Top videos

Function and Anatomy: The hip is a ball and socket type joint, formed by the articulation of the head of the femur with the pelvis. Normal range of motion includes: abduction 45 degrees, adduction 20-30 degrees, flexion 135 degrees, extension 30 degrees, internal and external rotation. Hip pathology can cause symptoms anywhere around the joint, though frequently pain is anterior and radiates to the groin region. Additionally, pathology outside of the hip can be referred to this region. History and exam obviously help in making these distinctions.

Common Benign Pain Syndromes--Symptoms and Etiology:
1. Non-specific musculoskeletal pain: This is the most common cause of back pain. Patients present with lumbar area pain that does not radiate, is worse with activity, and improves with rest. There may or may not be a clear history of antecedent over use or increased activity. The pain is presumably caused by irritation of the paraspinal muscles, ligaments or vertebral body articulations. However, a precise etiology is difficulty to identify.
2. Radicular Symptoms: Often referred to as "sciatica," this is a pain syndrome caused by irritation of one of the nerve roots as it exits the spinal column. The root can become inflamed as a result of a compromised neuroforamina (e.g. bony osteophyte that limits size of the opening) or a herniated disc (the fibrosis tears, allowing the propulsus to squeeze out and push on the adjacent root). Sometimes, it's not precisely clear what has lead to the irritation. In any case, patient's report a burning/electric shock type pain that starts in the low back, traveling down the buttocks and along the back of the leg, radiating below the knee. The most commonly affected nerve roots are L5 and S1.
3. Spinal Stenosis: Pain starts in the low back and radiates down the buttocks bilaterally, continuing along the backs of both legs. Symptoms are usually worse with walking and improve when the patient bends forward. Patient's may describe that they relieve symptoms by leaning forward on their shopping carts when walking in a super market. This is caused by spinal stenosis, a narrowing of the central canal that holds the spinal cord. The limited amount of space puts pressure on the nerve roots when the patient walks, causing the symptoms (referred to as neurogenic claudication). Spinal stenosis can be congenital or develop over years as a result of djd of the spine. As opposed to true claudication (pain in calfs/lower legs due to arterial insufficiency), pain resolves very quickly when person stops walking and assumes upright position. Also, peripheral pulses should be normal.
4. Mixed symptoms: In some patients, more then one process may co-exist, causing elements of more then one symptom syndrome to co-exist.

Clinical Review First aid and treatment of minor burns BMJ 2004; 328 doi: https://doi.org/10.1136/bmj.328.7454.1487 (Published 17 June 2004) Cite this as: BMJ 2004;328:1487 Article Related content Metrics Responses Jackie Hudspith, clinical nurse lead, Sukh Rayatt, specialist registrar, plastic and reconstructive surgery Author affiliations Introduction Some 250 000 burns occur annually in the United Kingdom. About 90% of these are minor and can be safely managed in primary care. Most of these will heal regardless of treatment, but the initial care can have a considerable influence on the cosmetic outcome. All burns should be assessed by taking an adequate history and examination.
When you’re trying to conceive a baby it is worth giving anything a go which you think will boost your chances. This includes considering that there may be better positions for getting pregnant. But it pays to bear in mind that the human race has been around for over 200,000 years and most of us were probably conceived without our ancestors investing too much thought into the mechanics. Science has proven that successful conception isn’t so much about sexual position as the frequency of sex between a fertile couple. Basically, if you want to fall pregnant, don’t use contraception and have frequent, active and enjoyable sex. Importantly, don’t stress too much about whether you’re doing it the right way. Women can, and do, conceive in any position. Nature has a way of making sure of that.
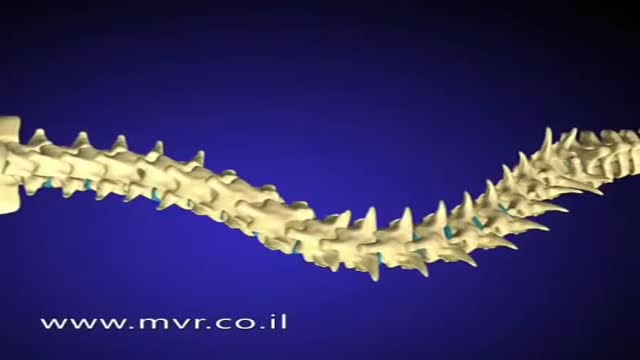
There are several approaches to scoliosis surgery, but all use modern instrumentation systems in which hooks and screws are applied to the spine to anchor long rods. The rods are then used to reduce and hold the spine while bone that is added fuses together with existing bone.

Breast Cancer spreads by 3 mechanisms- local spread, by lymph nodes, or through the blood. Dr. Lorraine Champion, and Dr. Lisa Bailey discuss how breast cancer spreads. They discuss the different methods of spread and how this will affect the treatment of breast cancer.

Physical assessment is taking an educated, systematic look at all aspects of an individual’s health status utilizing knowledge, skills and tools of health history and physical exam. To collect data- information about the client’s health, including physiological, psychological, sociocultural and spiritual aspects To establish actual and potential problems To establish the nurse-client relationship Method: The history is done first, then the physical examination focuses on finding data associated with the history. Health History- obtained through interview and record review. Physical exam- accomplished by tools and techniques ** A complete assessment is not necessarily carried out each time. A comprehensive assessment is part of a health screening examination. On admission, you will do an admission assessment (not necessarily including everything presented here) and document it on the admission form. You will do a daily shift assessment (patient systems review). And, if client has a specific problem, you may assess only that part of the body (focused). Data Collection: Information is organized into objective and subjective data: Subjective: Apparent only to person affected; includes client’s perceptions, feelings, thoughts, and expectations. It cannot be directly observed and can be discovered only asking questions. Objective: Detectable by an observer or can be tested against an acceptable standard; tangible, observable facts; includes observation of client behavior, medical records, lab and diagnostic tests, data collected by physical exam. ** To obtain data for the nursing health history, you must utilize good interview techniques and communications skills. Record accurately. DO NOT ASSUME. D. Frameworks for Health Assessment There are two main frameworks utilized in health assessment: Head to Toe- systematic collection of data starting with the head and working downward. Functional Health Assessment- Gordon’s 11 functional health patterns that address the behaviors a person uses to maintain health. PERSON is the ACC-ADN framework for assessment. It is similar to Gordon's functional health patterns.

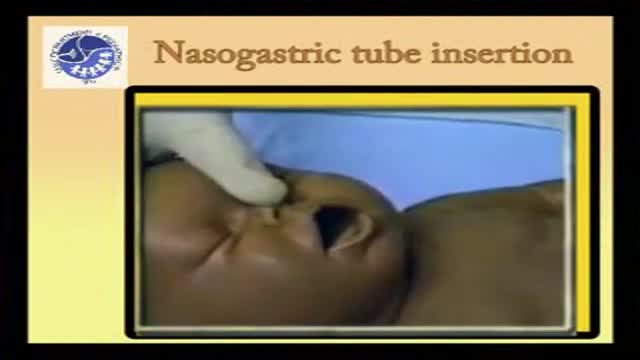
The following guidelines are an interpretation of the evidence presented in the 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations1). They apply primarily to newly born infants undergoing transition from intrauterine to extrauterine life, but the recommendations are also applicable to neonates who have completed perinatal transition and require resuscitation during the first few weeks to months following birth. Practitioners who resuscitate infants at birth or at any time during the initial hospital admission should consider following these guidelines. For the purposes of these guidelines, the terms newborn and neonate are intended to apply to any infant during the initial hospitalization. The term newly born is intended to apply specifically to an infant at the time of birth.

Rotator cuff pain commonly causes local swelling and tenderness in the front of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position. Beginning symptoms may be mild. Patients frequently do not seek treatment at an early stage. These symptoms may include: Minor pain that is present both with activity and at rest Pain radiating from the front of the shoulder to the side of the arm Sudden pain with lifting and reaching movements Athletes in overhead sports may have pain when throwing or serving a tennis ball As the problem progresses, the symptoms increase: Pain at night Loss of strength and motion Difficulty doing activities that place the arm behind the back, such as buttoning or zippering If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.

New York Plastic Surgeon, Carlin Vickery, MD (http://www.5thavesurgery.com) performs a CoolSculpting by Zeltiq procedure.
A NYC patient in this video explains her interest in the CoolSculpting procedure and discusses her experience on camera while receiving this Zeltiq treatment.