Top videos

This video demonstrates how to perform an abdominal examination in an OSCE station.
You can access our step-by-step OSCE guide to accompany this video here: https://geekymedics.com/abdominal-examination/
Check out our other awesome clinical skills resources including:
• 🔥 Geeky Medics Bundles (discounted products): https://app.geekymedics.com/purchase/bundles/
• ✨ 1000+ OSCE Stations: https://app.geekymedics.com/pu....rchase/osce-stations
• 🏥 Geeky Medics OSCE Revision Book: https://app.geekymedics.com/purchase/book/
• 📝 150+ PDF OSCE Checklists: https://geekymedics.com/pdf-osce-checklists/
• 🗂️ 3000+ OSCE Flashcards: https://app.geekymedics.com/pu....rchase/flashcard-col
• 📱 Geeky Medics OSCE App: https://geekymedics.com/geeky-medics-app/
• 🩺 Medical Finals SBA Question Pack: https://app.geekymedics.com/pu....rchase/medical-stude
• 💊 PSA Question Pack: https://app.geekymedics.com/pu....rchase/prescribing-s
Chapters:
- Introduction 00:00
- General inspection 00:35
- Hands 00:47
- Asterixis 01:20
- Arms and axilla 01:32
- Face, eyes & mouth 01:45
- Lymph node palpation 02:19
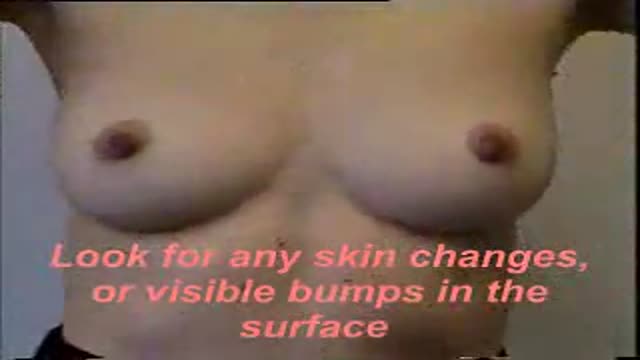
- Chest inspection 02:50
- Inspection of abdomen 03:02
- Palpation of abdomen 03:34
- Percussion of abdomen 05:36
- Shifting dullness 06:30
- Auscultation of abdomen 06:55
- Summary 07:29
Subscribe to our newsletter to be the first to know about our latest content: https://geekymedics.com/newsletter/ ✉️
Join the Geeky Medics community: 👩👩👧👧
Twitter: http://www.twitter.com/geekymedics
Instagram: https://instagram.com/geekymedics
Facebook: http://www.facebook.com/geekymedics
Always adhere to your medical school/local hospital guidelines when performing examinations or clinical procedures. DO NOT perform any examination or procedure on patients based purely upon the content of these videos. Geeky Medics accepts no liability for loss of any kind incurred as a result of reliance upon the information provided in this video.
Some people have found this video useful for ASMR purposes.
Wernicke's aphasia is a neurological disorder typically caused by stroke. It affects the Wernicke's region in the brain's left hemisphere which is reasoned to be responsible for processing of meaning, especially as it relates to verbal communication, hence the problems with speech witnessed in these patients

Mysterious massage from East Asia(CHINA).it can cure cure Erectile dysfunction,can let their life better.This video from mainland of China,so the language is Chinese mandarin.but you can see English show on the video too.Tiedang gong means kongfu of Iron penis&balls.

www.diabetes.org > Living With Diabetes > Treatment and Care > Medication > Insulin & Other Injectables Share: Print PageText Size:A A A Listen How Do Insulin Pumps Work? If you have been diagnosed with diabetes, you may feel overwhelmed by all the new information you have learned and will continue to learn about managing your diabetes. You already know your main goal should be to get your blood glucose (sugar) levels under control in order to increase your chances of a complication-free life. Many people know this, but need to know how to achieve good diabetes management, while balancing the day-to-day demands of diabetes with other life demands. An insulin pump can help you manage your diabetes. By using an insulin pump, you can match your insulin to your lifestyle, rather than getting an insulin injection and matching your life to how the insulin is working. When you work closely with your diabetes care team, insulin pumps can help you keep your blood glucose levels within your target ranges. People of all ages with type 1 diabetes use insulin pumps and people with type 2 diabetes have started to use them as well. - See more at: http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/insulin/how-do-insulin-pumps-work.html?referrer=https://www.google.com/#sthash.XD56v351.dpuf

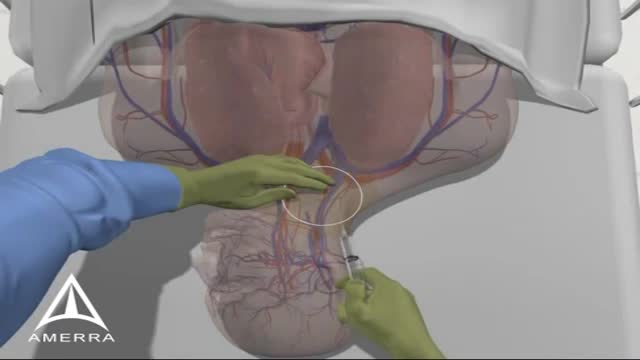
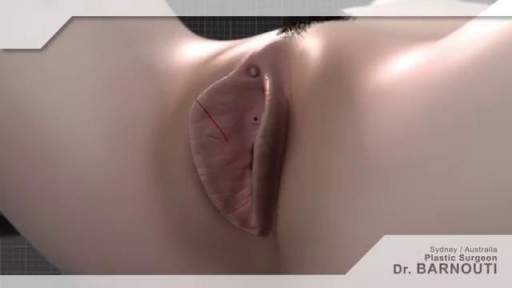
Inguinal or groin hernias are the most common type of hernias and most of the time occur in men. We talked with CU Medicine surgeon, Dr. Sam Phinney, about groin hernias and how they are treated. https://www.cumedicine.us/abou....t-cu-medicine/health

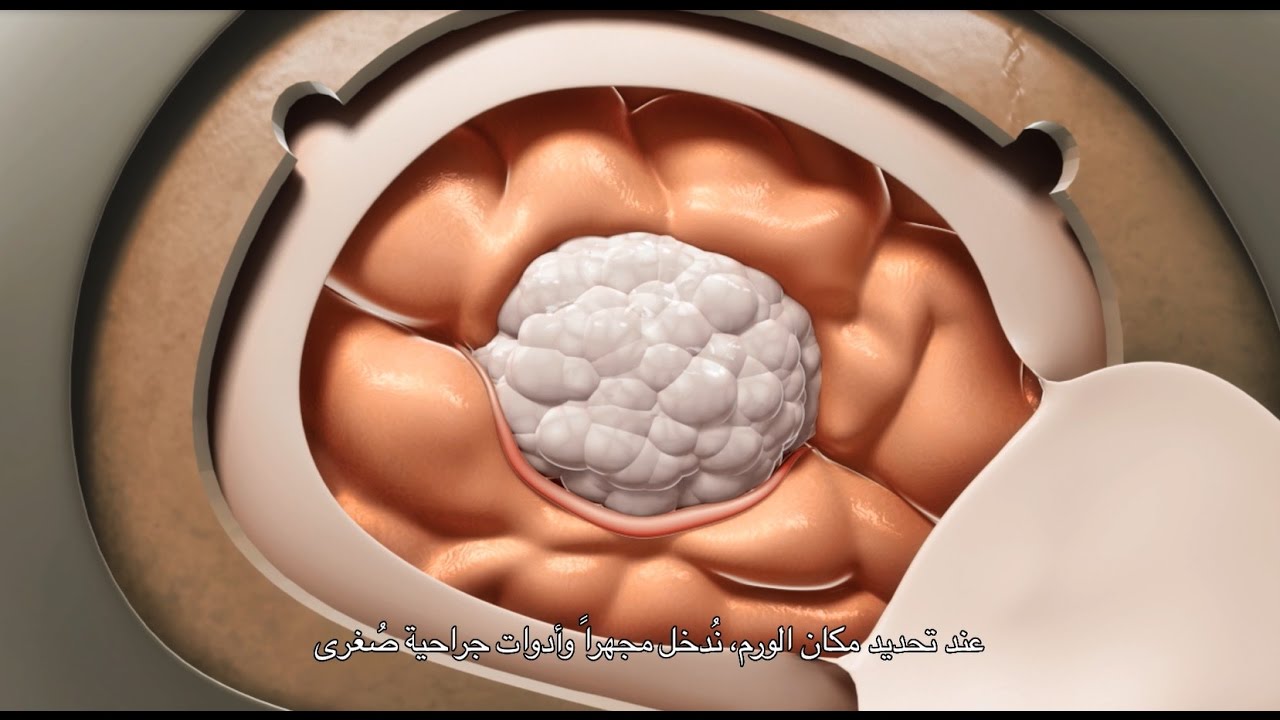
Bone tumors include abnormal healing of an injury, inherited conditions, radiation therapy. It can also be caused by bone cancer or another cancer that has spread to the bone from other parts of the body. A bone tumor may cause a painless mass. Some people have dull, aching pain. And in some cases, minor injury causes a fracture near the tumor. Treatments include surgery and radiation. Some noncancerous tumors go away without treatment