Top videos

Treatment may not be needed for an eschar if it is part of the natural healing process. However, if an eschar looks like it may have a wound infection – symptoms can include oozing fluid such as pus or blood, your clinician will likely recommend topical treatment or debridement to help control and remove the infection.

Surfactant. Surfactants are compounds that lower the surface tension (or interfacial tension) between two liquids or between a liquid and a solid. Surfactants may act as detergents, wetting agents, emulsifiers, foaming agents, and dispersants.

Sever's disease (also known as calcaneal apophysitis) is a type of bone injury in which the growth plate in the lower back of the heel, where the Achilles tendon (the heel cord that attaches to the growth plate) attaches, becomes inflamed and causes pain.
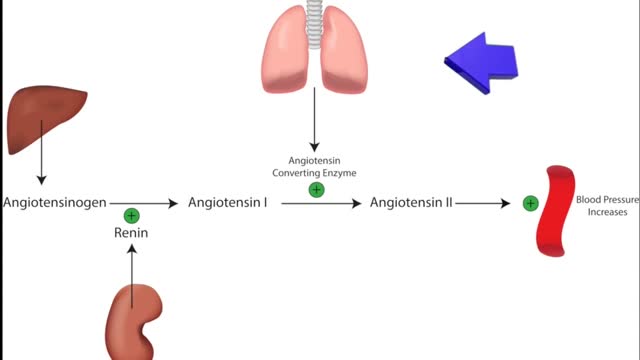
ACE inhibitors Email this page to a friend Print Facebook Twitter Google+ Angiotensin-converting enzyme (ACE) inhibitors are medicines. They treat heart, blood vessel, and kidney problems. How ACE inhibitors help ACE inhibitors are used to treat heart disease. These medicines make your heart work less hard by lowering your blood pressure. This keeps some kinds of heart disease from getting worse. Most people who have heart failure take these medicines. These medicines treat high blood pressure, strokes, or heart attacks. They may help lower your risk for stroke or heart attack. They are also used to treat diabetes and kidney problems. This can help keep your kidneys from getting worse. If you have these problems, ask your health care provider if you should be taking these medicines.

Endometriosis (en-doe-me-tree-O-sis) is an often painful disorder in which tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. Endometriosis most commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.

In breastfeeding, the latch is the moment everything comes together: Your baby takes a big mouthful of your nipple and areola (or "latches on"), begins to suck, and draws out your milk. When your baby has established a good latch, your nipple soreness is minimized and your little one gets the nourishment he needs. How do you pull all that off? First and most important, have faith in yourself and your baby. "Babies are designed to breastfeed," says Emily Pease, R.N., international board certified lactation consultant (IBCLC), of Swedish Hospital's Breastfeeding Center in Seattle. "They are born with instincts that help them find Mom's breast and latch on often with very little assistance. And if problems do come up, there are lots of ways to troubleshoot." Here are more steps to get a good latch right from the start.

Mitosis is the process in which a eukaryotic cell nucleus splits in two, followed by division of the parent cell into two daughter cells. The word "mitosis" means "threads," and it refers to the threadlike appearance of chromosomes as the cell prepares to divide.

Experts do not know the exact cause of Zollinger-Ellison syndrome. About 25 to 30 percent of gastrinomas are caused by an inherited genetic disorder called multiple endocrine neoplasia type 1 (MEN1). MEN1 causes hormone-releasing tumors in the endocrine glands and the duodenum.
A febrile seizure is a convulsion in a child that may be caused by a spike in body temperature, often from an infection. Your child's having a febrile seizure can be alarming, and the few minutes it lasts can seem like an eternity. Febrile seizures represent a unique response of a child's brain to fever, usually the first day of a fever. Fortunately, they're usually harmless and typically don't indicate an ongoing problem. You can help by keeping your child safe during a febrile seizure and by comforting him or her afterward.