Top videos

Here we’ll explain the symptoms of pancreatitis, how alcohol causes the condition and the other health problems it can lead to. You probably don’t pay much attention to your pancreas. But that small, tadpole-shaped organ behind your stomach and below your ribcage is pretty important. It produces two essential substances: digestive juices which your intestines use to break down food, and hormones that are involved in digestion, such as insulin, which regulates your blood sugar levels. Pancreatitis is when your pancreas becomes inflamed and its cells are damaged. Heavy drinking can cause pancreatitis. But if you drink within the government’s low risk unit guidelines, you should avoid upsetting this important organ.
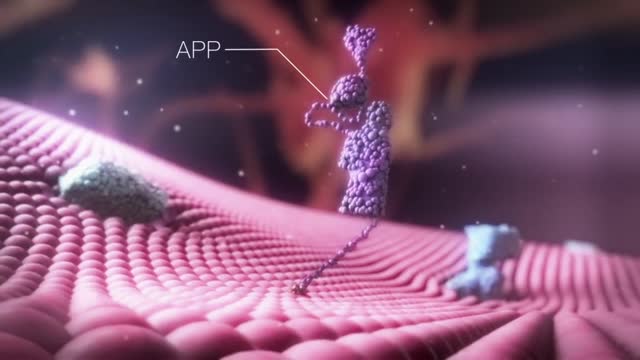
Alzheimer's is the most common form of dementia, a general term for memory loss and other intellectual abilities serious enough to interfere with daily life. Alzheimer's disease accounts for 60 to 80 percent of dementia cases. Alzheimer's is not a normal part of aging, although the greatest known risk factor is increasing age, and the majority of people with Alzheimer's are 65 and older. But Alzheimer's is not just a disease of old age. Up to 5 percent of people with the disease have early onset Alzheimer's (also known as younger-onset), which often appears when someone is in their 40s or 50s.
Magnetic resonance imaging (MRI) can be an important tool in the diagnosis of multiple sclerosis (MS). MRI can also be used to monitor the progression of the disease in people living with MS. How does it work? MRI uses very strong magnets, radio signals, and computer software to take 3-dimensional pictures of the inside of the body. Will I need contrast material? Maybe. Contrast material is a substance that temporarily changes the way imaging tools interact with the body. They are often used to visualize certain types of MS disease activity on the MRI. If your doctor thinks your scan requires this contrast material, you may get an injection before you get in the MRI machine. How long will it take? The time may vary based on the type of MRI. Be sure to discuss with your doctor in advance so he or she can provide you with exact timing. But don’t worry, you won’t have to stay still the whole time. The technician will let you know when they’re starting a new image.

Focal seizures (also called partial seizures [citation needed] and localized seizures) are seizures which affect initially only one hemisphere of the brain. [citation needed] The brain is divided into two hemispheres, each consisting of four lobes – the frontal, temporal, parietal and occipital lobes.

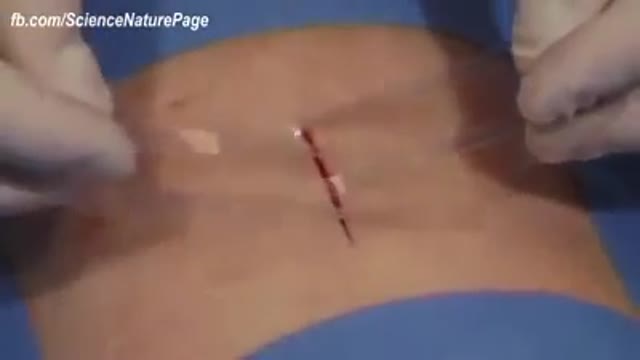
A pneumothorax is usually caused by an injury to the chest, such as a broken rib or puncture wound. It may also occur suddenly without an injury. A pneumothorax can result from damage to the lungs caused by conditions such as chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, and pneumonia.

There are several things to consider when trying to decide between gastric bypass surgery and gastric sleeve surgery. Unlike the laparoscopic adjustable gastric band (Lap Band), these two operations are both permanent, reduce hunger, and lead to the highest percentage of weight loss. To properly compare gastric sleeve surgery to gastric bypass surgery we will examine the following data : Expected weight loss. Speed of weight loss. Time of surgery. Gastric bypass benefits over sleeve. Gastric sleeve benefits over bypass. Risk of complications. Surgeon skill and preference.

The obstetric examination is distinct from other examinations in that you, the clinician, are trying to assess the health of two individuals – the mother and the fetus – simultaneously. From the initial history, you should be able to judge the health of the pregnancy, any risk factors that need to be addressed, and any concerns from the parents. The history is an opportunity for you to find out how much the parents know about pregnancy, labour and delivery and if they have any preferences to which these events are carried out. A carefully taken history will also direct your attention to specific signs during the examination. As such, it is important that you develop a concise and systematic method of taking the history and carrying out the examination so that you do not miss any important information. This article focuses primarily on the examination. Pregnancy is a sensitive issue, especially for the primigravida’s. Therefore, extra care is needed when you approach a pregnant woman. Always obtain expressed informed consent before examining her and have a chaperone accompany you throughout the examination. A walk-through of what you will be doing is a good way of reassuring the patient and allows the examination to go on smoothly. It is also important to let your patient know that if the examination is too painful, she can stop at any time she wants. Finally, before you begin, you should always wash your hands, especially at an OSCE station.
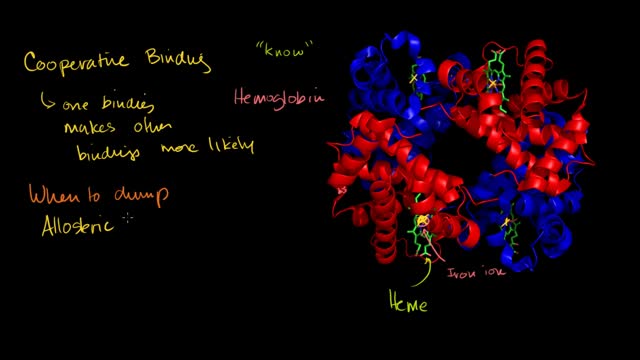
Hemoglobin is the protein molecule in red blood cells that carries oxygen from the lungs to the body's tissues and returns carbon dioxide from the tissues back to the lungs. Hemoglobin is made up of four protein molecules (globulin chains) that are connected together.

Rotator cuff pain commonly causes local swelling and tenderness in the front of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position. Beginning symptoms may be mild. Patients frequently do not seek treatment at an early stage. These symptoms may include: Minor pain that is present both with activity and at rest Pain radiating from the front of the shoulder to the side of the arm Sudden pain with lifting and reaching movements Athletes in overhead sports may have pain when throwing or serving a tennis ball As the problem progresses, the symptoms increase: Pain at night Loss of strength and motion Difficulty doing activities that place the arm behind the back, such as buttoning or zippering If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.

The examination consists of three portions: Inspection, Palpation, and Synthesis of data from these techniques In addition to palpating for size, also note the gland texture, mobility, tenderness and the presence of nodules. Inspection Inspection: Anterior Approach The patient should be seated or standing in a comfortable position with the neck in a neutral or slightly extended position. Cross-lighting increases shadows, improving the detection of masses. To enhance visualization of the thyroid, you can: Extending the neck, which stretches overlying tissues Have the patient swallow a sip of water, watching for the upward movement of the thyroid gland. quicktime video 251KB video demo from Return to the Bedside Inspection: Lateral Approach After completing anterior inspection of the thyroid, observe the neck from the side. Estimate the smooth, straight contour from the cricoid cartilage to the suprasternal notch. Measure any prominence beyond this imagined contour, using a ruler placed in the area of prominence. Palpation Note: There is no data comparing palpation using the anterior approach to the posterior approach so examiners should use the approach that they find most comfortable. Palpation: Anterior Approach placement of hands for palpatation of thyroid in anterior approach The patient is examined in the seated or standing position. Attempt to locate the thyroid isthmus by palpating between the cricoid cartilage and the suprasternal notch. Use one hand to slightly retract the sternocleidomastoid muscle while using the other to palpate the thyroid. Have the patient swallow a sip of water as you palpate, feeling for the upward movement of the thyroid gland. quicktime video 454KB video demo from Return to the Bedside. Palpation: Posterior Approach placement of hands for palpatation of thyroid in posterior approach The patient is examined in the seated or standing position. Standing behind the patient, attempt to locate the thyroid isthmus by palpating between the cricoid cartilage and the suprasternal notch. Move your hands laterally to try to feel under the sternocleidomstoids for the fullness of the thyroid. Have the patient swallow a sip of water as you palpate, feeling for the upward movement of the thyroid gland.

A visual prosthesis, often referred to as a bionic eye, is an experimental visual device intended to restore functional vision in those suffering from partial or total blindness. In 1983 Joao Lobo Antunes, a Portuguese doctor, implanted a bionic eye in a person born blind.

Mitosis is the process in which a eukaryotic cell nucleus splits in two, followed by division of the parent cell into two daughter cells. The word "mitosis" means "threads," and it refers to the threadlike appearance of chromosomes as the cell prepares to divide.
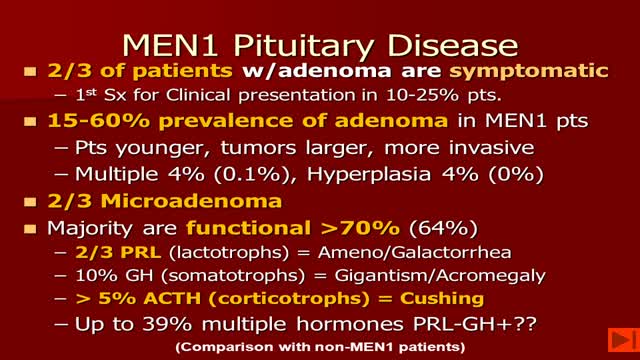
-MEN1 syndrome is composed of hyperparathyroidism, gastrinoma (pancreatic tumor) and pituitary tum or(remember the 3 Ps). Hyperparathyroidism in MEN1 is caused by hyperplasia of the parathyroid glands. Removal of 3 1/2 glands or total parathyroidectomy with autotransplantation is necessary.