Top videos

Visualization of the larynx by direct or indirect means is referred to as laryngoscopy and is the principal aim during airway management for passage of a tracheal tube. This paper presents a brief background regarding the development and practice of laryngoscopy and examines the equipment and techniques for both direct and indirect methods. Patient evaluation during the airway examination is discussed, as are predictors for difficult intubation. Laryngoscope blade design, newer intubating techniques, and a variety of indirect laryngoscopic technologies are reviewed, as is the learning curve for these techniques and devices.

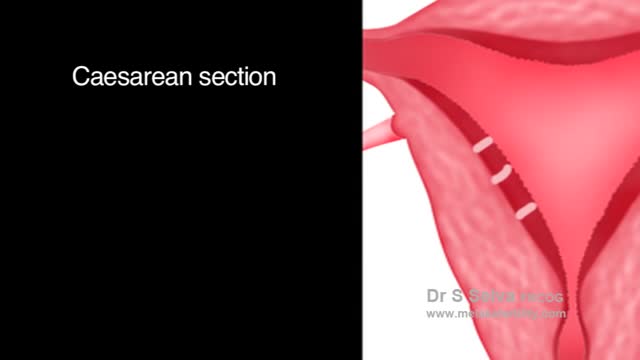
Note: This video contains graphic surgical footage so viewer discretion is advised.
Director of the Penn Orthopaedics Robotics and Navigation Program, Dr. Christopher Travers, discusses robotic joint replacement surgery, which is one of the multiple options that Penn Orthopaedics offers for joint replacement surgery. He walks through a robotic knee replacement surgery, discussing what the procedure is, how it differs from traditional joint replacement surgery, and the benefits.
Refer a patient (physicians only):
https://www.pennmedicine.org/refer-your-patient
Learn more about the Penn Joint Replacement Program:
https://www.pennmedicine.org/f....or-patients-and-visi
Learn more about Dr. Travers:
https://www.pennmedicine.org/providers/profile/christopher-travers?fadf=pennmedicine&keyword=travers
#RoboticSurgery #JointReplacementSurgery #KneeReplacement #SurgicalFootage

The lungs and respiratory system allow oxygen in the air to be taken into the body, while also enabling the body to get rid of carbon dioxide in the air breathed out. Respiration is the term for the exchange of oxygen from the environment for carbon dioxide from the body's cells.
The superior sagittal sinus (also known as the superior longitudinal sinus), within the human head, is an unpaired area along the attached margin of falx cerebri. It allows blood to drain from the lateral aspects of anterior cerebral hemispheres to the confluence of sinuses.

Cerebral palsy refers to brain damage that occurs before a child is five years old. Therefore, adults cannot develop cerebral palsy. However, cerebral palsy does not get better or worse with age, so when a child has the condition, he or she will continue to have the condition into adulthood.

Orthopedic surgeon Donald Polakoff, MD describes recovery time from knee replacement surgery.
SUBSCRIBE FOR MORE VIDEOS AND NEWS!
http://www.youtube.com/subscri....ption_center?add_use
CONNECT WITH US!
Google+ ► http://gplus.to/spuh
Facebook ► http://www.fb.com/SaintPetersUniversityHospital
Twitter ► http://twitter.com/sphcs_news
Pinterest ► http://www.pinterest.com/sphcs
Saint Peter's Healthcare System ► http://www.saintpetershcs.com
In developing countries, domestic animals (eg, dogs) are common sources of infection. In the United States, bats and wild animals (eg, raccoons) are the most common reservoirs of infection. The acquisition of rabies from bats can occur from an unrecognized bite or a scratch, and possibly by inhalation of aerosolized viral particles. Bats are found in all states except Hawaii, and spelunking (cave exploration) is a risk factor for rabies acquisition from bats.
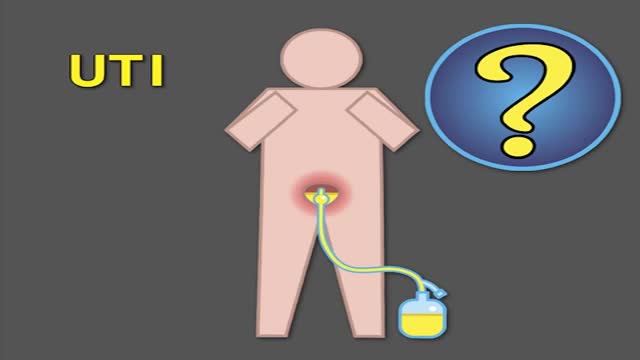
Indwelling urinary catheters are commonly used in hospitals and can lead to preventable catheter-associated UTI. How can rates of catheter-associated UTI be reduced in hospitals? New research findings are summarized in a new NEJM Quick Take. Learn more at http://nej.md/1WoeHdF SHOW MORE

A burn is tissue damage that results from scalding, overexposure to the sun or other radiation, contact with flames, chemicals or electricity, or smoke inhalation. Is it a major or minor burn? Call 911 or seek immediate care for major burns, which: Are deep Cause the skin to be dry and leathery May appear charred or have patches of white, brown or black Are larger than 3 inches (about 8 centimeters) in diameter or cover the hands, feet, face, groin, buttocks or a major joint A minor burn that doesn't require emergency care may involve: Superficial redness similar to a sunburn Pain Blisters An area no larger than 3 inches (about 8 centimeters) in diameter Treating major burns Until emergency help arrives: Protect the burned person from further harm. If you can do so safely, make sure the person you're helping is not in contact with the source of the burn. For electrical burns, make sure the power source is off before you approach the burned person. Make certain that the person burned is breathing. If needed, begin rescue breathing if you know how. Remove jewelry, belts and other restrictive items, especially from around burned areas and the neck. Burned areas swell rapidly. Cover the area of the burn. Use a cool, moist bandage or a clean cloth. Don't immerse large severe burns in water. Doing so could cause a serious loss of body heat (hypothermia). Elevate the burned area. Raise the wound above heart level, if possible. Watch for signs of shock. Signs and symptoms include fainting, pale complexion or breathing in a notably shallow fashion. Treating minor burns For minor burns: Cool the burn. Hold the burned area under cool (not cold) running water or apply a cool, wet compress until the pain eases. Remove rings or other tight items from the burned area. Try to do this quickly and gently, before the area swells. Don't break blisters. Fluid-filled blisters protect against infection. If a blister breaks, clean the area with water (mild soap is optional). Apply an antibiotic ointment. But if a rash appears, stop using the ointment. Apply lotion. Once a burn is completely cooled, apply a lotion, such as one that contains aloe vera or a moisturizer. This helps prevent drying and provides relief. Bandage the burn. Cover the burn with a sterile gauze bandage (not fluffy cotton). Wrap it loosely to avoid putting pressure on burned skin. Bandaging keeps air off the area, reduces pain and protects blistered skin. If needed, take an over-the-counter pain reliever, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) or acetaminophen (Tylenol, others).

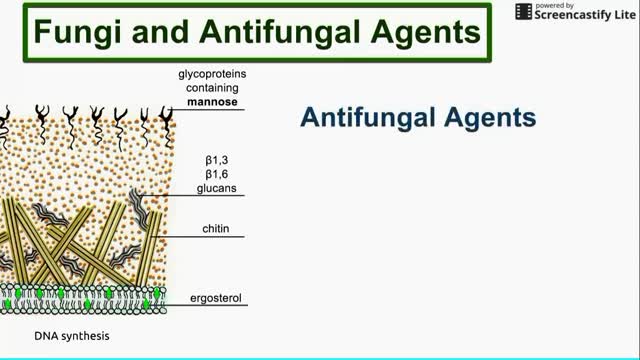
Allergic bronchopulmonary aspergillosis (ABPA) is a condition characterised by an exaggerated response of the immune system (a hypersensitivity response) to the fungus Aspergillus (most commonly Aspergillus fumigatus). It occurs most often in patients with asthma or cystic fibrosis.
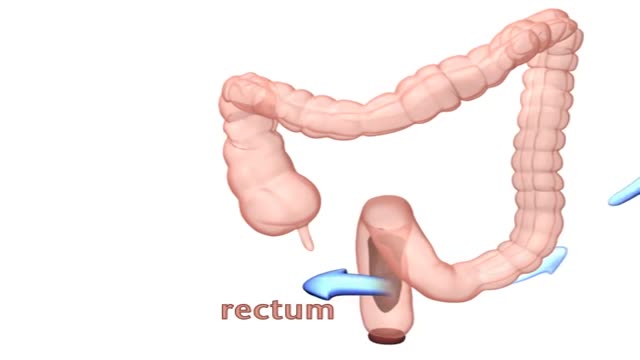
Encopresis is a problem that children age four or older can develop due to chronic (long-term) constipation. With constipation, children have fewer bowel movements than normal, and the bowel movements they do have can be hard, dry, and difficult to pass. The child may avoid using the bathroom to avoid discomfort.

During open carpal tunnel release surgery, the transverse carpal ligament is cut, which releases pressure on the median nerve and relieves the symptoms of carpal tunnel syndrome. An incision is made at the base of the palm of the hand. This allows the doctor to see the transverse carpal ligament.
Adenomyosis is a condition in which the inner lining of the uterus (the endometrium) breaks through the muscle wall of the uterus (the myometrium). Adenomyosis can cause menstrual cramps, lower abdominal pressure, and bloating before menstrual periods and can result in heavy periods.
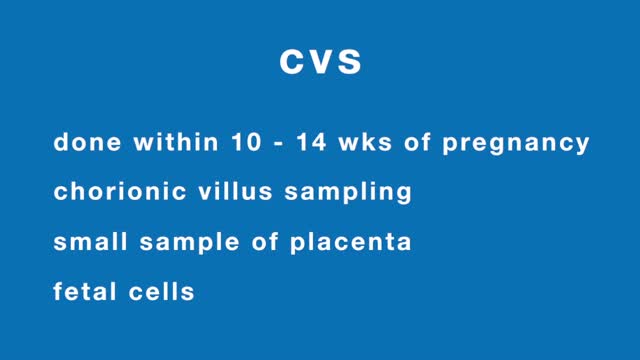
Chorionic villus sampling, often referred to as CVS, is a diagnostic test for identifying chromosome abnormalities and other inherited disorders. This test may be recommended by your health care provider, if you or your partner has family medical histories that reveal potential risks.