Top videos

www.diabetes.org > Living With Diabetes > Treatment and Care > Medication > Insulin & Other Injectables Share: Print PageText Size:A A A Listen How Do Insulin Pumps Work? If you have been diagnosed with diabetes, you may feel overwhelmed by all the new information you have learned and will continue to learn about managing your diabetes. You already know your main goal should be to get your blood glucose (sugar) levels under control in order to increase your chances of a complication-free life. Many people know this, but need to know how to achieve good diabetes management, while balancing the day-to-day demands of diabetes with other life demands. An insulin pump can help you manage your diabetes. By using an insulin pump, you can match your insulin to your lifestyle, rather than getting an insulin injection and matching your life to how the insulin is working. When you work closely with your diabetes care team, insulin pumps can help you keep your blood glucose levels within your target ranges. People of all ages with type 1 diabetes use insulin pumps and people with type 2 diabetes have started to use them as well. - See more at: http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/insulin/how-do-insulin-pumps-work.html?referrer=https://www.google.com/#sthash.XD56v351.dpuf
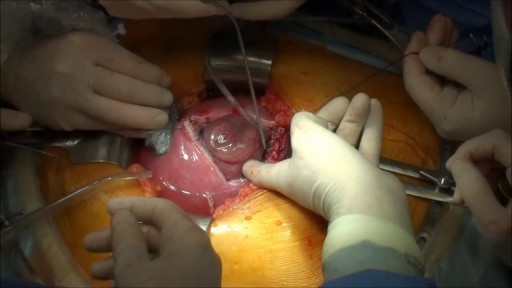
Prenatal repair of myelomeningocele (MMC), the most common and severe form of spina bifida, is a delicate surgical procedure where fetal surgeons open the uterus and close the opening in the baby's back while they are still in the womb.

Most C-sections are done under regional anesthesia, which numbs only the lower part of your body — allowing you to remain awake during the procedure. A common choice is a spinal block, in which pain medication is injected directly into the sac surrounding your spinal cord

Thoracentesis is a procedure used to obtain a sample of fluid from the space around the lungs. Normally, only a thin layer of fluid is present in the area between the lungs and chest wall. However, some conditions can cause a large amount of fluid to accumulate. This collection of fluid is called a pleural effusion.

Mysterious massage from East Asia(CHINA).it can cure cure Erectile dysfunction,can let their life better.This video from mainland of China,so the language is Chinese mandarin.but you can see English show on the video too.Tiedang gong means kongfu of Iron penis&balls.

Lumpectomy means that a focal area of cancer is going to be removed. A lot of patients with a lumpectomy don’t need any specific breast reconstruction, explains Dr. Miguel Angel Medina, Director of Microsurgery with Miami Cancer Institute.
Al the end of surgical treatment, all those patients go on to need radiation therapy. For patients who have large breasts, physicians have to take a larger lumpectomy than normal.
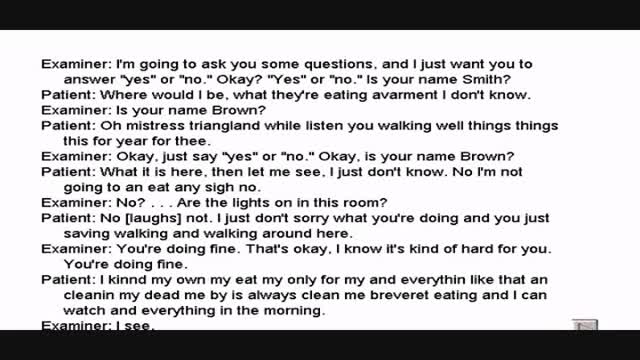
Wernicke's aphasia is a neurological disorder typically caused by stroke. It affects the Wernicke's region in the brain's left hemisphere which is reasoned to be responsible for processing of meaning, especially as it relates to verbal communication, hence the problems with speech witnessed in these patients
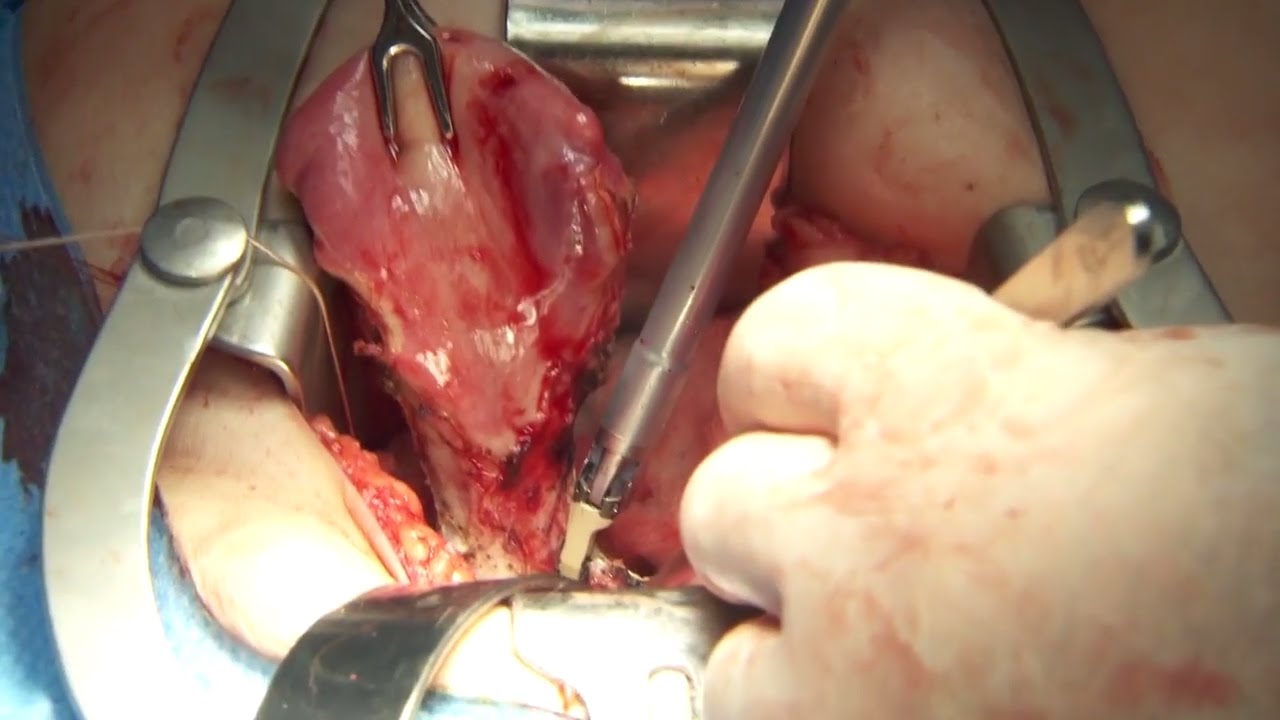
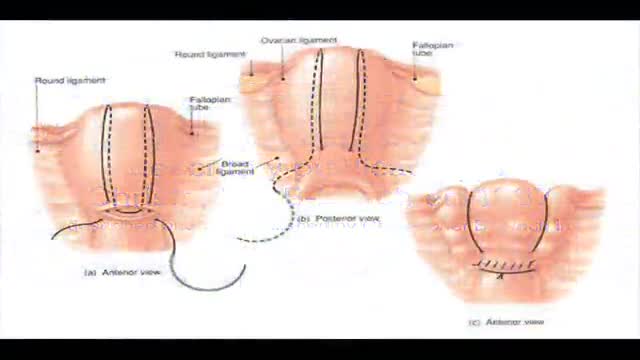
Olympus has extended the value of its award-winning combined surgical energy device, THUNDERBEAT, to open surgical procedures. Watch Dr. Francois Blaudeau master use of THUNDERBEAT Open Extended Jaw (OEJ) in a total abdominal hysterectomy.
http://medical.olympusamerica.com/products/thunderbeat?utm_source=youtube&utm_campaign=Total%20Abdominal%20Hysterectomy%20Surgery%20-%20THUNDERBEAT&utm_medium=description&utm_term=energy&utm_content=surgical
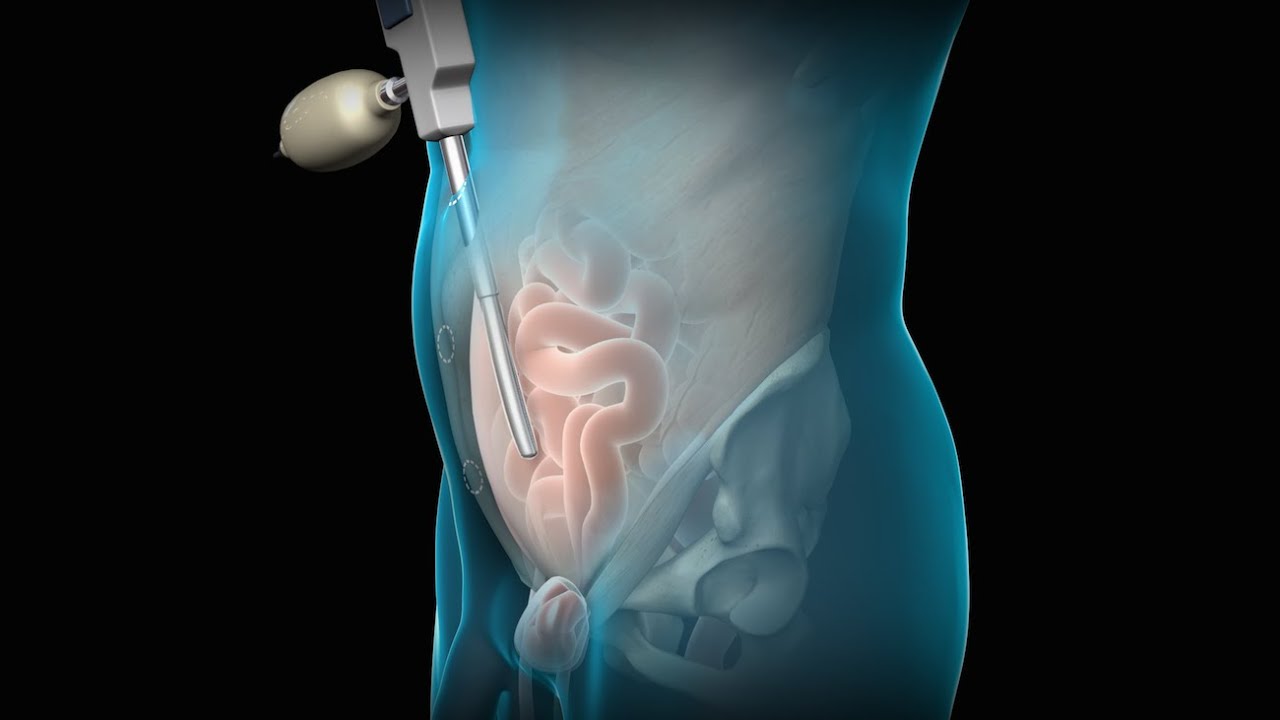
To license this video for patient education or content marketing, visit: http://www.nucleushealth.com/?utm_source=youtube&utm_medium=video-description&utm_campaign=tephernia-030615
An inguinal hernia is a bulging of the intestine through a defect or weak spot in the wall of the lower abdomen. This video shows how inguinal hernias form and how they are treated.
#TotalExtraperitonealLaparoscopicInguinalHerniaRepair #TEP #laparoscopy
ANCE00200

Most women have vaginal discharge at many different times throughout their cycle. During ovulation, white and watery discharge is common and accepted as normal. But, discharge after ovulation is widely believed to be a sign of pregnancy.

Site enhancement oil, often called "santol" or "synthol" (no relation to the Synthol mouthwash brand), refers to oils injected into muscles to increase the size or change the shape. Some bodybuilders, particularly at the professional level, inject their muscles with such mixtures to mimic the appearance of developed muscle where it may otherwise be disproportionate or lagging. This is known as "fluffing".Synthol is 85% oil, 7.5% lidocaine, and 7.5% alcohol. It is not restricted, and many brands are available on the Internet. The use of injected oil to enhance muscle appearance is common among bodybuilders, despite the fact that synthol can cause pulmonary embolisms, nerve damage, infections, sclerosing lipogranuloma,[60] stroke,[55] and the formation of oil-filled granulomas, cysts or ulcers in the muscle. Rare cases might require surgical intervention to avoid further damage to the muscle and/or to prevent loss of life. Sesame oil is often used in such mixtures, which can cause allergic reactions such as vasculitis.