Top videos
This new surgical technique provide good stability for all type of fracture even severe comminution. Each fragment are reduced and several pin sleeves are inserted circumferentially and tighten by braded cable through the sleeve box. The final features of surgery seems blooming sunflower 'Himwari in Jananese'.

Site enhancement oil, often called "santol" or "synthol" (no relation to the Synthol mouthwash brand), refers to oils injected into muscles to increase the size or change the shape. Some bodybuilders, particularly at the professional level, inject their muscles with such mixtures to mimic the appearance of developed muscle where it may otherwise be disproportionate or lagging. This is known as "fluffing".Synthol is 85% oil, 7.5% lidocaine, and 7.5% alcohol. It is not restricted, and many brands are available on the Internet. The use of injected oil to enhance muscle appearance is common among bodybuilders, despite the fact that synthol can cause pulmonary embolisms, nerve damage, infections, sclerosing lipogranuloma,[60] stroke,[55] and the formation of oil-filled granulomas, cysts or ulcers in the muscle. Rare cases might require surgical intervention to avoid further damage to the muscle and/or to prevent loss of life. Sesame oil is often used in such mixtures, which can cause allergic reactions such as vasculitis.

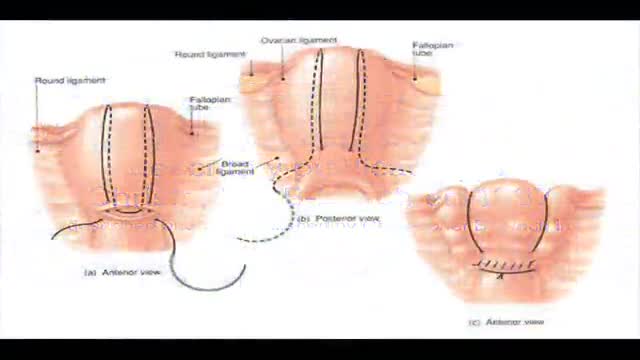
Ankle fusion (arthrodesis) This is a surgical procedure which joins together the main bones of the ankle joint (the tibia and the talus). However, depending on the technique your surgeon will use, occasionally the fibula will be included in this procedure. The two joint surfaces which generate the pain are removed.
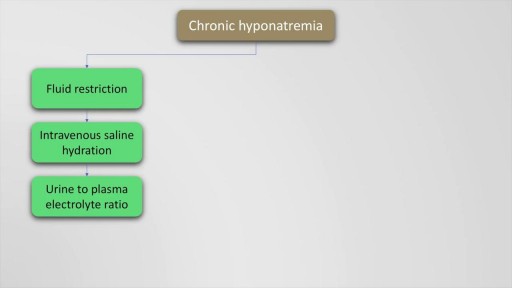
Hyponatremia is defined as a serum sodium of less than 135 Meq per litre and occurs in upto 22 % of hospitalised patients. The causes of hyponatremia may be understood based on the pre-existing volume status of the patient which may either be hypovolemic, euvolemic or hypervolemic hyponatremia. This presentation discusses in detail, the causes of these underlying conditions. Also mentioned are the clinical features and management options and therapeutic sodium targets in patients with hyponatremia. Drugs such as demeclocycline and vaptans (Tolvaptan, Conivaptan) are also mentioned as management options which may be used on a case to case basis. Finally, the all important targets of sodium correction over 24 hours are also mentioned, along with a practical formula for calculation of sodium deficit which is explained with an example.

An amputation is the removal of an extremity or appendage from the body. Amputations in the upper extremity can occur as a result of trauma, or they can be performed in the treatment of congenital or acquired conditions. Although successful replantation represents a technical triumph to the surgeon, the patient's best interests should direct the treatment of amputations. The goals involved in the treatment of amputations of the upper extremity include the following : Preservation of functional length Durable coverage Preservation of useful sensibility Prevention of symptomatic neuromas Prevention of adjacent joint contractures Early return to work Early prosthetic fitting These goals apply differently to different levels of amputation. Treatment of amputations can be challenging and rewarding. It is imperative that the surgeon treat the patient with the ultimate goal of optimizing function and rehabilitation and not become absorbed in the enthusiasm of the technical challenge of the replantation, which could result in poorer outcome and greater financial cost due to lost wages, hospitalization, and therapy.
When the hematocrit rises to 60 or 70%, which it often does in polycythemia, the blood viscosity can become as great as 10 times that of water, and its flow through blood vessels is greatly retarded because of increased resistance to flow. This will lead to decreased oxygen delivery.

Atherosclerosis is a narrowing of the arteries caused by a buildup of plaque. It’s also called arteriosclerosis or hardening of the arteries. Arteries are the blood vessels that carry oxygen and nutrients from your heart to the rest of your body. As you get older, fat and cholesterol can collect in your arteries and form plaque. The buildup of plaque makes it difficult for blood to flow through your arteries. This buildup may occur in any artery in your body and can result in a shortage of blood and oxygen in various tissues of your body. Pieces of plaque can also break off, causing a blood clot. Atherosclerosis can lead to heart attack, stroke, or heart failure if left untreated.

A hematoma is a collection of blood outside of a blood vessel. There are several types of hematomas and they are often described based on their location. Examples of hematomas include subdural, spinal, under the finger or toenail bed (subungual), ear, and liver (hepatic). Some causes of hematomas are as pelvic bone fractures, fingernail injuries (subungual), bumps, passing blood clots, blood clot in the leg (DVT), blood cancers, and excessive alcohol use. Symptoms of hematomas depend upon their location and whether adjacent structures are affected by the inflammation and swelling associated with the bleeding and may include