Top videos

Unstable ankle joints after internal fixation of type B malleolar fractures exist. Residual instability most often occurs after trimalleolar fractures with initial joint dislocation. Treatment with an additional positioning screw generally produced a satisfactory result.

Surfactant. Surfactants are compounds that lower the surface tension (or interfacial tension) between two liquids or between a liquid and a solid. Surfactants may act as detergents, wetting agents, emulsifiers, foaming agents, and dispersants.

Sever's disease (also known as calcaneal apophysitis) is a type of bone injury in which the growth plate in the lower back of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and causes pain.

Skin Whitening Tips, Vitamin C For Skin Whitening, Skin Whitening Before And After, Skin Whitening. http://skin-whitening.good-info.co Each and every person wants a clean and radiant skin. Some spend fortunes on cosmetic products that will lighten the skin and remove all the imperfections, others spend their money on esthetic operations in the hope that their skin will look perfect. Lastly, there are people trying to fake a healthy skin by using all kinds of makeup that will cover the imperfections and leave the impression that the skin is healthy and has no scars, wrinkles or spots. All these people are looking for a way through which they can make their skin look good. Yet, what they have not taken into consideration is the power of natural ingredients. Fruits, vegetables and products coming from animals are great sources of anti-oxidants and are rich in substances which can whiten the skin, moisturize it, attenuate the fine lines and wrinkles and give it elasticity. There are many natural ingredients which can be used in order to remove the dark spots and whiten the skin and as many reasons to start trying them. The first reason for which you should try the natural skin whitening ingredients is the fact that they have no side effects. Because most of the ingredients with which the homemade skin whitening recipes are made are natural, and are used in our everyday diet, the human body tolerates them very well and responds positively to the ingredients they contain. In addition to that, because you know what you put in that homemade recipe, you know if your skin will going to react negatively to it. There are certain products (fruits, vegetables, animal products) to which certain people are allergic. Exclude those ingredients from your recipes and you know you will obtain a 100% safe homemade product. Click Here. http://skin-whitening.good-info.co
http://vitiligo-home-remedies.plus101.com ---- white spots on skin, small white spots on face, what causes white spots on skin, vitiligo. The Link Between Vitiligo and Auto Immune Disorders. If you suffer with Vitiligo, a condition that strips your skin of its natural pigment or coloring, the odds are good that you are also battling some sort of autoimmune disorder. It took years for doctors to connect the two disorders, but recent research shows that at least 20 percent of Vitiligo suffers also get autoimmune thyroid disease, and that's juts the beginning. Many more suffer a multitude of other disorders. Until recently, the link between the Vitiligo and autoimmune problems were not clear. Doctors seemed to see a link, but nothing substantial could be proven. Until now. In march 2013, The National Institute's of Health's National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) announced an amazing discovery: a connection between a specific gene named NALP1, Vitiligo and a host of autoimmune diseases including thyroid disease, pernicious anemia, rheumatoid arthritis, lupus and Addison's Disease. According to lead researcher, Richard Spritz M.D., the discovery of this gene may make newer, more effective Vitiligo treatments possible within the next few years. But that's not all. It will also be able to help treat certain auto immune disorders. By finding ways to block the inflammatory response of the NALP1 gene, doctors may some day be able to cure certain autoimmune disorders. A long-term solution for vitiligo should address the internal causes of vitiligo by tackling all vitiligo contributing factors. Only by controlling the nutritional, hormonal, psychological and environmental triggers of vitiligo, using a multidimensional and holistic approach to healing you can reverse the "internal vitiligo environment"- the only, safe, natural and effective way you could ever achieve lasting vitiligo freedom. More Info: http://vitiligo-home-remedies.plus101.com
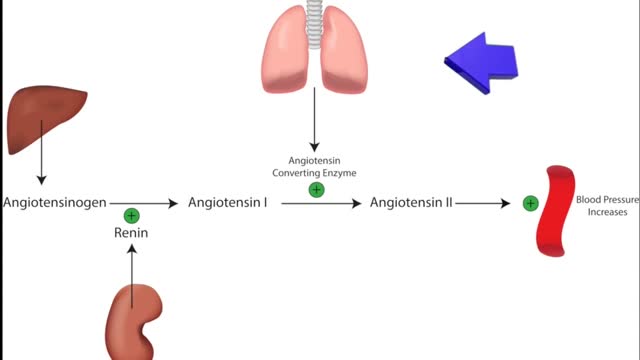
ACE inhibitors Email this page to a friend Print Facebook Twitter Google+ Angiotensin-converting enzyme (ACE) inhibitors are medicines. They treat heart, blood vessel, and kidney problems. How ACE inhibitors help ACE inhibitors are used to treat heart disease. These medicines make your heart work less hard by lowering your blood pressure. This keeps some kinds of heart disease from getting worse. Most people who have heart failure take these medicines. These medicines treat high blood pressure, strokes, or heart attacks. They may help lower your risk for stroke or heart attack. They are also used to treat diabetes and kidney problems. This can help keep your kidneys from getting worse. If you have these problems, ask your health care provider if you should be taking these medicines.
Appareil Pour La Cellulite, Creme Anti Cellulite Efficace, Anti Cellulite Maison, Café Cellulite--- http://perdre-sa-cellulite.plus101.com --- Cellulite Des Cuisses, Que Faire? Comment Eliminer Vite Sa Cellulite Des Cuisses Avec Des Exercices et L'alimentation cellulite-cuissesMême si la plupart des gens se mettent continuellement à la chasse de la cellulite, jusqu’à ce jour, il n’y a pas encore eu de remèdes miracles. Elle est particulièrement causée par le manque d’activités physiques et une alimentation non équilibrée. Elle apparaît souvent sur les fesses, les hanches et principalement sur les cuisses. Ainsi, pour se débarrasser de la cellulite surtout celle des cuisses, il est important d’avoir une alimentation équilibrée et de pratiquer des exercices sportifs. Il vous suffit de suivre les recommandations dans la vidéo ci-dessous qui vous aideront à tonifier vos jambes de manière efficaces, ainsi réduisant la présence de la cellulite sur les fesses, hanches et cuisses pour une silhouette plus attirante.CLIQUEZ ICI: http://perdre-sa-cellulite.plus101.com

Endometriosis (en-doe-me-tree-O-sis) is an often painful disorder in which tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. Endometriosis most commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.

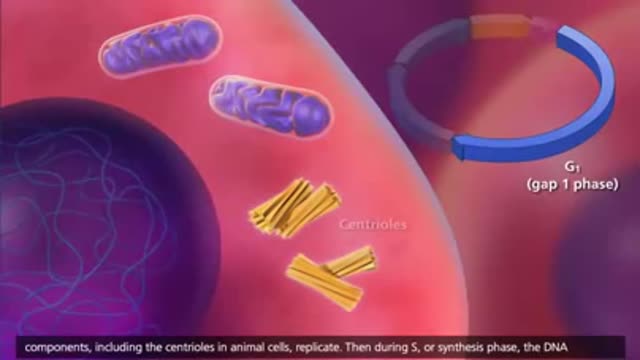
Mitosis is the process in which a eukaryotic cell nucleus splits in two, followed by division of the parent cell into two daughter cells. The word "mitosis" means "threads," and it refers to the threadlike appearance of chromosomes as the cell prepares to divide.

Experts do not know the exact cause of Zollinger-Ellison syndrome. About 25 to 30 percent of gastrinomas are caused by an inherited genetic disorder called multiple endocrine neoplasia type 1 (MEN1). MEN1 causes hormone-releasing tumors in the endocrine glands and the duodenum.
A febrile seizure is a convulsion in a child that may be caused by a spike in body temperature, often from an infection. Your child's having a febrile seizure can be alarming, and the few minutes it lasts can seem like an eternity. Febrile seizures represent a unique response of a child's brain to fever, usually the first day of a fever. Fortunately, they're usually harmless and typically don't indicate an ongoing problem. You can help by keeping your child safe during a febrile seizure and by comforting him or her afterward.