Top videos

Ganglion cysts are noncancerous lumps that most commonly develop along the tendons or joints of your wrists or hands. They also may occur in the ankles and feet. Ganglion cysts are typically round or oval and are filled with a jellylike fluid. Small ganglion cysts can be pea-sized, while larger ones can be around an inch (2.5 centimeters) in diameter. Ganglion cysts can be painful if they press on a nearby nerve. Their location can sometimes interfere with joint movement. If your ganglion cyst is causing you problems, your doctor may suggest trying to drain the cyst with a needle. Removing the cyst surgically also is an option. But if you have no symptoms, no treatment is necessary. In many cases, the cysts go away on their own.
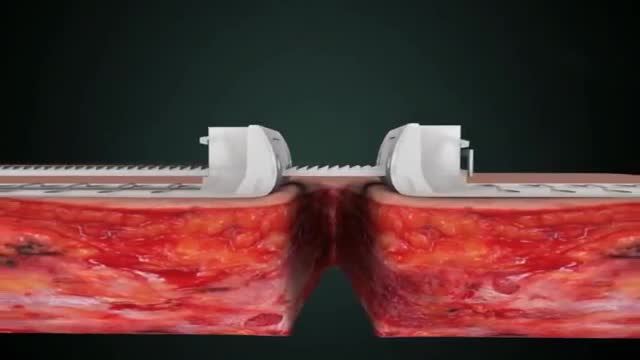
Wound closure techniques have evolved from the earliest development of suturing materials to comprise resources that include synthetic sutures, absorbables, staples, tapes, and adhesive compounds. The engineering of sutures in synthetic material along with standardization of traditional materials (eg, catgut, silk) has made for superior aesthetic results. Similarly, the creation of topical skin adhesives (the monomer 2-octyl cyanoacrylate), surgical staples, and tapes to substitute for sutures has supplemented the armamentarium of wound closure techniques. Aesthetic closure of a wound, whether traumatic or surgically induced, is based on knowledge of healing mechanisms and skin anatomy (see the image below), as well as an appreciation of suture material and closure technique. Choosing the proper materials and wound closure technique ensures optimal healing.[1]

Factitious disorder is the term used to describe a pattern of behavior centered on the exaggeration or outright falsifications of one’s own health problems or the health problems of others. Some people with this disorder fake or exaggerate physical problems; others fake or exaggerate psychological problems or a combination of physical and psychological problems. Factitious disorder differs from a pattern of falsified or exaggerated behavior called malingering. While malingerers make their claims out of a motivation for personal gain, people with factitious disorder have no such motivation.

The shoulder and arm receives its nerve supply through the brachial plexus. The brachial plexus is a complex network of nerves which come out of the neck, passes down to the front of the shoulder and then splits into many separate nerves to travel to different muscles and parts of the skin. Normally an arm movement is produced by initially thinking of the movement, then a message passes from the brain, down through the spinal cord to the appropriate nerve. Then the instruction to move is conveyed along the nerve to the specific arm muscle which then contracts and moves the arm.
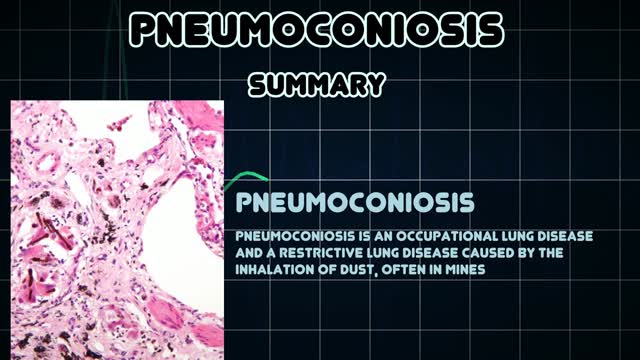
Pneumoconiosis is a general term given to any lung disease caused by dusts that are breathed in and then deposited deep in the lungs causing damage. Pneumoconiosis is usually considered an occupational lung disease, and includes asbestosis, silicosis and coal workers' pneumoconiosis (CWP), also known as "Black Lung Disease."

Sclerotherapy is a procedure used to eliminate varicose veins and spider veins. Sclerotherapy involves an injection of a solution (generally a salt solution) directly into the vein. The solution irritates the lining of the blood vessel, causing it to collapse and stick together and the blood to clot.Sep 17, 2016
Like the VenaCure EVLT® procedure, which uses a laser to ablate the varicose vein, VNUS RF treatment is an alternative to more invasive leg stripping surgery. It is used primarily to treat the great saphenous veins (GSV), small saphenous vein (SSV), and other superficial veins in the legs.

Pyogenic liver abscesses are mainly treated by percutaneous aspiration or drainage under antibiotic cover. If interventional radiology fails, surgical drainage becomes necessary. Recently, we performed laparoscopic liver abscess drainage successfully, and we aimed to focus on the topic in light of a systematic review of the literature.

Menstruation is a woman's monthly bleeding. When you menstruate, your body sheds the lining of the uterus (womb). Menstrual blood flows from the uterus through the small opening in the cervix and passes out of the body through the vagina. Most menstrual periods last from 3 to 5 days.
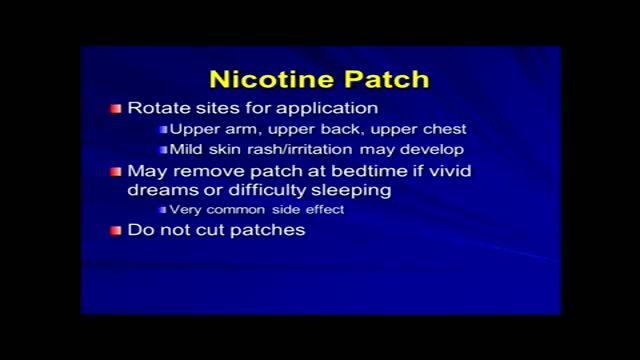
Tobacco use is the most common preventable cause of death. About half of the people who don't quit smoking will die of smoking-related problems. Quitting smoking is important for your health. Soon after you quit, your circulation begins to improve, and your blood pressure starts to return to normal. Your sense of smell and taste return, and it's easier for you to breathe. In the long term, giving up tobacco can help you live longer. Your risk of getting cancer decreases with each year you stay smoke-free. Quitting is not easy. You may have short-term affects such as weight gain, irritability, and anxiety. Some people try several times before they succeed. There are many ways to quit smoking. Some people stop "cold turkey." Others benefit from step-by-step manuals, counseling, or medicines or products that help reduce nicotine addiction. Some people think that switching to e-cigarettes can help you quit smoking, but that has not been proven. Your health care provider can help you find the best way for you to quit.

A torn meniscus is one of the most common knee injuries. Any activity that causes you to forcefully twist or rotate your knee, especially when putting your full weight on it, can lead to a torn meniscus. Each of your knees has two menisci — C-shaped pieces of cartilage that act like a cushion between your shinbone and your thighbone. A torn meniscus causes pain, swelling and stiffness. You also might feel a block to knee motion and have trouble extending your knee fully. Conservative treatment — such as rest, ice and medication — is sometimes enough to relieve the pain of a torn meniscus and give the injury time to heal on its own. In other cases, however, a torn meniscus requires surgical repair.

An unnamed Russian scientist has introduced the concept of a device that attaches to the wall of the artery. It would first stop blood flow to the area to prevent breakaway plaque. A drill would then scrape the plaque from the artery wall. The procedure of treating plaque buildup could include bypass surgery, stent replacement and balloon angioplasty. Since the plaques are of different types and locations in the body, the inventor proposed using different types of cutting mills.
Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism. The liver carries out several necessary functions, including detoxifying harmful substances in your body, cleaning your blood and making vital nutrients. Cirrhosis occurs in response to damage to your liver. Each time your liver is injured, it tries to repair itself. In the process, scar tissue forms. As cirrhosis progresses, more and more scar tissue forms, making it difficult for the liver to function. Decompensated cirrhosis is the term used to describe the development of specific complications resulting from the changes brought on by cirrhosis. Decompensated cirrhosis is life-threatening. The liver damage done by cirrhosis generally can't be undone. But if liver cirrhosis is diagnosed early and the cause is treated, further damage can be limited and, rarely, reversed.

What is the spleen and what causes an enlarged spleen (splenomegaly)? The spleen sits under your rib cage in the upper left part of your abdomen toward your back. It is an organ that is part of the lymph system and works as a drainage network that defends your body against infection. White blood cells produced in the spleen engulf bacteria, dead tissue, and foreign matter, removing them from the blood as blood passes through it. The spleen also maintains healthy red and white blood cells and platelets; platelets help your blood clot. The spleen filters blood, removing abnormal blood cells from the bloodstream. A spleen is normally about the size of your fist. A doctor usually can't feel it during an exam. But diseases can cause it to swell and become many times its normal size. Because the spleen is involved in many functions, many conditions may affect it.
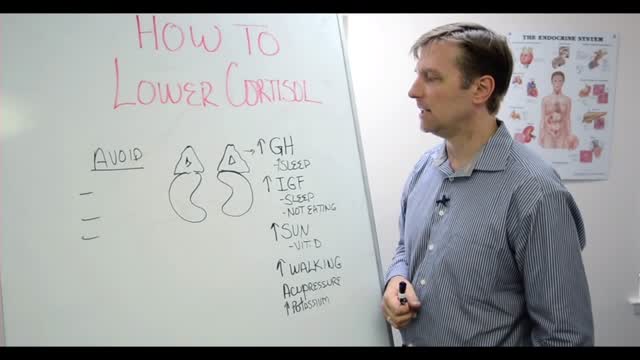
Assuming you haven't been diagnosed with Cushing's disease by your doctor, here are steps you can take to help lower high cortisol levels naturally: Switch to a Whole Foods, Anti-inflammatory Diet. Reduce and Manage Stress. Exercise Regularly. Use Adaptogen Herbs and Superfoods. Try Essential Oils to Promote Relaxation.