Top videos

For a full Surgical Airway Techniques resource: https://bit.ly/2rb9Nud
Video courtesy of Gauri Mankekar, MBBS, MS, PhD

OB_A_1013
3D animation depicting the operating room and initial procedure preparing the patient for a laparoscopic hysterectomy. The patient is prepped and draped in the usual fashion and surrounded by the surgeon and surgical assistants. The skin is elevated, an infraumbilical incision is made, a trocar port is inserted through the incision and the abdomen is insufflated. Finally, a laparoscope is inserted into the port to allow for direct visualization of the uterus and the surgery can begin.
To view more animations and exhibits, visit our medical library: https://www.trialexhibitsinc.c....om/library/multimedi
Contact us on your next case for consulting, trial graphics, animations, medical illustrations or presentation services. 800-591-1123 [a]www.trialex.com[/a]
This video is for reference only. The video may not be otherwise used, reproduced nor modified. For more information to purchase a copy or permission to use this animation on your next case, project, website or TV, contact us at [a]www.trialex.com[/a] or 800-591-1123.
Copyright @ Trial Exhibits, Inc.

Eric knew he needed help when an old knee injury began worsening over the course of time and was significantly affecting his quality of life. That’s when he turned to his hometown orthopedic experts at Mayo Clinic Health System in Mankato, who recommended a total knee replacement. After overcoming some initial fears, Eric decided it was time to have the operation — a fuller and more active life with his family depended on it.
Caesarean section is the most common way to deliver a breech baby in the USA, Australia, and Great Britain. Like any major surgery, it involves risks. Maternal mortality is increased by a Caesarean section, but still remains a rare complication in the First World. Third World statistics are dramatically different, and mortality is increased significantly. There is remote risk of injury to the mother’s internal organs, injury to the baby, and severe hemorrhage requiring hysterectomy with resultant infertility. More commonly seen are problems with noncatastrophic bleeding, postoperative infection and wound healing problems. It should be added that the increase in maternal mortality rates could be slightly skewed due to the fact that Caesarean sections are often used during high-risk pregnancies and/or when mortality is already a strong possibility.
One large study has confirmed that elective cesarean section has lower risk to the fetus and a slightly increased risk to the mother, than planned vaginal delivery of the breech however elements of the methodology used have undergone some criticism.
The same birth injuries that can occur in vaginal breech birth may rarely occur in Caesarean breech delivery. A Caesarean breech delivery is still a breech delivery. However the soft tissues of the uterus and abdominal wall are more forgiving of breech delivery than the hard bony ring of the pelvis. If a Caesarean is scheduled in advance (rather than waiting for the onset of labor) there is a risk of accidentally delivering the baby too early, so that the baby might have complications of prematurity. The mother’s subsequent pregnancies will be riskier than they would be after a vaginal birth (uterine rupture). The presence of a uterine scar will be a risk factor for any subsequent pregnancies.

A Pap smear (Papanicolau smear; also known as the Pap test) is a screening test for cervical cancer. The test itself involves collection of a sample of cells from a woman's cervix (the end of the uterus that extends into the vagina) during a routine pelvic exam
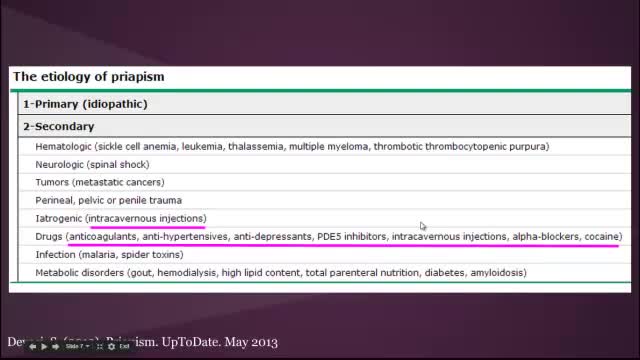
Priapism is a prolonged erection of the penis. The persistent erection continues hours beyond or isn't caused by sexual stimulation. Priapism is usually painful. Although priapism is an uncommon condition overall, it occurs commonly in certain groups, such as people who have sickle cell anemia. Prompt treatment for priapism is usually needed to prevent tissue damage that could result in the inability to get or maintain an erection (erectile dysfunction). Priapism is most common in men in their 30s.

http://www.nucleushealth.com/ - This 3D medical animation shows the cause and laparoscopic treatment of a ventral incisional hernia. If you have had abdominal surgery in the past, a ventral incisional hernia may appear at the site of your surgical scar. Your intestine may push through a weakened spot in the tissue between your abdominal muscles creating a bulge beneath your skin. If your hernia is not repaired, complications may occur.
#VentralHernia #VentralIncisionalHernia #IncisionalHernia
ANH11053
Mysterious massage from East Asia(CHINA).it can cure cure Erectile dysfunction,can let their life better.This video from mainland of China,so the language is Chinese mandarin.but you can see English show on the video too.Tiedang gong means kongfu of Iron penis&balls.

Orthopedic spine surgeons and vascular surgeons at UW Health in Madison, WI work together to perform minimally invasive anterior lumbar interbody fusion (Mini-ALIF). With this type of spinal fusion surgery, patients have smaller incisions, usually spend less time in the hospital and typically return to daily activities more quickly. Learn more https://www.uwhealth.org/ALIF