Top videos
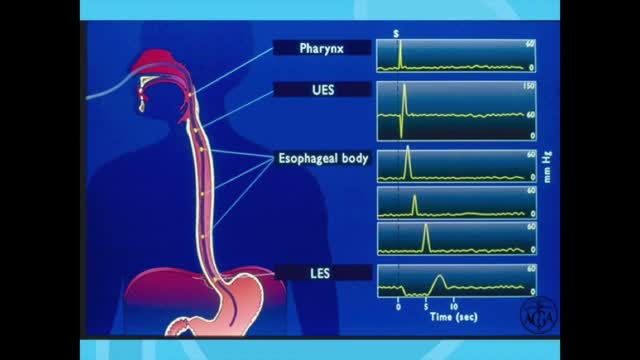
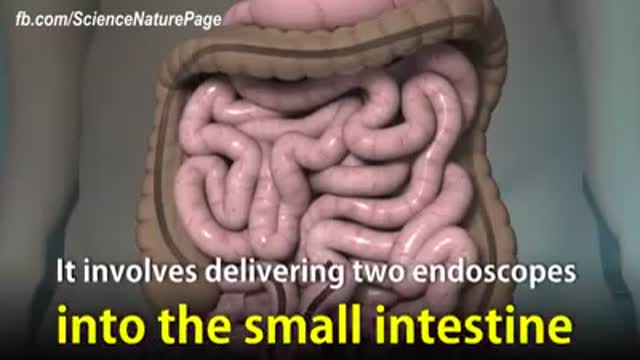
Esophageal manometry is a test used to measure the function of the lower esophageal sphincter (the valve that prevents reflux of gastric acid into the esophagus) and the muscles of the esophagus (see diagram). This test will tell your doctor if your esophagus is able to move food to your stomach normally.
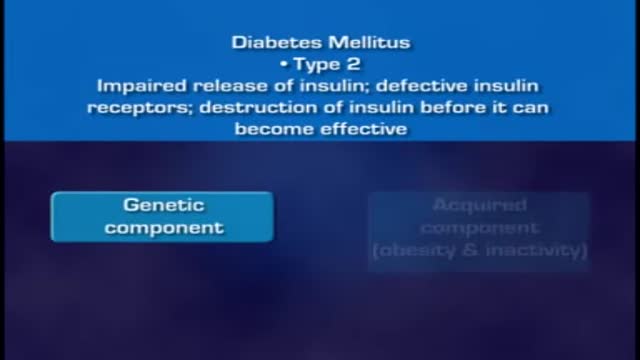
When food is taken, it is broken down into smaller components. Sugars and carbohydrates are thus broken down into glucose for the body to utilize them as an energy source. The liver is also able to manufacture glucose. In normal persons the hormone insulin, which is made by the beta cells of the pancreas, regulates how much glucose is in the blood. When there is excess of glucose in blood, insulin stimulates cells to absorb enough glucose from the blood for the energy that they need. Insulin also stimulates the liver to absorb and store any excess glucose that is in the blood. Insulin release is triggered after a meal when there is a rise in blood glucose. When blood glucose levels fall, during exercise for example, insulin levels fall too. High insulin will promote glucose uptake, glycolysis (break down of glucose), and glycogenesis (formation of storage form of glucose called glycogen), as well as uptake and synthesis of amino acids, proteins, and fat. Low insulin will promote gluconeogenesis (breakdown of various substrates to release glucose), glycogenolysis (breakdown of glycogen to release gluose), lipolysis (breakdown of lipids to release glucose), and proteolysis (breakdown of proteins to release glucose). Insulin acts via insulin receptors.
A modified radical mastectomy is a procedure in which the entire breast is removed, including the skin, areola, nipple, and most axillary lymph nodes; the pectoralis major muscle is spared. Historically, a modified radical mastectomy was the primary method of treatment of breast cancer. [1, 2] As the treatment of breast cancer evolved, breast conservation has become more widely used. [3, 4] However, mastectomy still remains a viable option for women with breast cancer. [5, 6]
Coronary artery bypass grafting (CABG) is a type of surgery that improves blood flow to the heart. Surgeons use CABG to treat people who have severe coronary heart disease (CHD). CHD is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries.
Genital warts are growths on the skin of the genital area and around the anus. They are caused by certain types of the human papilloma virus (HPV). There are more than 100 types of HPV. Some types of HPV produce warts on different parts of the body, like plantar warts on the feet and common hand warts. There is no specific treatment for HPV, but there are treatments for health problems caused by HPV. Genital warts can be treated by your healthcare provider, or with prescription medication. HPV-related cancers are more treatable when diagnosed and treated promptly. For more information, visit www.cancer.org.
Diabetes is a growing global health concern, as is obesity. Diabetes and obesity are intrinsically linked: obesity increases the risk of diabetes and also contributes to disease progression and cardiovascular disease. Although the benefits of weight loss in the prevention of diabetes and as a critical component of managing the condition are well established, weight reduction remains challenging for individuals with type 2 diabetes due to a host of metabolic and psychological factors. For many patients, lifestyle intervention is not enough to achieve weight loss, and alternative options, such as pharmacotherapy, need to be considered. However, many traditional glucose-lowering medications may lead to weight gain. This article focuses on the potential of currently available pharmacological strategies and on emerging approaches in development to support the glycemic and weight-loss goals of individuals with type 2 diabetes. Two pharmacotherapy types are considered: those developed primarily for blood glucose control that have a favorable effect on body weight and those developed primarily to induce weight loss that have a favorable effect on blood glucose control. Finally, the potential of combination therapies for the management of obese patients with type 2 diabetes is discussed.

Three cholinesterase inhibitors are commonly prescribed: Donepezil (Aricept) is approved to treat all stages of Alzheimer's. Rivastigmine (Exelon) is approved to treat mild to moderate Alzheimer's. Galantamine (Razadyne) is approved to treat mild to moderate Alzheimer's. Currently, there is no cure for Alzheimer's. But drug and non-drug treatments may help with both cognitive and behavioral symptoms. Researchers are looking for new treatments to alter the course of the disease and improve the quality of life for people with dementia. ... Medications for Memory Loss.

Watch Spinal Stenosis Videos Spinal stenosis occurs when the spinal cord in the neck (cervical spine) or the spinal nerve roots in the lower back (lumbar spine) are compressed. Symptoms of lumbar stenosis often include leg pain (sciatica) and leg tingling, weakness, or numbness. Arm pain is a typical symptom of cervical spinal stenosis. For cervical spinal stenosis with myelopathy, difficulty with coordination often occurs. Stenosis treatment may include non-surgical options (exercise, anti-inflammatory medication, epidural injections, and activity modification) or back surgery.

A palatal view of a maxillary premolar during a crown lengthening procedure. Crown lengthening is a surgical procedure performed by a dentist to expose a greater amount of tooth structure for the purpose of subsequently restoring the tooth prosthetically.

Adult-onset Still's disease (AOSD) is a rare systemic inflammatory disease characterized by the classic triad of persistent high spiking fevers, joint pain, and a distinctive salmon-colored bumpy rash. The disease is considered a diagnosis of exclusion.

In vitro fertilization, or IVF, is the most common and effective type of assisted reproductive technology to help women become pregnant. It involves fertilizing an egg outside the body, in a laboratory dish, and then implanting it in a woman's uterus. By 2016, some 6.5 million babies had been born using in-vitro fertilization (IVF). According to the Centers for Disease Control and Prevention (CDC), around 1.6 percent of babies born in the United States each year are conceived through assisted reproductive technology (ART).
Trisomy 18, also called Edwards syndrome, is a chromosomal condition associated with abnormalities in many parts of the body. Individuals with trisomy 18 often have slow growth before birth (intrauterine growth retardation) and a low birth weight. Affected individuals may have heart defects and abnormalities of other organs that develop before birth. Other features of trisomy 18 include a small, abnormally shaped head; a small jaw and mouth; and clenched fists with overlapping fingers. Due to the presence of several life-threatening medical problems, many individuals with trisomy 18 die before birth or within their first month. Five to 10 percent of children with this condition live past their first year, and these children often have severe intellectual disability.

Rheum is made up of mucus, skin cells, oils and dust. The rheum that comes from the eyes and forms eye boogers is called gound, which you may know as eye sand, eye gunk, sleep dust, sleep sand, sleep in your eyes, or eye shnooters. When you're awake, gound doesn't cause any problems.

The following guidelines are an interpretation of the evidence presented in the 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations1). They apply primarily to newly born infants undergoing transition from intrauterine to extrauterine life, but the recommendations are also applicable to neonates who have completed perinatal transition and require resuscitation during the first few weeks to months following birth. Practitioners who resuscitate infants at birth or at any time during the initial hospital admission should consider following these guidelines. For the purposes of these guidelines, the terms newborn and neonate are intended to apply to any infant during the initial hospitalization. The term newly born is intended to apply specifically to an infant at the time of birth.
Multicystic dysplastic kidney (MCDK) is a condition that results from the malformation of the kidney during fetal development. The kidney consists of irregular cysts of varying sizes. Multicystic dysplastic kidney is a common type of renal cystic disease, and it is a cause of an abdominal mass in infants.

Squamous cell carcinomas typically appear as persistent, thick, rough, scaly patches that can bleed if bumped, scratched or scraped. They often look like warts and sometimes appear as open sores with a raised border and a crusted surface. In addition to the signs of SCC shown here, any change in a preexisting skin growth, such as an open sore that fails to heal, or the development of a new growth, should prompt an immediate visit to a physician.