Top videos

During root canal treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterwards, the tooth is restored with a crown or filling for protection.

Treatment may not be needed for an eschar if it is part of the natural healing process. However, if an eschar looks like it may have a wound infection – symptoms can include oozing fluid such as pus or blood, your clinician will likely recommend topical treatment or debridement to help control and remove the infection.
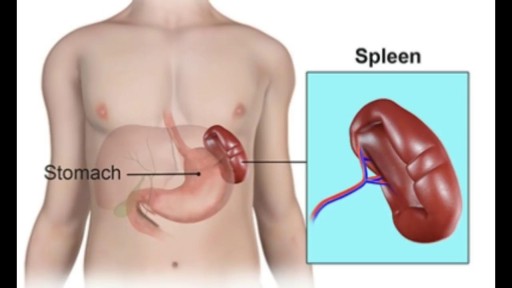
The spleen plays multiple supporting roles in the body. It acts as a filter for blood as part of the immune system. Old red blood cells are recycled in the spleen, and platelets and white blood cells are stored there. The spleen also helps fight certain kinds of bacteria that cause pneumonia and meningitis

Sever's disease (also known as calcaneal apophysitis) is a type of bone injury in which the growth plate in the lower back of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and causes pain.
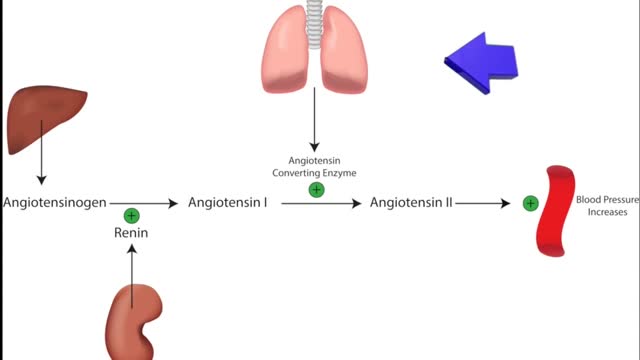
ACE inhibitors Email this page to a friend Print Facebook Twitter Google+ Angiotensin-converting enzyme (ACE) inhibitors are medicines. They treat heart, blood vessel, and kidney problems. How ACE inhibitors help ACE inhibitors are used to treat heart disease. These medicines make your heart work less hard by lowering your blood pressure. This keeps some kinds of heart disease from getting worse. Most people who have heart failure take these medicines. These medicines treat high blood pressure, strokes, or heart attacks. They may help lower your risk for stroke or heart attack. They are also used to treat diabetes and kidney problems. This can help keep your kidneys from getting worse. If you have these problems, ask your health care provider if you should be taking these medicines.

Endometriosis (en-doe-me-tree-O-sis) is an often painful disorder in which tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. Endometriosis most commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.

Skin Whitening Tips, Vitamin C For Skin Whitening, Skin Whitening Before And After, Skin Whitening. http://skin-whitening.good-info.co Each and every person wants a clean and radiant skin. Some spend fortunes on cosmetic products that will lighten the skin and remove all the imperfections, others spend their money on esthetic operations in the hope that their skin will look perfect. Lastly, there are people trying to fake a healthy skin by using all kinds of makeup that will cover the imperfections and leave the impression that the skin is healthy and has no scars, wrinkles or spots. All these people are looking for a way through which they can make their skin look good. Yet, what they have not taken into consideration is the power of natural ingredients. Fruits, vegetables and products coming from animals are great sources of anti-oxidants and are rich in substances which can whiten the skin, moisturize it, attenuate the fine lines and wrinkles and give it elasticity. There are many natural ingredients which can be used in order to remove the dark spots and whiten the skin and as many reasons to start trying them. The first reason for which you should try the natural skin whitening ingredients is the fact that they have no side effects. Because most of the ingredients with which the homemade skin whitening recipes are made are natural, and are used in our everyday diet, the human body tolerates them very well and responds positively to the ingredients they contain. In addition to that, because you know what you put in that homemade recipe, you know if your skin will going to react negatively to it. There are certain products (fruits, vegetables, animal products) to which certain people are allergic. Exclude those ingredients from your recipes and you know you will obtain a 100% safe homemade product. Click Here. http://skin-whitening.good-info.co
Appareil Pour La Cellulite, Creme Anti Cellulite Efficace, Anti Cellulite Maison, Café Cellulite--- http://perdre-sa-cellulite.plus101.com --- Cellulite Des Cuisses, Que Faire? Comment Eliminer Vite Sa Cellulite Des Cuisses Avec Des Exercices et L'alimentation cellulite-cuissesMême si la plupart des gens se mettent continuellement à la chasse de la cellulite, jusqu’à ce jour, il n’y a pas encore eu de remèdes miracles. Elle est particulièrement causée par le manque d’activités physiques et une alimentation non équilibrée. Elle apparaît souvent sur les fesses, les hanches et principalement sur les cuisses. Ainsi, pour se débarrasser de la cellulite surtout celle des cuisses, il est important d’avoir une alimentation équilibrée et de pratiquer des exercices sportifs. Il vous suffit de suivre les recommandations dans la vidéo ci-dessous qui vous aideront à tonifier vos jambes de manière efficaces, ainsi réduisant la présence de la cellulite sur les fesses, hanches et cuisses pour une silhouette plus attirante.CLIQUEZ ICI: http://perdre-sa-cellulite.plus101.com

A visual prosthesis, often referred to as a bionic eye, is an experimental visual device intended to restore functional vision in those suffering from partial or total blindness. In 1983 Joao Lobo Antunes, a Portuguese doctor, implanted a bionic eye in a person born blind.
all pregnant women be screened for Chlamydia at the first prenatal visit. Women under age 25 and those at increased risk for chlamydia! Infection should have repeat testing in the third trimester. Chlamydia endometritis during pregnancy can lead to chorioamnionitis and premature delivery of the fetus. Untreated infection during pregnancy can also lead to conjunctivitis (ophthalmia neonatorum) and pneumonia in the newborn baby

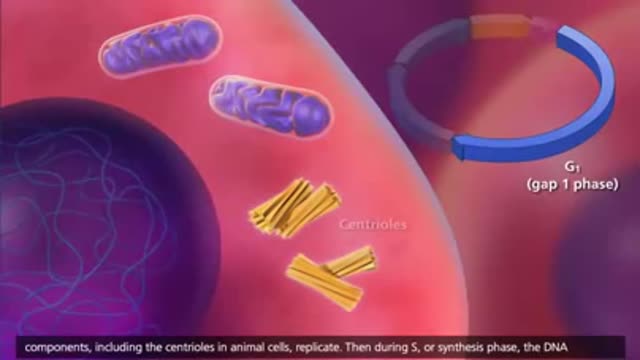
Mitosis is the process in which a eukaryotic cell nucleus splits in two, followed by division of the parent cell into two daughter cells. The word "mitosis" means "threads," and it refers to the threadlike appearance of chromosomes as the cell prepares to divide.