents of the Thoracic Surgery—Integrated Residency at Cedars-Sinai will be part of an incredibly rich, academic environment—each year our research and thought leadership features in hundreds of publications in journals including Nature, New England Journal of Medicine, JAMA, Lancet and leading specialty journals.
Learn more about the Cedars-Sinai Thoracic Surgery—Integrated Residency: https://ceda.rs/3UDrZFL
Connect with us:
https://twitter.com/CedarsSinai
https://www.facebook.com/CedarsSinai
https://www.instagram.com/CedarsSinai
Cedars-Sinai is a leader in providing high-quality healthcare encompassing primary care, specialized medicine and research. Since 1902, Cedars-Sinai has evolved to meet the needs of one of the most diverse regions in the nation, setting standards in quality and innovative patient care, research, teaching and community service. Today, Cedars- Sinai is known for its national leadership in transforming healthcare for the benefit of patients. Cedars-Sinai impacts the future of healthcare by developing new approaches to treatment and educating tomorrow’s health professionals. Additionally, Cedars-Sinai demonstrates a commitment to the community through programs that improve the health of its most vulnerable residents.
A modified radical mastectomy is a procedure in which the entire breast is removed, including the skin, areola, nipple, and most axillary lymph nodes; the pectoralis major muscle is spared. Historically, a modified radical mastectomy was the primary method of treatment of breast cancer. [1, 2] As the treatment of breast cancer evolved, breast conservation has become more widely used. [3, 4] However, mastectomy still remains a viable option for women with breast cancer. [5, 6]
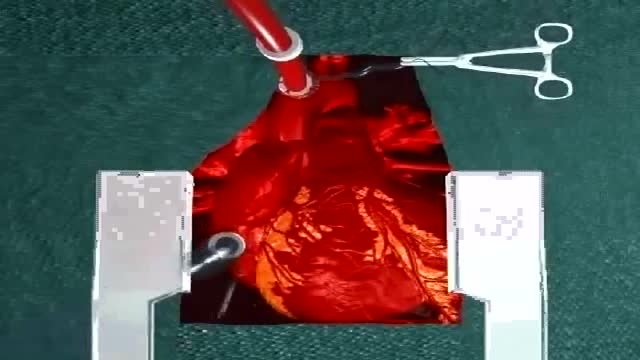
Coronary artery bypass grafting (CABG) is a type of surgery that improves blood flow to the heart. Surgeons use CABG to treat people who have severe coronary heart disease (CHD). CHD is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries.

Research from Mayo Clinic finds that half of elderly patients who start dialysis after age 75 will die within one year.
Lead study author and a health care delivery scholar with the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Dr. Bjorg Thorsteinsdottir says many elderly patients and their families feel that they have no choice but to start dialysis, with several expressing regret from having initiated therapy.
The findings were presented at the American Society of Nephrology's Kidney Week 2013 in Atlanta.
Genital warts are growths on the skin of the genital area and around the anus. They are caused by certain types of the human papilloma virus (HPV). There are more than 100 types of HPV. Some types of HPV produce warts on different parts of the body, like plantar warts on the feet and common hand warts. There is no specific treatment for HPV, but there are treatments for health problems caused by HPV. Genital warts can be treated by your healthcare provider, or with prescription medication. HPV-related cancers are more treatable when diagnosed and treated promptly. For more information, visit www.cancer.org.

Here we’ll explain the symptoms of pancreatitis, how alcohol causes the condition and the other health problems it can lead to. You probably don’t pay much attention to your pancreas. But that small, tadpole-shaped organ behind your stomach and below your ribcage is pretty important. It produces two essential substances: digestive juices which your intestines use to break down food, and hormones that are involved in digestion, such as insulin, which regulates your blood sugar levels. Pancreatitis is when your pancreas becomes inflamed and its cells are damaged. Heavy drinking can cause pancreatitis. But if you drink within the government’s low risk unit guidelines, you should avoid upsetting this important organ.
Diabetes is a growing global health concern, as is obesity. Diabetes and obesity are intrinsically linked: obesity increases the risk of diabetes and also contributes to disease progression and cardiovascular disease. Although the benefits of weight loss in the prevention of diabetes and as a critical component of managing the condition are well established, weight reduction remains challenging for individuals with type 2 diabetes due to a host of metabolic and psychological factors. For many patients, lifestyle intervention is not enough to achieve weight loss, and alternative options, such as pharmacotherapy, need to be considered. However, many traditional glucose-lowering medications may lead to weight gain. This article focuses on the potential of currently available pharmacological strategies and on emerging approaches in development to support the glycemic and weight-loss goals of individuals with type 2 diabetes. Two pharmacotherapy types are considered: those developed primarily for blood glucose control that have a favorable effect on body weight and those developed primarily to induce weight loss that have a favorable effect on blood glucose control. Finally, the potential of combination therapies for the management of obese patients with type 2 diabetes is discussed.

Three cholinesterase inhibitors are commonly prescribed: Donepezil (Aricept) is approved to treat all stages of Alzheimer's. Rivastigmine (Exelon) is approved to treat mild to moderate Alzheimer's. Galantamine (Razadyne) is approved to treat mild to moderate Alzheimer's. Currently, there is no cure for Alzheimer's. But drug and non-drug treatments may help with both cognitive and behavioral symptoms. Researchers are looking for new treatments to alter the course of the disease and improve the quality of life for people with dementia. ... Medications for Memory Loss.

A palatal view of a maxillary premolar during a crown lengthening procedure. Crown lengthening is a surgical procedure performed by a dentist to expose a greater amount of tooth structure for the purpose of subsequently restoring the tooth prosthetically.

You should not use aspirin if you have a bleeding disorder such as hemophilia, a recent history of stomach or intestinal bleeding, or if you are allergic to an NSAID (non-steroidal anti-inflammatory drug) such as Advil, Motrin, Aleve, Orudis, Indocin, Lodine, Voltaren, Toradol, Mobic, Relafen, Feldene, and others. Do not give this medication to a child or teenager with a fever, flu symptoms, or chicken pox. Salicylates can cause Reye's syndrome, a serious and sometimes fatal condition in children.