Top videos

#HerniaRepair #HerniaSurgery #LaparoscopicHerniaRepair #OpenHerniaRepair #InguinalHernia #UmbilicalHernia #VentralHernia #MeshRepair #HerniaRecovery #HerniaComplications
hernia operation
hernia treatment
hernia
hernia treatment at home
hernia operation and recovery
hernia surgery and recovery
terapi hernia
inguinal hernia treatment without surgery
harnia
hernia surgery
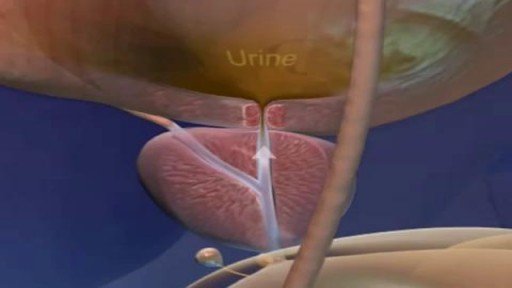
hernia surgery animation
harniya operation
hernia symptoms men
harniya
hernia ka ilaj
hernia laparoscopic surgery animation
abdominal hernia treatment without sur...
hernia symptoms
turun berok
abdominal hernia
hernia exercises without surgery
hernia operation in 3d animation
inguinal hernia surgery
umbilical hernia symptoms and treatment
harnia operation
harniya ka ilaj
hernia animation
hernia belt
hernias
how to treat hernia without surgery
inguinal hernia recovery after surgery
ngiri
open hernia surgery
skates
turun bero
3d surgery
after hernia surgery recovery
appam kaise banate hain
hernia belt for men
hernia belt how to use
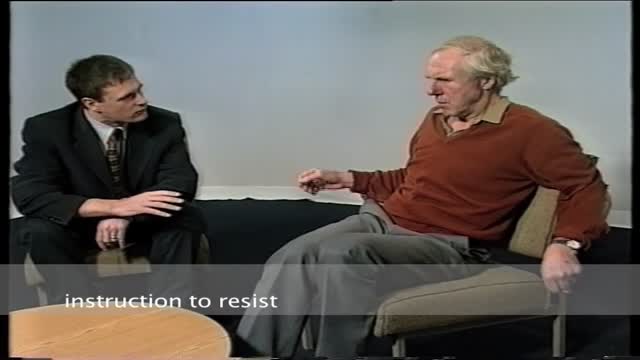
hernia exam
hernia inguinal sintomas
hernia ka operation kaisa hota hai
hernia operation ke baad exercise
hernia operation video
hernia repair
hernia repair mesh complications
hernia repair surgery animation
hernia surgery recovery tips
hernie abdominale
herniya

Dr. Horacio Asbun, Mayo Clinic in Florida, explains the Whipple procedure using this animated graphic of a pancreas. Cancer of the pancreas affects 45,000 people every year in the U.S., and it is the fourth leading cause of cancer-related deaths. The five-year overall survival rate if a tumor is detected early and surgically removed is 22 percent, versus 6 percent without early detection and surgery. To learn more, visit http://mayocl.in/2zk7FDi.
This video in Spanish/español: https://www.youtube.com/watch?v=N_zWboNMKWk

Dr. James Wall performs a bilateral inguinial hernia repair surgical procedure.
Featured:
James Wall, MD
Assistant Professor of Surgery, Pediatric Surgery
Assistant Professor of Bioengineering (By Courtesy)
Lucile Salter Packard Children's Hospital
Micaela Esquivel, MD
Chief Resident of General Surgery

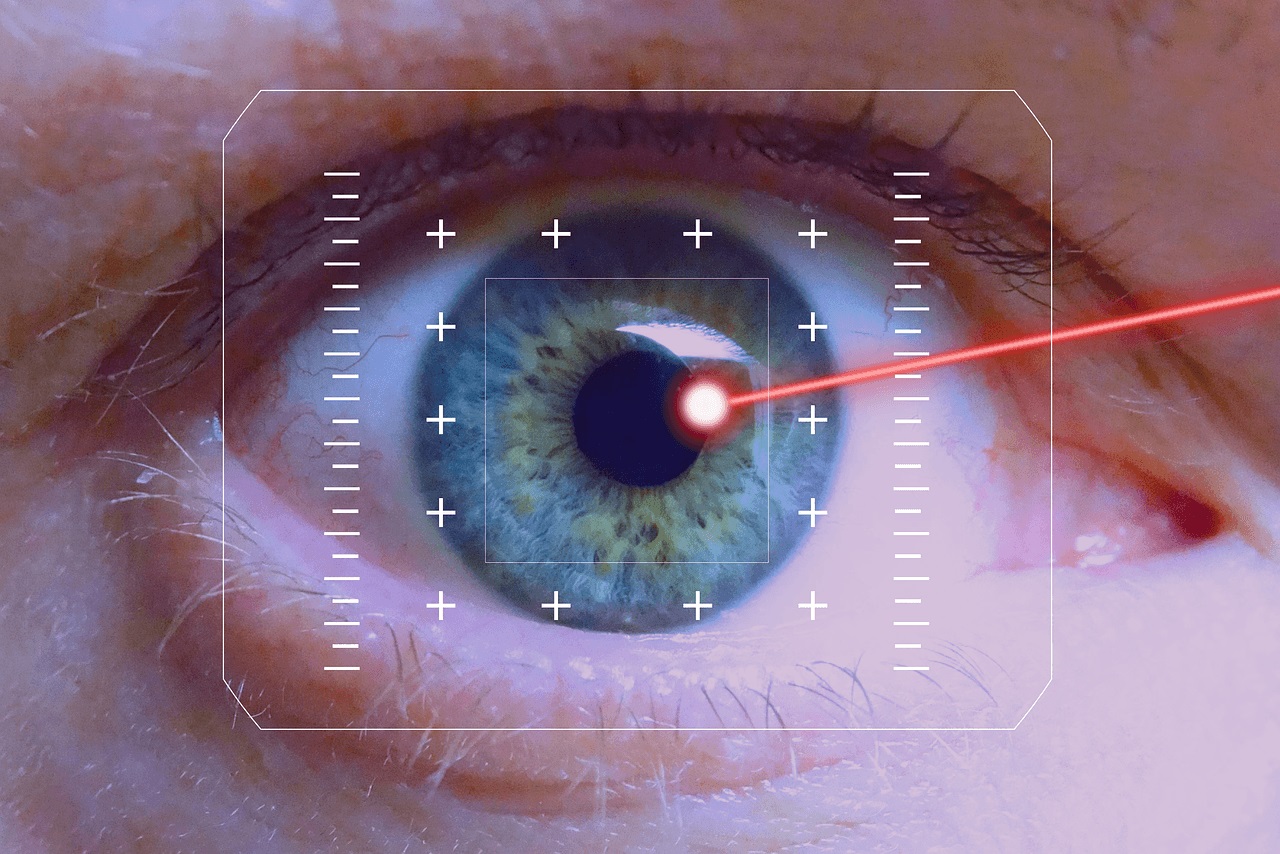
Retinitis pigmentosa is a rare, inherited degenerative eye disease that causes severe vision impairment. Symptoms often begin in childhood. They include decreased vision at night or in low light and loss of side vision (tunnel vision).

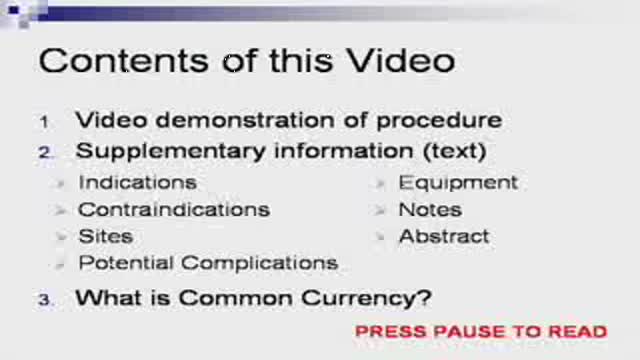
Please remember that this video is to be used for educational purposes. You must follow your facility or colleges' policies and procedure checklists to ensure you are completing the skill satisfactorily. Thanks for watching!
Music from #Uppbeat (free for Creators!):
https://uppbeat.io/t/swoop/blue-sea
License code: W9DFUQ4II7YVHA59

Pass your tests and improve your grades with the below FREE resources:
1) A FREE 140 Must Know Meds book
Click here to get your FREE copy of the 140 Must Know Meds Book: https://bit.ly/41rxSt0
2) A FREE test-taking tips webinar
Join us for our free test-taking tips webinar to boost your exam scores: https://bit.ly/nursingtesttaking
You can now test your knowledge with a free lesson quiz on NURSING.com!
Click here for your free quiz: https://bit.ly/3uyTWEu
Learn what's working for other Nursing Students! Check out our Top 10 Most Popular Lessons Here: https://bit.ly/3nda5u3
Dressing Changes- Wet to Dry (Nursing Skills)
FREE Nursing School Cheat Sheets at: http://www.NURSING.com
Get the full Dressing Change lesson here: https://nursing.com/lesson/ski....lls-05-04-wound-care
Click here for the related lesson on Wound Assessment: https://nursing.com/lesson/ski....lls-05-02-wound-care
Welcome to the NURSING Family, we call it the most supportive nursing cohort on the planet.
At NURSING.com, we want to help you remove the stress and overwhelm of nursing school so that you can focus on becoming an amazing nurse.
Check out our freebies and learn more at: (http://www.nursing.com)
Dressing Changes- Wet to Dry (Nursing Skills):
In this video we’re going to look at how to do a wet to dry dressing change. Wound care and dressing changes should be performed at least daily or more often depending on orders. Dressing changes should be sterile to avoid introducing any new bacteria to the wound and to promote wound healing.
Bookmarks:
0:05 Introduction
0:10 Wound Assessment link above
0:24 Dressing Change Prep
1:24 Wet vs Dry Gauze
1:37 Soaking Gauze
2:00 Gauze Ring Out
2:25 Packing the wound
3:00 Covering the wound bed
3:37 Dry gauze barrier
4:00 ABD pad application
4:46 Documentation
4:54 Outro
Visit us at https://nursing.com/medical-disclaimer/ for disclaimer information.
NCLEX®, NCLEX-RN® are registered trademarks of the National Council of State Boards of Nursing, INC. and hold no affiliation with NURSING.com.

Shoutout to director/videographer Valentina Vee and producer Sean Tien for helping me bring this to life.
New Comedy Show Dates!
SAN DIEGO, 8/26-8/27
LAS VEGAS, 9/3
HUNTINGTON BEACH, 9/9
WASHINGTON D.C., 10/7-10/8
Get Tickets Here! ----- https://linktr.ee/steveioe
Join the waitlist for Dr. Socko hospital grip socks: https://drsocko.com/
Looking for Blue MuFKR Hoodies? https://mufkr.com/
Find me on
TikTok: https://www.tiktok.com/@steveioe
Instagram: https://www.instagram.com/steveioe
Twitter: https://twitter.com/steveioe
Facebook: https://www.facebook.com/steveioe
P.O. Box:
532308
Los Angeles CA 90053