Top videos
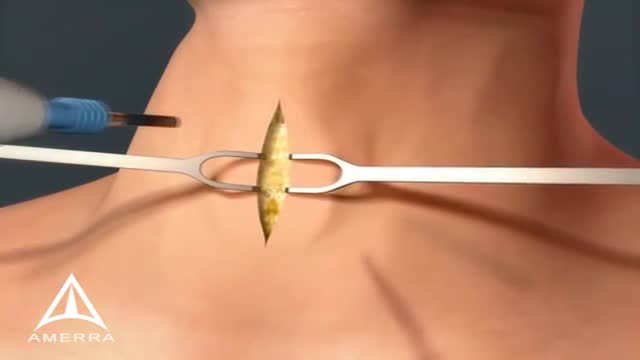
A tracheotomy or a tracheostomy is an opening surgically created through the neck into the trachea (windpipe) to allow direct access to the breathing tube and is commonly done in an operating room under general anesthesia. A tube is usually placed through this opening to provide an airway and to remove secretions from the lungs. Breathing is done through the tracheostomy tube rather than through the nose and mouth. The term “tracheotomy” refers to the incision into the trachea (windpipe) that forms a temporary or permanent opening, which is called a “tracheostomy,” however; the terms are sometimes used interchangeably.

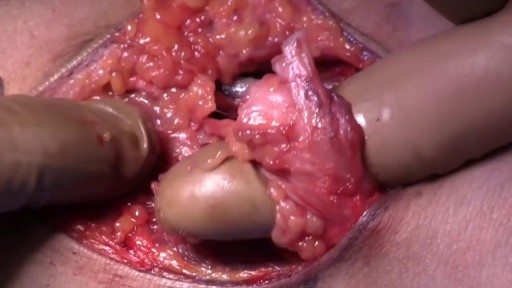
Shoulder dystocia is a rare emergency that can happen during the end of the second stage of labour. It's all to do with how your baby moves down through your vagina and out into the world. Shoulder dystocia happens when your baby's head has been born, but one of her shoulders becomes stuck.

The cat's stomach is a sac-like structure designed to store large volumes of food and continue the digestive process. The esophagus carries food to the stomach, where it enters via a valve-like structure called the cardiac sphincter. On the interior surface of the stomach is a series of folds called gastric folds. These folds function to help grind and digest food. The inner stomach lining secretes acids and enzymes to break down food. Once the initial stomach digestive process is complete, the partially digested food exits the stomach through the pyloric sphincter area and then enters the duodenum (first segment of the small intestine). Once eaten, most food leaves the stomach within twelve hours after entering.
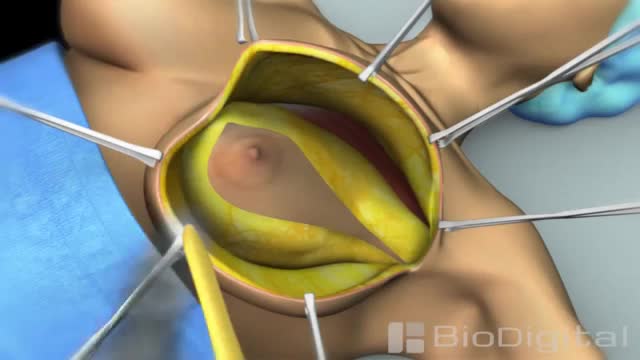
Mastectomy is surgery to remove all breast tissue from a breast as a way to treat or prevent breast cancer. For those with early-stage breast cancer, mastectomy may be one treatment option. Breast-conserving surgery (lumpectomy), in which only the tumor is removed from the breast, may be another option.

irregular, curved toenails. footwear that places a lot of pressure on the big toes, such as socks and stockings that are too tight or shoes that are too tight, narrow, or flat for your feet. toenail injury, including stubbing your toe, dropping something heavy on your foot, or kicking a ball repeatedly. poor posture. How can ingrowing toenails be prevented? Cut your nails straight across; do not cut them too short or too low at the sides. ... Keep your feet clean and dry. ... Avoid tight shoes and use cotton socks rather than synthetic. If you have diabetes, you should take extra care when cutting your nails:

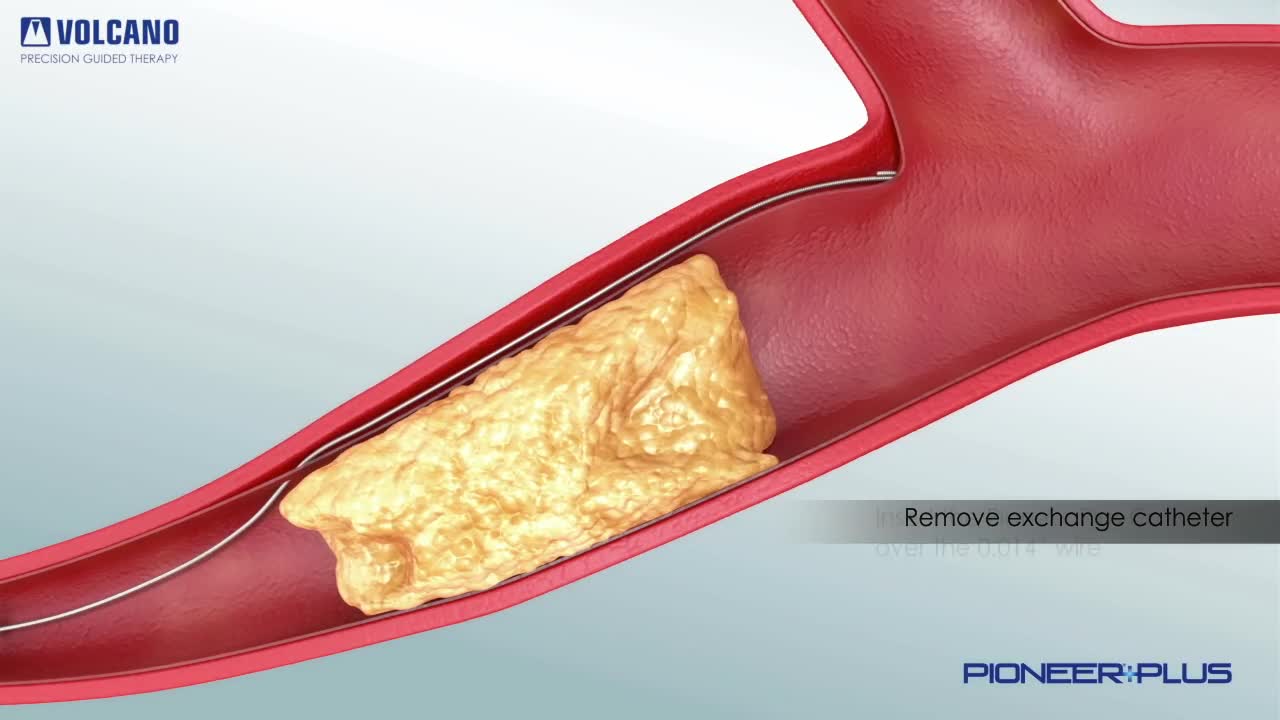
Blood clotting, or coagulation, is an important process that prevents excessive bleeding when a blood vessel is injured. Platelets (a type of blood cell) and proteins in your plasma (the liquid part of blood) work together to stop the bleeding by forming a clot over the injury.

A pneumothorax is usually caused by an injury to the chest, such as a broken rib or puncture wound. It may also occur suddenly without an injury. A pneumothorax can result from damage to the lungs caused by conditions such as chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, and pneumonia.
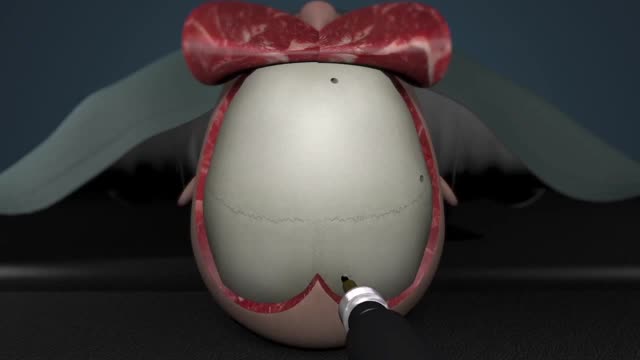
A craniotomy is the surgical removal of part of the bone from the skull to expose the brain. Specialized tools are used to remove the section of bone called the bone flap. The bone flap is temporarily removed, then replaced after the brain surgery has been done.
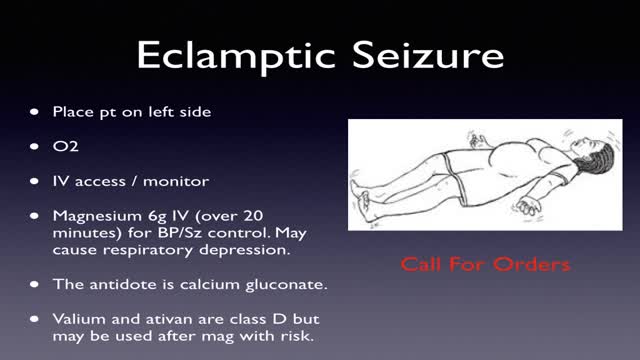
Obstetrical emergencies of pregnancy ECTOPIC PREGNANCY. ... PLACENTAL ABRUPTION. ... PLACENTA PREVIA. ... ECTOPIC PREGNANCY. ... PLACENTAL ABRUPTION. ... PLACENTA PREVIA. ... Amniotic fluid — The liquid in the placental sac that cushions the fetus and regulates temperature in the placental environment.
The biceps muscle is located in the front of your upper arm. It is attached to the bones of the shoulder and elbow by tendons — strong cords of fibrous tissue that attach muscles to bones. Tears of the biceps tendon at the elbow are uncommon. They are most often caused by a sudden injury and tend to result in greater arm weakness than injuries to the biceps tendon at the shoulder. Once torn, the biceps tendon at the elbow will not grow back to the bone and heal. Other arm muscles make it possible to bend the elbow fairly well without the biceps tendon. However, they cannot fulfill all the functions of the elbow, especially the motion of rotating the forearm from palm down to palm up. This motion is called supination. To return arm strength to near normal levels, surgery to repair the torn tendon is usually recommended. However, nonsurgical treatment is a reasonable option for patients who may not require full arm function.
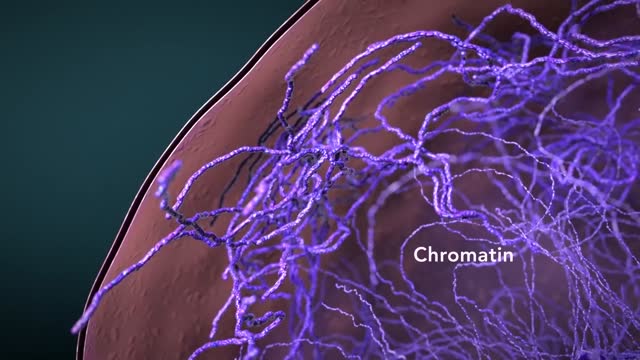
Cytoplasmic organelles are "little organs" that are suspended in the cytoplasm of the cell. Each type of organelle has a definite structure and a specific role in the function of the cell. Examples of cytoplasmic organelles are mitochondrion, ribosomes, endoplasmic reticulum, golgi apparatus, and lysosomes.
Cushing's disease is a serious condition of an excess of the steroid hormone cortisol in the blood level caused by a pituitary tumor secreting adrenocorticotropic hormone (ACTH). ACTH is a hormone produced by the normal pituitary gland. ACTH stimulates the adrenal glands (located on top of the kidneys) to produce cortisol, commonly referred to as the stress hormone.
Blind loop syndrome (BLS), commonly referred to in the literature as small intestinal bacterial overgrowth (SIBO) or bacterial overgrowth syndrome (BOS), is a state that occurs when the normal bacterial flora of the small intestine proliferates to numbers that cause significant derangement to the normal physiological ...