Top videos

Bone tumors develop when cells in the bone divide without control, forming a mass of tissue. Most bone tumors are benign, which means they are not cancer and cannot spread. However, they may still weaken bone and lead to fractures or cause other problems. Bone cancer destroys normal bone tissue and may spread to other parts of the body (called metastasis). Benign Bone Tumors Benign tumors are more common than malignant tumors of the bones. These are a few common types of benign bone tumors: Osteochondroma is the most common benign bone tumor. It is more common in people under age 20. Giant cell tumor is a benign tumor, typically affecting the leg (malignant types of this tumor are uncommon). Osteoid osteoma is a bone tumor, often occurring in long bones, that occurs commonly in the early 20s. Osteoblastoma is a single tumor that occurs in the spine and long bones, mostly in young adults. Enchondroma usually appears in bones of the hand and feet. It often has no symptoms. It is the most common type of hand tumor.
The menstrual cycle is the regular natural change that occurs in the female reproductive system like the uterus and ovaries that make pregnancy possible. The cycle is required for the production of ovocytes, and for the preparation of the uterus for pregnancy.
Myelodysplastic syndromes are a group of cancers in which immature blood cells in the bone marrow do not mature or become healthy blood cells. In a healthy person, the bone marrow makes blood stem cells (immature cells) that become mature blood cells over time.Aug 12, 2015

Spina bifida is a condition that affects the spine and is usually apparent at birth. It is a type of neural tube defect (NTD). Spina bifida can happen anywhere along the spine if the neural tube does not close all the way. When the neural tube doesn’t close all the way, the backbone that protects the spinal cord doesn’t form and close as it should. This often results in damage to the spinal cord and nerves. Spina bifida might cause physical and intellectual disabilities that range from mild to severe. The severity depends on: The size and location of the opening in the spine. Whether part of the spinal cord and nerves are affected.
Major signs and symptoms include enlargement of the liver and spleen (hepatosplenomegaly), a low number of red blood cells (anemia), easy bruising caused by a decrease in blood platelets (thrombocytopenia), lung disease, and bone abnormalities such as bone pain, fractures, and arthritis.
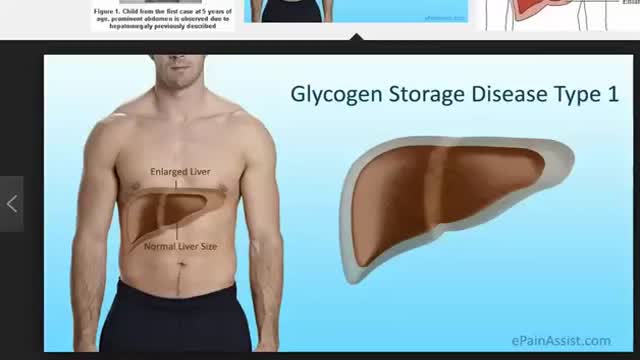
Signs and symptoms of this condition typically appear around the age of 3 or 4 months, when babies start to sleep through the night and do not eat as frequently as newborns. Affected infants may have low blood sugar (hypoglycemia), which can lead to seizures. They can also have a buildup of lactic acid in the body (lactic acidosis), high blood levels of a waste product called uric acid (hyperuricemia), and excess amounts of fats in the blood (hyperlipidemia). As they get older, children with GSDI have thin arms and legs and short stature. An enlarged liver may give the appearance of a protruding abdomen. The kidneys may also be enlarged. Affected individuals may also have diarrhea and deposits of cholesterol in the skin (xanthomas).
Surgery to replace an aortic valve is done for aortic valve stenosis and aortic valve regurgitation. During this surgery, the damaged valve is removed and replaced with an artificial valve. The valve replacement is typically an open-heart surgery.

Mohs Surgeon Dr. Leslie Christenson shows entire Mohs Surgery from start to finish. This is the full procedure and includes the entire surgery. Dr. Christenson talks about the procedure as she removes the skin cancer.
Learn more about Dr. Christenson: https://www.mcfarlandclinic.co....m/doctors/leslie-chr
Learn more about Mohs Surgery: https://www.mcfarlandclinic.co....m/doctors/specialtie
The vast majority of glucocorticoid activity in most mammals is from cortisol, also known as hydrocortisone. Corticosterone, the major glucocorticoid in rodents, is another glucocorticoid. Cortisol binds to the glucocorticoid receptor in the cytoplasm and the hormone-receptor complex is then translocated into the nucleus, where it binds to its DNA response element and modulates transcription from a battery of genes, leading to changes in the cell's phenotype. Only about 10% of circulating cortisol is free. The remaining majority circulates bound to plasma proteins, particularly corticosteroid-binding globulin (transcortin). This protein binding likely decreases the metabolic clearance rate of glucocorticoids and, because the bound steroid is not biologically active, tends to act as a buffer and blunt wild fluctuations in cortisol concentration.

Pediatric Surgery Day Unit (PSDU)
Welcome to Harley Street state-of-the-art Pediatric Surgery Day Unit! We are thrilled to have the opportunity to provide exceptional care and support for our young patients and their families. At our unit, we understand the unique needs and concerns associated with pediatric surgery, and we strive to create a safe and comforting environment for everyone involved.
Compassionate Care by Dedicated Professionals
Lead by Consultant Pediatric Surgeon, Dr. Niall Martin Jones, we will ensure your baby is looked after to the highest possible standards. Our dedicated team and support staff is committed to delivering the highest quality of care. All procedures are performed with local anesthetic and sucrose for comfort. Usually, your baby is so comfortable that she/he will be asleep by the end of the treatment.
Advanced Technology and Safety Measures
Patient safety is our utmost priority. We have implemented rigorous infection control measures to ensure a sterile environment. Our operating rooms are equipped with advanced technology and monitoring systems to ensure the highest standards of safety and precision during surgery. Our anesthesiologists are experienced in administering anesthesia to children, ensuring a smooth and comfortable experience.
learn more https://www.hsmc.ae/our-clinic....s/pediatric-surgery-
#pediatricsurgery #pediatrics #childhealthcare

Visualization of the larynx by direct or indirect means is referred to as laryngoscopy and is the principal aim during airway management for passage of a tracheal tube. This paper presents a brief background regarding the development and practice of laryngoscopy and examines the equipment and techniques for both direct and indirect methods. Patient evaluation during the airway examination is discussed, as are predictors for difficult intubation. Laryngoscope blade design, newer intubating techniques, and a variety of indirect laryngoscopic technologies are reviewed, as is the learning curve for these techniques and devices.

The lungs and respiratory system allow oxygen in the air to be taken into the body, while also enabling the body to get rid of carbon dioxide in the air breathed out. Respiration is the term for the exchange of oxygen from the environment for carbon dioxide from the body's cells.
The superior sagittal sinus (also known as the superior longitudinal sinus), within the human head, is an unpaired area along the attached margin of falx cerebri. It allows blood to drain from the lateral aspects of anterior cerebral hemispheres to the confluence of sinuses.

-Korsakoff's syndrome is a common and preventable sequel of Wernicke's encephalopathy. Thiamine, if given during the stage of Wernicke's encephalopathy, can prevent the onset of Korsakoff's psychosis. The administration of glucose prior to thiamine can precipitate Korsakoff's syndrome, as seen in this case. In such patients, brain MRI frequently shows abnormal enhancement of the mammillary bodies & thallamus

An epidural abscess is a collection of pus (infected material) between the outer covering of the brain and spinal cord and the bones of the skull or spine. The abscess causes swelling in the area. Spinal cord abscess (SCA) is a rare condition capable of causing permanent damage to the spinal cord. Abscesses are caused when injured tissue becomes infected. The body's immune system sends white blood cells to help fight off the infection. They begin to fill the damaged tissue, causing pus to build up.