Top videos

Neurotransmitter 3D Animation
on Tuesday, December 21, 2010
Neurotransmitters are endogenous chemicals which transmit signals from a neuron to a target cell across a synapse. Neurotransmitters are packaged into synaptic vesicles clustered beneath the membrane on the presynaptic side of a synapse, and are released into the synaptic cleft, where they bind to receptors in the membrane on the postsynaptic side of the synapse. Release of neurotransmitters usually follows arrival of an action potential at the synapse, but may also follow graded electrical potentials. Low level "baseline" release also occurs without electrical stimulation. Neurotransmitters are synthesized from plentiful and simple precursors, such as amino acids, which are readily available from the diet and which require only a small number of biosynthetic steps to convert. The chemical identity of neurotransmitters is often difficult to determine experimentally. For example, it is easy using an electron microscope to recognize vesicles on the presynaptic side of a synapse, but it may not be easy to determine directly what chemical is packed into them. The difficulties led to many historical controversies over whether a given chemical was or was not clearly established as a transmitter. In an effort to give some structure to the arguments, neurochemists worked out a set of experimentally tractable rules. According to the prevailing beliefs of the 1960s, a chemical can be classified as a neurotransmitter if it meets the following conditions: * There are precursors and/or synthesis enzymes located in the presynaptic side of the synapse. * The chemical is present in the presynaptic element. * It is available in sufficient quantity in the presynaptic neuron to affect the postsynaptic neuron; * There are postsynaptic receptors and the chemical is able to bind to them. * A biochemical mechanism for inactivation is present. There are many different ways to classify neurotransmitters. Dividing them into amino acids, peptides, and monoamines is sufficient for some classification purposes. Major neurotransmitters: * Amino acids: glutamate, aspartate, D-serine, γ-aminobutyric acid (GABA), glycine * Monoamines and other biogenic amines: dopamine (DA), norepinephrine (noradrenaline; NE, NA), epinephrine (adrenaline), histamine, serotonin (SE, 5-HT), melatonin * Others: acetylcholine (ACh), adenosine, anandamide, nitric oxide, etc. In addition, over 50 neuroactive peptides have been found, and new ones are discovered regularly. Many of these are "co-released" along with a small-molecule transmitter, but in some cases a peptide is the primary transmitter at a synapse. β-endorphin is a relatively well known example of a peptide neurotransmitter; it engages in highly specific interactions with opioid receptors in the central nervous system. Single ions, such as synaptically released zinc, are also considered neurotransmitters by some[by whom?], as are some gaseous molecules such as nitric oxide (NO) and carbon monoxide (CO). These are not classical neurotransmitters by the strictest definition, however, because although they have all been shown experimentally to be released by presynaptic terminals in an activity-dependent way, they are not packaged into vesicles. By far the most prevalent transmitter is glutamate, which is excitatory at well over 90% of the synapses in the human brain. The next most prevalent is GABA, which is inhibitory at more than 90% of the synapses that do not use glutamate. Even though other transmitters are used in far fewer synapses, they may be very important functionally—the great majority of psychoactive drugs exert their effects by altering the actions of some neurotransmitter systems, often acting through transmitters other than glutamate or GABA. Addictive drugs such as cocaine and amphetamine exert their effects primarily on the dop
Rectal bleeding can refer to any blood that passes from your anus, although rectal bleeding is usually assumed to refer to bleeding from your lower colon or rectum. Your rectum makes up the last few inches of your large intestine. Rectal bleeding may show up as blood in your stool, on the toilet paper or in the toilet bowl. Blood that results from rectal bleeding can range in color from bright red to dark maroon to a dark, tarry color.

Most times, a pulmonary embolism is caused by blood clots that travel from the legs or, rarely, other parts of the body (deep vein thrombosis, or DVT). Symptoms include shortness of breath, chest pain, and cough. Prompt treatment to break up the clot greatly reduces the risk of death. This can be done with blood thinners and drugs or procedures. Compression stockings and physical activity can help prevent clots from forming in the first place.

The Combitube is a twin lumen device designed for use in emergency situations and difficult airways. It can be inserted without the need for visualization into the oropharynx, and usually enters the esophagus. It has a low volume inflatable distal cuff and a much larger proximal cuff designed to occlude the oro- and nasopharynx.
If the tube has entered the trachea, ventilation is achieved through the distal lumen as with a standard ETT. More commonly the device enters the esophagus and ventilation is achieved through multiple proximal apertures situated above the distal cuff. In the latter case the proximal and distal cuffs have to be inflated to prevent air from escaping through the esophagus or back out of the oro- and nasopharynx.
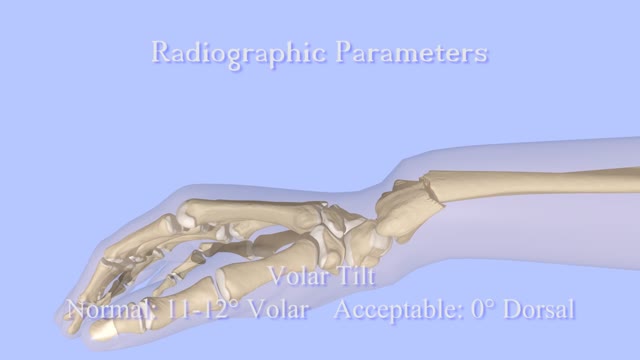
Closed Reduction of Distal Radius Fractures - Discussion: (distal radius fracture menu) - closed reduction & immobilization in plaster cast remains accepted method of treatment for majority of stable distal radius frx; - unstable fractures will often lose reduction in the cast and will slip back to the pre-reduction position; - patients should be examined for carpal tunnel symptoms before and after reduction; - carpal tunnel symptoms that do not resolve following reduction will require carpal tunnel release; - cautions: - The efficacy of closed reduction in displaced distal radius fractures. - Technique: - anesthesia: (see: anesthesia menu) - hematoma block w/ lidocaine; - w/ hematoma block surgeon should look for "flash back" of blood from hematoma, prior to injection; - references: - Regional anesthesia preferable for Colles' fracture. Controlled comparison with local anesthesia. - Neurological complications of dynamic reduction of Colles' fractures without anesthesia compared with traditional manipulation after local infiltration anesthesia. - methods of reduction: - Jones method: involves increasing deformity, applying traction, and immobilizing hand & wrist in reduced position; - placing hand & wrist in too much flexion (Cotton-Loder position) leads to median nerve compression & stiff fingers; - Bohler advocated longitudinal traction followed by extension and realignment; - consider hyper-extending the distal fragment, and then translating it distally (while in extended position) until it can be "hooked over" proximal fragment; - subsequently, the distal fragment can be flexed (or hinged) over the proximal shaft fragment; - closed reduction of distal radius fractures is facilitated by having an assistant provide counter traction (above the elbow) while the surgeon controls the distal fragment w/ both hands (both thumbs over the dorsal surface of the distal fragment); - flouroscopy: - it allows a quick, gentle, and complete reduction; - prepare are by prewrapping the arm w/ sheet cotton and have the plaster or fibroglass ready; - if flouroscopy is not available, then do not pre-wrap the extremity w/ cotton; - it will be necessary to palpate the landmarks (outer shaped of radius, radial styloid, and Lister's tubercle, in order to judge success of reduction; - casting: - generally, the surgeon will use a pre-measured double sugar sugar tong splint, which is 6-8 layers in thickness; - more than 8 layers of plaster can cause full thickness burns: - reference: Setting temperatures of synthetic casts. - position of immobilization - follow up: - radiographs: - repeat radiographs are required weekly for 2-3 weeks to ensure that there is maintenance of the reduction; - a fracture reduction that slips should be considered to be unstable and probably require fixation with (pins, or ex fix ect.) - there is some evidence that remanipulation following fracture displacement in cast is not effective for these fractures; - ultimately, whether or not a patient is satisfied with the results of non operative treatment depends heavily on th

Here we’ll explain the symptoms of pancreatitis, how alcohol causes the condition and the other health problems it can lead to. You probably don’t pay much attention to your pancreas. But that small, tadpole-shaped organ behind your stomach and below your ribcage is pretty important. It produces two essential substances: digestive juices which your intestines use to break down food, and hormones that are involved in digestion, such as insulin, which regulates your blood sugar levels. Pancreatitis is when your pancreas becomes inflamed and its cells are damaged. Heavy drinking can cause pancreatitis. But if you drink within the government’s low risk unit guidelines, you should avoid upsetting this important organ.
Femoroacetabular impingement (FAI) is a condition in which extra bone grows along one or both of the bones that form the hip joint — giving the bones an irregular shape. Because they do not fit together perfectly, the bones rub against each other during movement. Over time this friction can damage the joint, causing pain and limiting activity.

Clinical Review First aid and treatment of minor burns BMJ 2004; 328 doi: https://doi.org/10.1136/bmj.328.7454.1487 (Published 17 June 2004) Cite this as: BMJ 2004;328:1487 Article Related content Metrics Responses Jackie Hudspith, clinical nurse lead, Sukh Rayatt, specialist registrar, plastic and reconstructive surgery Author affiliations Introduction Some 250 000 burns occur annually in the United Kingdom. About 90% of these are minor and can be safely managed in primary care. Most of these will heal regardless of treatment, but the initial care can have a considerable influence on the cosmetic outcome. All burns should be assessed by taking an adequate history and examination.